The actual incidence of complications secondary to neuraxial anaesthesia (NA) is unknown, with postdural puncture headache being the most frequent example.1,2 Intracranial subdural haematoma (SDH) is estimated to affect one in 500000 to 1000000 patients undergoing lumbar puncture3 and spinal haematoma is estimated to affect one in 190000 undergoing epidural anaesthesia and one in 320000 undergoing spinal anaesthesia.1 Both complications have been associated with considerable levels of morbidity and mortality3–6; every effort should therefore be made to ensure early diagnosis and treatment.
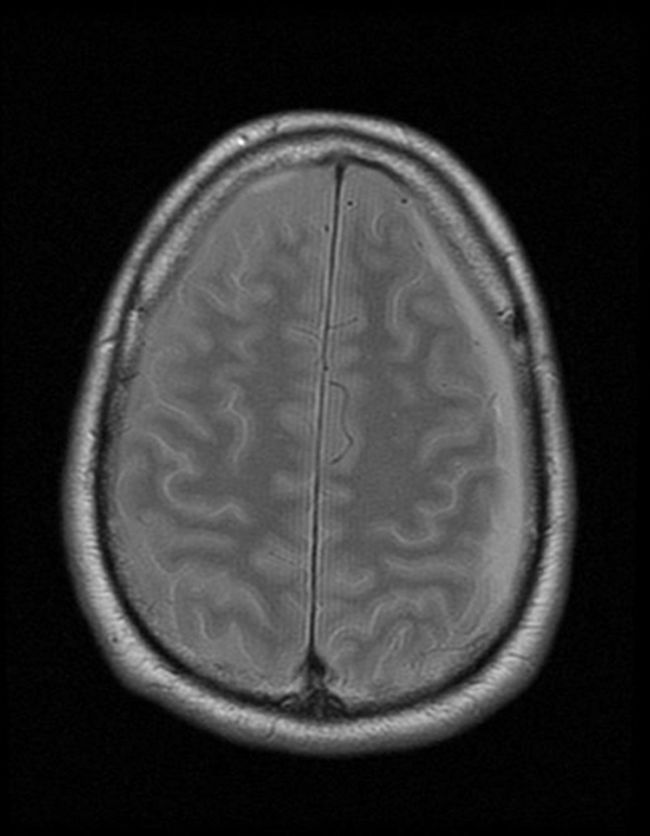
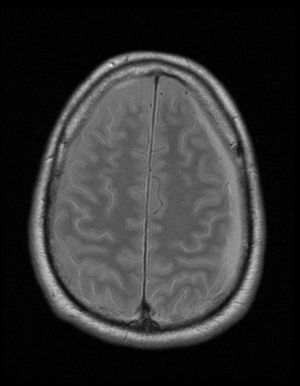
Clinical caseOur patient was a 56-year-old man with no relevant clinical history. Twenty-four hours after undergoing prostate surgery under spinal anaesthesia, he presented intense occipital headache radiating to the neck, triggered by standing. Examination revealed no focal neurological signs. The patient was diagnosed with intracranial hypotension and started on intravenous corticosteroids and nonsteroidal anti-inflammatory drugs. One month after onset, the patient attended our department due to the persistence of symptoms. For 15 days he had experienced constant, pulsatile pain; the intensity had decreased, but pain now also occurred in the supine position, increasing with Valsalva manoeuvres; he had also begun experiencing intense neck pain. A brain MRI scan was performed, revealing an extra-axial collection in the left frontoparietal region, with a maximum thickness of 1cm. It appeared hyperintense on proton density-weighted sequences (Fig. 1) and isointense on T2-weighted sequences. A neck and chest MRI scan showed a posterior subdural space-occupying lesion extending from C7 to T10-T11, appearing with heterogeneous intensity on STIR (Fig. 2), T1-weighted, and gradient echo sequences, and displaying no contrast uptake. The patient was diagnosed with intracranial and spinal SDH, and responded well to conservative treatment.
SDH secondary to NA is caused by reduced CSF volume and pressure, which causes traction on the brain and subdural bridging veins, leading to haemorrhage.2–8
Intracranial SDH after NA is difficult to diagnose, as the main clinical symptom is intense headache, which is also a frequent symptom of intracranial hypotension; the latter must therefore be ruled out before diagnosis of intracranial SDH can be made.2,3 In intracranial SDH, headache may be accompanied by nausea, vomiting, interscapular pain, and focal neurological signs; the condition is differentiated from intracranial hypotension by the fact that pain rarely improves with changes of posture.2,5 Onset usually occurs between 2hours and 44 days after the procedure.3 Pomeranz and colleagues presented a case of intracranial SDH with initially normal brain CT scan results (CT is usually performed following the lumbar puncture) and onset of intracranial SDH 38 days later; this suggests that onset of the condition may be delayed, occurring even several weeks after the lumbar puncture is performed.4 Risk factors for intracranial SDH include puncture technique, needle calibre and insertion angle, undergoing repeated lumbar punctures, female sex, pregnancy, dehydration, arteriovenous malformations, bleeding disorders, and cerebral atrophy.2–8
Spinal haematoma usually presents with intense radicular pain and no sign of infection, and may rapidly progress with motor involvement; the condition usually appears between several hours and 7 days after the NA.1 It is more frequent in patients treated with antiplatelet drugs or heparin and patients with bleeding disorders; however, no risk factor is identified in 30% of cases.7
Early diagnosis is a priority for both conditions in order to begin the appropriate treatment. Treatment for intracranial SDH6 may be conservative or surgical; compressive spinal haematomas, in turn, require emergency decompressive laminectomy.6 In a review of Spanish cases, Castillo et al.9 report that 55% of cases of spinal haematoma required surgical treatment; only 45% could be managed with conservative treatment. If symptoms do not progress in the first hours after the procedure, conservative treatment with close neurological monitoring may be sufficient.9
Please cite this article as: Figueroa Arenas MA, Castañeda Rodríguez LY, Pérez Redondo JC, Uría DF. Hematoma subdural intracraneal y espinal secundario a anestesia neuroaxial. Neurología. 2018;33:476–477.