Our aim is to assess the burden on caregivers of patients with Parkinson's disease (PD) treated with deep brain stimulation (DBS) compared to those caring for patients at advanced stages and undergoing other treatments. We have also assessed the variables associated with presence of caregiver overload.
Material and methodsWe included consecutive patients with PD treated with DBS. Our control group included patients in advanced stages of PD undergoing other treatments. Patients were assessed with the following scales: UPDRS-II, UPDRS-III, UPDRS-IV, Hoehn and Yahr, Schwab & England, Barthel, PDQ-39, MoCA, Apathy Evaluation Scale, HADS, and the abbreviated QUIP. Caregiver burden was evaluated with the Zarit caregiver burden interview and their moods were assessed with the HADS scale.
ResultsWe included 11 patients treated with DBS and 11 with other treatments. For patients treated with DBS, we observed a better quality of life according to the PDQ-39 questionnaire (P=.028), and a lower score on the HADS anxiety subscale (P=.010). Caregiver overload was observed in 54.5% of the caregivers of patients in both groups (P=1.000); Zarit scores were similar (P=.835). Caregiver overload was associated with higher scores on the caregiver's Apathy Evaluation Scale (P=.048) and on the HADS anxiety subscale (P=.006).
ConclusionAccording to our results, treatment with DBS is not associated with lower caregiver burden. Apathy in patients and anxiety in caregivers are factors associated with the appearance of overload.
Nuestro objetivo es determinar el grado de carga de cuidadores de pacientes con enfermedad de Parkinson (EP) en tratamiento con estimulación cerebral profunda (ECP) con respecto a aquellos en estadios avanzados con otros tratamientos y las variables asociadas a la presencia de sobrecarga.
Material y métodosSe incluyeron de forma consecutiva a pacientes con EP en tratamiento con ECP, utilizando como grupo control a otros con EP en estadío avanzado sin ECP. Los pacientes fueron sometidos a una valoración mediante las escalas UPDRS-II, UPDRS-III, UPDRS-IV, Hoehn y Yahr, Schawb & England, Barthel, PDQ-39, MoCA, Apathy Scale, HADS y la QUIP abreviada. A los cuidadores se les estudió mediante el inventario de sobrecarga de Zarit y de valoración afectiva HADS.
ResultadosSe incluyeron 11 pacientes en tratamiento con ECP y 11 con otros tratamientos. En aquellos con ECP se observó una mejor calidad de vida según la escala PDQ-39 (p=0,028), y una menor puntuación en la subescala HADS para la ansiedad (p=0,010). Se observó sobrecarga en un 54,5% de los cuidadores de pacientes de ambos grupos (p=1,000), con una puntuación similar en la escala Zarit (p=0,835). La presencia de sobrecarga se asoció una mayor puntuación en la escala de apatía (p=0,048) y en la subescala HADS de ansiedad en el cuidador (p=0,006).
ConclusiónSegún los resultados de nuestro estudio el tratamiento con ECP no se relaciona con una menor carga del cuidador, siendo la apatía del paciente y la ansiedad del cuidador factores asociados a su desarrollo.
Parkinson's disease (PD) is a neurodegenerative disease causing a series of motor and non-motor symptoms which negatively affect patients’ quality of life.1 As the disease progresses, caregivers become essential to maintaining patients’ quality of life: their presence has been observed to decrease the morbidity and mortality rates of PD patients.2 On many occasions, the caregiver is a close relative, and will experience physical and emotional stress, changes to their everyday socio-economic activities, and, occasionally, overload.
In advanced stages of PD, different treatments have been proven to improve patients’ quality of life3,4; one of these is deep brain stimulation (DBS). However, few studies discuss the effect of this treatment on the overload of PD patients’ caregivers.5,6 Our aim is to compare the degree of caregiver burden in cases of PD patients treated with DBS and patients with advanced PD receiving other treatments, and to identify the variables significantly impacting caregiver burden in these cases.
Material and methodsThis is a cross-sectional observational study. We included consecutive patients treated at the movement disorders unit at Hospital Universitario Miguel Servet, Zaragoza, between September 2014 and July 2015. The study was approved by the Clinical Research Ethics Committee of Aragón.
We included patients with advanced PD who had been receiving treatment with DBS, continuous apomorphine infusion, or continuous intraduodenal levodopa infusion for more than 3 months. We also included patients with motor fluctuations who had previously received continuous apomorphine infusion or continuous intraduodenal levodopa infusion, which since had been suspended. We also included those patients for whom, at the beginning of the study, DBS, apomorphine infusion, or intraduodenal levodopa had been prescribed but had not yet started. All patients must have a main caregiver, defined as the person who lives with the patient and is directly involved in their care or directly affected by the patient's health problem.7 We excluded patients whose main caregiver was a professional or belonged to a social support organisation, patients with moderate or severe cognitive impairment who were unable to understand or autonomously complete the questionnaires, and patients (or their caregivers, when applicable) who did not sign the informed consent form.
We gathered the following demographic data from patients: age, sex, and disease duration. We assessed disease severity with the Unified Parkinson's Disease Rating Scale (UPDRS) subscales II, III, and IV8 and the Hoehn and Yahr,9 Schwab and England,10 and Barthel11 scales. Quality of life was measured with the 39-item Parkinson's Disease Questionnaire (PDQ-39).12 Presence of sleep disorders was assessed using the Scales for Outcomes in PD (SCOPA) Sleep Scale,13 the degree of apathy with the Apathy Scale,14 the presence of mood disorders with the Hospital Anxiety and Depression Scale (HADS),15 cognitive disorders with the Montreal Cognitive Assessment (MoCA),16 and the presence of impulse control disorders with the shortened version of the Questionnaire for Impulsive-Compulsive Disorders in Parkinson's Disease (QUIP).17
Caregivers’ demographic data (age and sex), emotional state (measured with the HADS), and the degree of burden (measured with the Zarit Caregiver Burden Interview) were recorded.18 In the latter scale, values ≥47 were considered to signal overload.
Statistical analysis was performed using the SPSS statistical software, version 15.0. We used measures of central tendency and dispersion in the descriptive analysis, and conducted a bivariate analysis to identify the variables for which the group treated with DBS displayed significant differences with respect to those with other treatments and to determine which variables were associated with caregiver overload. The t test was used to establish the connection between dichotomous qualitative variables and quantitative variables. The Mann–Whitney U test was used when variables were not normally distributed. The chi-square test was used to analyse categorical variables, and the Fisher exact test was used when at least 80% of the expected cell values in the contingency table were ≤5. The correlation study for quantitative variables consisted of the Pearson correlation coefficient for normally distributed variables and the Spearman rank correlation coefficient for non-normally distributed variables. Statistical significance was set at P<.05.
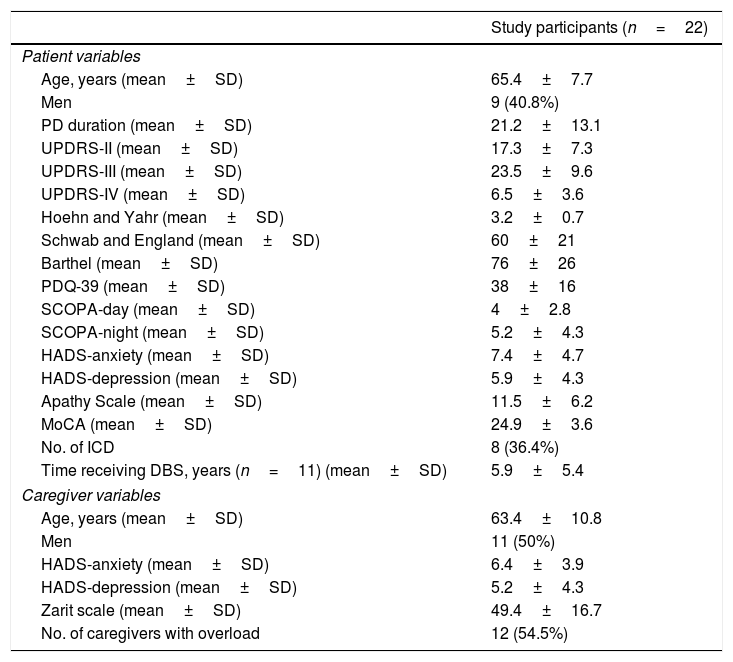
ResultsWe included a total of 22 patients, of whom 11 were treated with DBS, and the remaining 11 with other treatments (3 with apomorphine infusion, one with intraduodenal levodopa infusion, 3 pending DBS treatment, 2 pending apomorphine treatment, and 2 who were intolerant to apomorphine). Twenty caregivers were patients’ partners and 2 were their children. The study population characteristics are listed in Table 1.
Clinical characteristics of patients and caregivers.
| Study participants (n=22) | |
|---|---|
| Patient variables | |
| Age, years (mean±SD) | 65.4±7.7 |
| Men | 9 (40.8%) |
| PD duration (mean±SD) | 21.2±13.1 |
| UPDRS-II (mean±SD) | 17.3±7.3 |
| UPDRS-III (mean±SD) | 23.5±9.6 |
| UPDRS-IV (mean±SD) | 6.5±3.6 |
| Hoehn and Yahr (mean±SD) | 3.2±0.7 |
| Schwab and England (mean±SD) | 60±21 |
| Barthel (mean±SD) | 76±26 |
| PDQ-39 (mean±SD) | 38±16 |
| SCOPA-day (mean±SD) | 4±2.8 |
| SCOPA-night (mean±SD) | 5.2±4.3 |
| HADS-anxiety (mean±SD) | 7.4±4.7 |
| HADS-depression (mean±SD) | 5.9±4.3 |
| Apathy Scale (mean±SD) | 11.5±6.2 |
| MoCA (mean±SD) | 24.9±3.6 |
| No. of ICD | 8 (36.4%) |
| Time receiving DBS, years (n=11) (mean±SD) | 5.9±5.4 |
| Caregiver variables | |
| Age, years (mean±SD) | 63.4±10.8 |
| Men | 11 (50%) |
| HADS-anxiety (mean±SD) | 6.4±3.9 |
| HADS-depression (mean±SD) | 5.2±4.3 |
| Zarit scale (mean±SD) | 49.4±16.7 |
| No. of caregivers with overload | 12 (54.5%) |
SD: standard deviation; ICD: impulse control disorder.
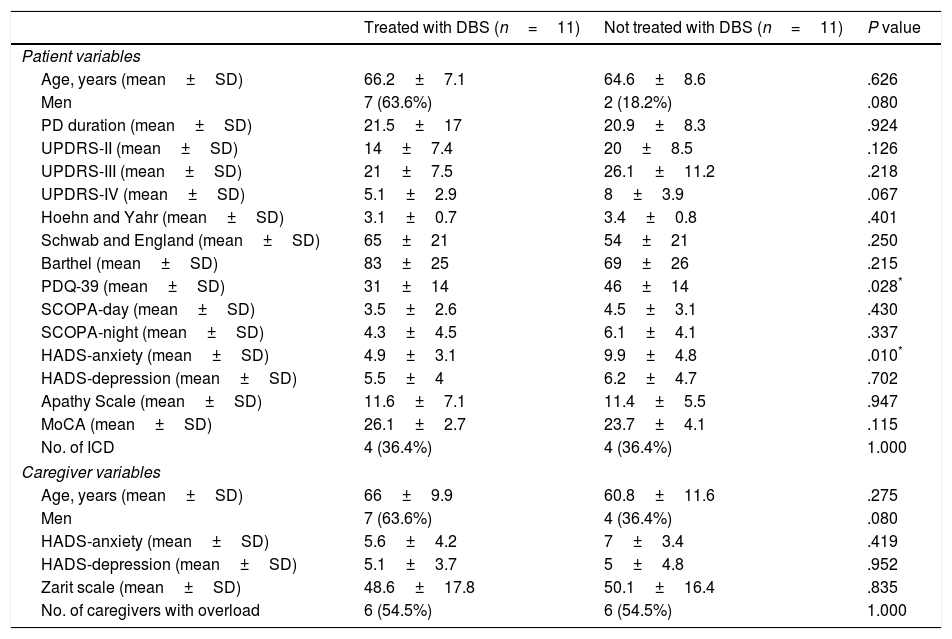
In patients treated with DBS, we observed an improved quality of life according to the PDQ-39 and a lower score on the HADS anxiety subscale, compared to the patients receiving other treatments; no significant differences were found for the remaining variables. We did not observe differences in the variables recorded for the caregivers of patients receiving DBS and patients receiving other treatments. Scores on the Zarit scale were similar and we found the same proportion of caregivers with overload in both groups (Table 2).
Differences according to DBS treatment.
| Treated with DBS (n=11) | Not treated with DBS (n=11) | P value | |
|---|---|---|---|
| Patient variables | |||
| Age, years (mean±SD) | 66.2±7.1 | 64.6±8.6 | .626 |
| Men | 7 (63.6%) | 2 (18.2%) | .080 |
| PD duration (mean±SD) | 21.5±17 | 20.9±8.3 | .924 |
| UPDRS-II (mean±SD) | 14±7.4 | 20±8.5 | .126 |
| UPDRS-III (mean±SD) | 21±7.5 | 26.1±11.2 | .218 |
| UPDRS-IV (mean±SD) | 5.1±2.9 | 8±3.9 | .067 |
| Hoehn and Yahr (mean±SD) | 3.1±0.7 | 3.4±0.8 | .401 |
| Schwab and England (mean±SD) | 65±21 | 54±21 | .250 |
| Barthel (mean±SD) | 83±25 | 69±26 | .215 |
| PDQ-39 (mean±SD) | 31±14 | 46±14 | .028* |
| SCOPA-day (mean±SD) | 3.5±2.6 | 4.5±3.1 | .430 |
| SCOPA-night (mean±SD) | 4.3±4.5 | 6.1±4.1 | .337 |
| HADS-anxiety (mean±SD) | 4.9±3.1 | 9.9±4.8 | .010* |
| HADS-depression (mean±SD) | 5.5±4 | 6.2±4.7 | .702 |
| Apathy Scale (mean±SD) | 11.6±7.1 | 11.4±5.5 | .947 |
| MoCA (mean±SD) | 26.1±2.7 | 23.7±4.1 | .115 |
| No. of ICD | 4 (36.4%) | 4 (36.4%) | 1.000 |
| Caregiver variables | |||
| Age, years (mean±SD) | 66±9.9 | 60.8±11.6 | .275 |
| Men | 7 (63.6%) | 4 (36.4%) | .080 |
| HADS-anxiety (mean±SD) | 5.6±4.2 | 7±3.4 | .419 |
| HADS-depression (mean±SD) | 5.1±3.7 | 5±4.8 | .952 |
| Zarit scale (mean±SD) | 48.6±17.8 | 50.1±16.4 | .835 |
| No. of caregivers with overload | 6 (54.5%) | 6 (54.5%) | 1.000 |
SD: standard deviation; ICD: impulse control disorder.
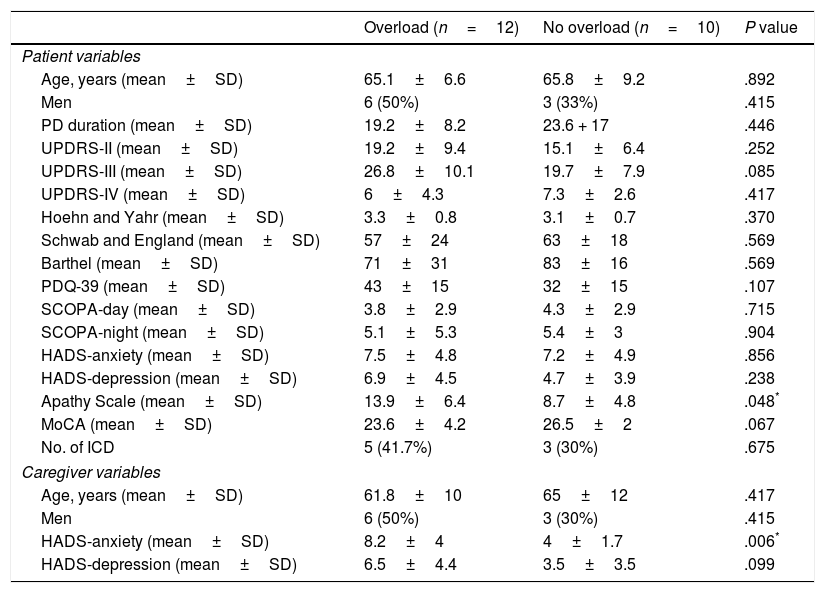
When analysing which variables were related to overload, we only observed that caregivers with overload displayed higher HADS anxiety subscale scores, and that their patients had significantly higher scores on the apathy scale (Table 3). The Zarit scale was significantly correlated with the UPDRS-III (r=0.461; P=.031), PDQ-39 (r=0.432; P=.045), HADS depression subscale (r=0.534; P=.010), and HADS anxiety subscale (r=0.840; P=.000); no significant correlation was observed with the remaining variables.
Differences according to caregiver overload.
| Overload (n=12) | No overload (n=10) | P value | |
|---|---|---|---|
| Patient variables | |||
| Age, years (mean±SD) | 65.1±6.6 | 65.8±9.2 | .892 |
| Men | 6 (50%) | 3 (33%) | .415 |
| PD duration (mean±SD) | 19.2±8.2 | 23.6 + 17 | .446 |
| UPDRS-II (mean±SD) | 19.2±9.4 | 15.1±6.4 | .252 |
| UPDRS-III (mean±SD) | 26.8±10.1 | 19.7±7.9 | .085 |
| UPDRS-IV (mean±SD) | 6±4.3 | 7.3±2.6 | .417 |
| Hoehn and Yahr (mean±SD) | 3.3±0.8 | 3.1±0.7 | .370 |
| Schwab and England (mean±SD) | 57±24 | 63±18 | .569 |
| Barthel (mean±SD) | 71±31 | 83±16 | .569 |
| PDQ-39 (mean±SD) | 43±15 | 32±15 | .107 |
| SCOPA-day (mean±SD) | 3.8±2.9 | 4.3±2.9 | .715 |
| SCOPA-night (mean±SD) | 5.1±5.3 | 5.4±3 | .904 |
| HADS-anxiety (mean±SD) | 7.5±4.8 | 7.2±4.9 | .856 |
| HADS-depression (mean±SD) | 6.9±4.5 | 4.7±3.9 | .238 |
| Apathy Scale (mean±SD) | 13.9±6.4 | 8.7±4.8 | .048* |
| MoCA (mean±SD) | 23.6±4.2 | 26.5±2 | .067 |
| No. of ICD | 5 (41.7%) | 3 (30%) | .675 |
| Caregiver variables | |||
| Age, years (mean±SD) | 61.8±10 | 65±12 | .417 |
| Men | 6 (50%) | 3 (30%) | .415 |
| HADS-anxiety (mean±SD) | 8.2±4 | 4±1.7 | .006* |
| HADS-depression (mean±SD) | 6.5±4.4 | 3.5±3.5 | .099 |
SD: standard deviation; ICD: impulse control disorder.
In this study, despite the better quality of life observed in patients treated with DBS, the degree of burden among the caregivers of these patients was similar to that of caregivers of patients with advanced PD receiving other treatments. These results were similar to those reported by Oyama et al.,5 which showed better quality of life in 275 patients treated with DBS, compared to controls, despite similar degrees of caregiver overload in both groups. Soileau et al.6 prospectively observed that at 6 months after treatment onset, the level of overload experienced by caregivers of 12 patients treated with DBS was not significantly reduced with regards to the baseline situation, despite the improved motor function observed in the patient. These authors suggested that the lack of improvement in patients’ quality of life could be the consequence of the short follow-up period, during which patients and caregivers probably would not yet have adapted to the new situation.
Overload in caregivers of patients with PD has been related to factors associated with the patients themselves, such as the degree of disability and disease severity, quality of life, and the presence of mood disorders, sleep disorders, and non-motor symptoms; and to factors related to the caregivers, such as their quality of life and emotional state.7,19–22 In our study, the presence of overload was significantly correlated with a higher score on the apathy scale; apathy is a non-motor symptom which can even be exacerbated after DBS treatment onset as a consequence of the need for lower doses of levodopa and dopaminergic agonists.23 The other variable associated with caregiver overload was a higher score for caregiver anxiety on the HADS, with a strong correlation being observable between this scale and Zarit scale scores. The directionality of this relationship is difficult to interpret with the study data, but is probably bidirectional. Caregiver anxiety may be expressed as overload, and overload, in turn, could probably increase caregivers’ anxiety levels.
Considering this anxiety-overload relationship, it is necessary to identify caregivers’ stress factors to decrease their level of anxiety. When overload is identified in a caregiver, we should assess the possibility of a psychotherapeutic intervention to assess the presence of anxiety, and to treat this, if present.
Treatment with DBS requires frequent medical consultations and repeated changes to medication and stimulator programming, which both the patient and the caregiver should understand. Furthermore, throughout the course of the disease, the patient with PD assumes the role of the sick person and establishes a physical and emotional dependence on the caregiver. With the improved motor function and quality of life of the patient treated with DBS, this relationship of dependence should change, improve, and translate into reduced caregiver overload. However, neither our results nor those of other studies support this.5,6 We should try to identify the factors contributing to this situation, since the aim of advanced therapy in patients with PD is to improve not only their quality of life but also, in parallel, that of the caregivers (partners or children) involved in the process of the disease.
The main limitations of our study were the small sample size and its cross-sectional design. Further prospective studies with larger samples are necessary to identify the factors causing overload to the caregivers of patients treated with DBS.
FundingThis study received no public or private financial support.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Crespo-Burillo JA, Rivero-Celada D, Saenz-de Cabezón A, Casado-Pellejero J, Alberdi-Viñas J, Alarcia-Alejos R. Influencia de la estimulación cerebral profunda en la carga de cuidadores de pacientes con enfermedad de Parkinson. Neurología. 2018;33:154–159.
Results from this study were presented at the 67th Annual Meeting of the Spanish Society of Neurology.