To describe the sociodemographic and clinical characteristics of a cohort of patients with epilepsy from a reference centre in Colombia.
MethodsCross-sectional study including patients diagnosed with epilepsy who attended our epilepsy centre (Neurocentro) between 2013 and 2016. Data were gathered from patients’ medical histories.
ResultsWe gathered data from a total of 354 patients diagnosed with epilepsy. Median age was 37 years; 52% were men. Seizures were focal in 57% of the patients and generalised in 38%; seizure type was not determined in 6% of the sample. The most frequent aetiology was cryptogenic (21%), followed by traumatic (14%). Median time of disease progression and age at onset were 23 and 11 years, respectively. Psychiatric comorbidities were found in 18% of the patients and 40% had some degree of cognitive impairment. Around 40% of our sample reported adverse reactions to antiepileptic drugs at some point during treatment. Antiepileptic drugs were administered in monotherapy in 36% of the patients. Around 37% had drug-resistant epilepsy and 14% underwent surgery.
ConclusionsPsychiatric comorbidities, cognitive impairment, adverse drug reactions, and drug-resistant epilepsy are common among epileptic patients in Colombia. Knowledge of the factors with an impact on epilepsy may lay the foundations for improving management of these patients on the administrative level and improving quality of life.
Describir las características clínicas y sociodemográficas de pacientes con epilepsia de un centro de referencia de Colombia.
MétodosEstudio de corte transversal. Se incluyó a los pacientes con diagnóstico de epilepsia que acudieron al centro de epilepsia Neurocentro en el período comprendido entre los años 2013 y 2016. La información se obtuvo de las historias clínicas.
ResultadosSe estudió a 354 pacientes con diagnóstico de epilepsia. La mediana de edad fue de 37 años y el 52% eran hombres. El 57% presentó crisis de tipo focales, el 38% de tipo generalizada y 6% sin clasificar. La etiología más prevalente fue la criptogénica (21%) seguida de la traumática (14%). La mediana de tiempo de evolución de la epilepsia y de inicio de las crisis fue de 23 años y 11 años, respectivamente. La comorbilidad psiquiátrica se encontró en el 18% de los pacientes. El 40% presentó algún grado de deterioro cognitivo y la misma proporción refirió efectos adversos a los antiepilépticos en algún momento durante su tratamiento. El manejo farmacológico con antiepilépticos en monoterapia se presentó en el 36%. La farmacorresistencia fue hallada en 37% de los estudiados. Se realizó intervención quirúrgica en el 14% del total de pacientes.
ConclusionesObservamos que la comorbilidad psiquiátrica, el deterioro cognitivo, las reacciones adversas a los antiepilépticos y la farmacorresistencia son frecuentes entre los pacientes epilépticos en Colombia. Esperamos que este estudio sirva como soporte para lograr una legislación en salud más integral que mejore la calidad de vida de estos pacientes teniendo en cuenta todas las variables que influyen en la enfermedad.
Epilepsy is one of the most common neurological diseases, affecting over 50 million people worldwide; 80% of patients are from developing regions.1,2 Around 5 million people in Latin America and the Caribbean are estimated to have epilepsy.3 The prevalence of epilepsy in Colombia is estimated at 11.3 cases per 1000 population.4
The International League Against Epilepsy (ILAE) defines the condition as a disorder of the brain characterised by an enduring predisposition to generate abnormal electrical activity, called epileptic seizures, with considerable neurobiological, cognitive, psychological, and social consequences.5,6 Most patients have focal seizures, which commonly progress to generalised seizures1,4; in most cases, the aetiology is unknown,1 which considerably limits treatment and clinical prognosis.
Seizures can be managed by pharmacological treatment in up to 70% of patients; in Latin America, however, nearly 60% of patients either are not diagnosed or do not receive treatment due to lack of availability or high costs.7,8 Some patients respond poorly to antiepileptic drugs (AED) and require other treatment approaches, including surgery.9–11 Other deleterious consequences of epilepsy include trauma during seizures, adverse reactions to AEDs, and cognitive impairment due to status epilepticus.12
Several studies with small samples or considering a limited number of clinical variables have been conducted in Colombia.13–19 Ours is the epilepsy study with the largest patient sample to be conducted in the country. We describe the clinical and sociodemographic characteristics of a population of patients with epilepsy from a reference centre in Pereira, Colombia.
Patients and methodsPatients and type of studyWe conducted a cross-sectional study of patients diagnosed with epilepsy and attending the Neurocentro institute for epilepsy and Parkinson's disease between January 2013 and the first trimester of 2016. Neurocentro is the only institution specialising in epilepsy treatment in the Colombian Coffee Triangle. In order to be included in the study, patients had to: 1) be older than 16, 2) have a diagnosis of epilepsy based on the ILAE diagnostic criteria5; 3) have a complete clinical history (both patients attending the institute for the first time and patients previously diagnosed with epilepsy and attending a follow-up consultation); and 4) be assessed by an epilepsy specialist. The only exclusion criterion was presence of non-epileptic seizures during video-EEG. All patients were evaluated by a team of clinical neurologists and an epilepsy specialist, and where necessary by psychiatrists, neuropsychologists, and a functional neurosurgeon.
Clinical histories were obtained from the eOfiClinic digital database; data were filtered to identify patients diagnosed with epilepsy. We subsequently analysed each clinical history and identified those patients meeting the inclusion criteria. Data were gathered on the following variables:
- –
Sociodemographic variables: age, sex, area of residence (urban or rural), years of schooling, and employment status.
- –
Clinical and surgery variables: triggering factors, family history of epilepsy, history of status epilepticus, type of seizures according to the 2010 ILAE classification,20 aetiology (vascular, idiopathic, metabolic, autoimmune, mixed, tumour, infection, trauma, neuronal migration disorder, mesial temporal sclerosis, perinatal hypoxia, etc.), presence of aura, time of seizure occurrence (during sleep, awake, or both), longest interictal period, age at epilepsy onset, association with moon phases, cognitive impairment, neurological examination results (normal or pathological), complementary test results, neuropsychological assessment results, epilepsy surgery (lobectomy, corpus callosotomy, hemispherectomy, amygdalohippocampectomy, lesionectomy, or deep brain stimulation), and any associated comorbidities.
- –
Pharmacological variables: AEDs currently used, adverse reactions to AEDs, drug resistance (according to the ILAE criteria21), and concomitant medications.
The type of epilepsy was established based on clinical characteristics and diagnostic test results. Some of the study’s strengths are its large sample size, the wide range of variables studied, and the small likelihood of information bias due to the high standards for information management followed by clinical professionals. One limitation is the selection bias: 1) most patients were adults, and no paediatric patients were included; and 2) data were gathered from a reference centre. We also did not calculate a sample size that would enable us to extrapolate our results to the general population.
Statistical analysisFor continuous variables, data are presented as means, medians, and interquartile ranges, according to whether the variable followed a normal distribution. Qualitative variables are expressed as absolute frequencies and percentages. Data were analysed with the STATA statistical software, version 14.
Our study was approved by Neurocentro's bioethics committee as “research with no risk” according to Resolution no. 008430/1993 of the Colombian Ministry of Health, and complies with the principles of the Declaration of Helsinki.
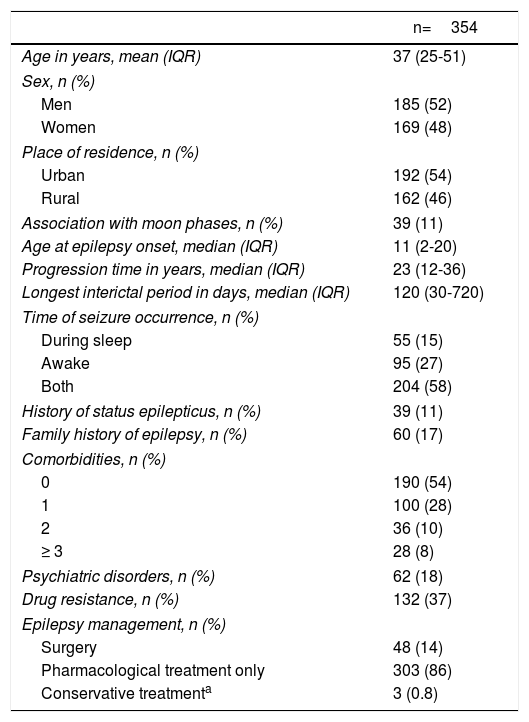
ResultsWe identified 366 patients; 12 had non-epileptic seizures and were therefore excluded, leaving a total of 354 patients. The median age at epilepsy onset was 11 years (range, 1 month to 91 years) (Table 1).
Patient demographic and clinical characteristics.
| n=354 | |
|---|---|
| Age in years, mean (IQR) | 37 (25-51) |
| Sex, n (%) | |
| Men | 185 (52) |
| Women | 169 (48) |
| Place of residence, n (%) | |
| Urban | 192 (54) |
| Rural | 162 (46) |
| Association with moon phases, n (%) | 39 (11) |
| Age at epilepsy onset, median (IQR) | 11 (2-20) |
| Progression time in years, median (IQR) | 23 (12-36) |
| Longest interictal period in days, median (IQR) | 120 (30-720) |
| Time of seizure occurrence, n (%) | |
| During sleep | 55 (15) |
| Awake | 95 (27) |
| Both | 204 (58) |
| History of status epilepticus, n (%) | 39 (11) |
| Family history of epilepsy, n (%) | 60 (17) |
| Comorbidities, n (%) | |
| 0 | 190 (54) |
| 1 | 100 (28) |
| 2 | 36 (10) |
| ≥ 3 | 28 (8) |
| Psychiatric disorders, n (%) | 62 (18) |
| Drug resistance, n (%) | 132 (37) |
| Epilepsy management, n (%) | |
| Surgery | 48 (14) |
| Pharmacological treatment only | 303 (86) |
| Conservative treatmenta | 3 (0.8) |
IQR: interquartile range.
Seven patients (2%) had ictal pain and 95 (27%) reported experiencing some type of aura. Most patients (240; 68%) reported no trigger factors during the initial consultation. Some of the trigger factors reported by the remaining patients were stress (18 patients; 5%), sleep deprivation (19; 5%), treatment non-adherence (15; 4%), the menstrual cycle (15; 4%), infections (7; 2%), alcohol consumption (2; 0.6%), lights or light artefacts (2; 0.6%), exercise (2; 0.6%), fatigue (1; 0.3%), a combination of these factors (22; 6%), and other trigger factors (11; 3%). Thirty-nine patients (11%) reported an association between seizures and moon phases.
The neurological examination revealed alterations in 125 patients (35.3%). A neuropsychological assessment was conducted in 106 patients (30%), in most cases to decide on the most suitable surgical approach. Cognitive alterations were identified in 140 patients (40%) through standardised neuropsychological tests and psychiatric consultations; these were mild in 72 patients (20%), moderate in 37 (11%), and severe in 31 (9%).
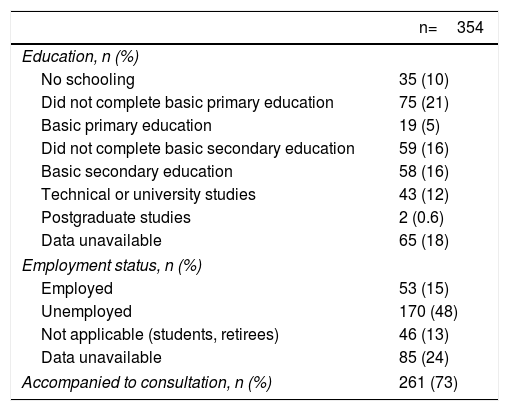
Ten percent of patients had not attended school and only 12.6% had university studies. The unemployment rate in our sample was 48% (Table 2).
Patient social characteristics.
| n=354 | |
|---|---|
| Education, n (%) | |
| No schooling | 35 (10) |
| Did not complete basic primary education | 75 (21) |
| Basic primary education | 19 (5) |
| Did not complete basic secondary education | 59 (16) |
| Basic secondary education | 58 (16) |
| Technical or university studies | 43 (12) |
| Postgraduate studies | 2 (0.6) |
| Data unavailable | 65 (18) |
| Employment status, n (%) | |
| Employed | 53 (15) |
| Unemployed | 170 (48) |
| Not applicable (students, retirees) | 46 (13) |
| Data unavailable | 85 (24) |
| Accompanied to consultation, n (%) | 261 (73) |
According to the clinical histories, 8 patients (2.3%) had undergone EEG only; 12 (4%) video-EEG only; 6 (1.7%) CT only; 7 (2%) MRI only; 12 (4%) EEG plus video-EEG; 141 (40%) were evaluated with EEG, video-EEG, and MRI; 54 (15%) all 4 studies; and 33 (9%) EEG plus MRI but not video-EEG.
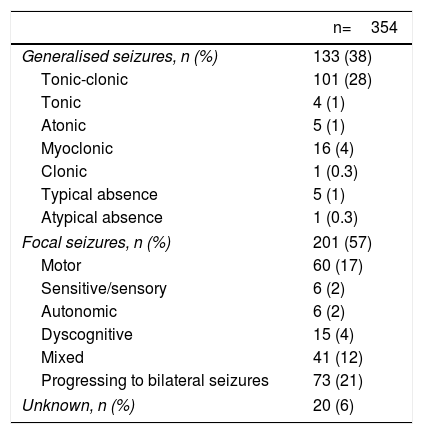
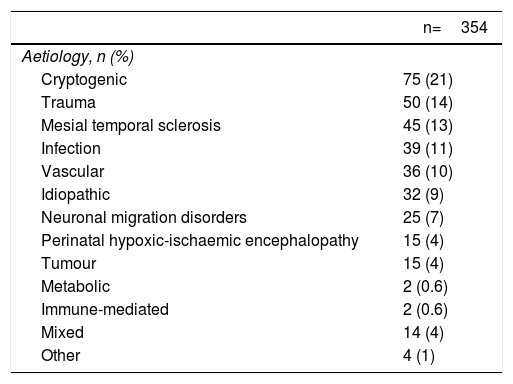
The most frequent aetiology was cryptogenic. Regarding seizure type, 201 (57%) had focal epilepsy, 133 (38%) had generalised epilepsy, and 20 (6%) had unclassified epilepsy (Tables 3 and 4).
Types of epileptic seizures in the sample.
| n=354 | |
|---|---|
| Generalised seizures, n (%) | 133 (38) |
| Tonic-clonic | 101 (28) |
| Tonic | 4 (1) |
| Atonic | 5 (1) |
| Myoclonic | 16 (4) |
| Clonic | 1 (0.3) |
| Typical absence | 5 (1) |
| Atypical absence | 1 (0.3) |
| Focal seizures, n (%) | 201 (57) |
| Motor | 60 (17) |
| Sensitive/sensory | 6 (2) |
| Autonomic | 6 (2) |
| Dyscognitive | 15 (4) |
| Mixed | 41 (12) |
| Progressing to bilateral seizures | 73 (21) |
| Unknown, n (%) | 20 (6) |
Epilepsy aetiology.
| n=354 | |
|---|---|
| Aetiology, n (%) | |
| Cryptogenic | 75 (21) |
| Trauma | 50 (14) |
| Mesial temporal sclerosis | 45 (13) |
| Infection | 39 (11) |
| Vascular | 36 (10) |
| Idiopathic | 32 (9) |
| Neuronal migration disorders | 25 (7) |
| Perinatal hypoxic-ischaemic encephalopathy | 15 (4) |
| Tumour | 15 (4) |
| Metabolic | 2 (0.6) |
| Immune-mediated | 2 (0.6) |
| Mixed | 14 (4) |
| Other | 4 (1) |
Comorbidities were recorded for 164 patients (46%); 28 patients (8%) had 3 or more comorbidities. Psychiatric comorbidities were the most frequent (in 62 patients; 18%), followed by neurological diseases (46; 13%), cardiovascular diseases (27; 7.6%), endocrine disorders (25; 7%), infections (8; 2.2%), bone and muscle disorders (7; 2%), haematological diseases (1; 0.3%), and kidney diseases (1; 0.3%).
The most frequent neurological disorders were cerebrovascular accident (12 patients; 3.7%), migraine (6; 1.7%), head trauma (6; 1.7%), and cerebral palsy (4; 1.1%). The most frequent cardiovascular conditions were arterial hypertension (16; 4.5%) and ischaemic heart disease (5; 1.4%). The most common endocrine disorders were thyroid disorders (13; 3.6%), type 2 diabetes mellitus (5; 1.4%), and dyslipidaemia (3; 0.8%).
The most frequent psychiatric disorders were depression (28; 8%), organic mental disorders (18; 5%), aggressiveness (6; 1.7%), schizophrenia (4; 1%), bipolar affective disorder (4; 1%), generalised anxiety disorder (3; 0.8%), and attention-deficit/hyperactivity disorder (1; 0.3%). Four patients (1.1%) had anxiety and depression, and 3 patients showed psychotic symptoms in addition to anxiety and depression. No patients had personality disorders or obsessive-compulsive disorder.
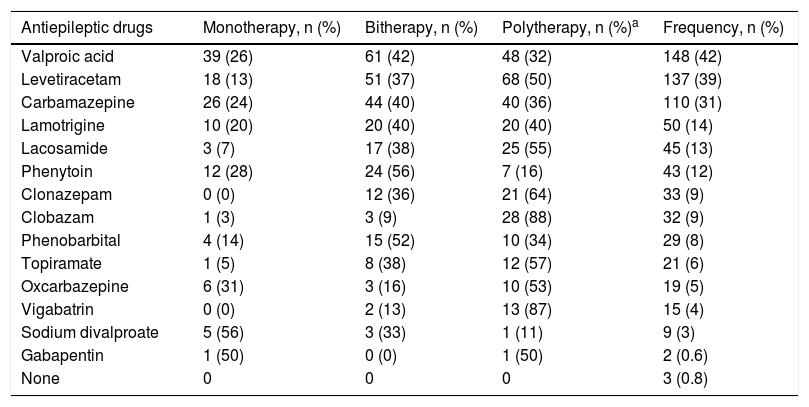
Pharmacological and surgical treatmentsAEDs were used in monotherapy in 126 patients (36%); 132 patients (37%) received 2 AEDs, 72 (20%) received 3, 15 (4%) received 4, and 6 (1.7%) received 5. Thirty-nine patients (11%) received one concomitant medication, 12 (3.5%) received 2, 7 (2%) received 3, 4 (1.2%) received 4, and 8 (2.4%) received 5 or more concomitant medications. The most frequent AED was valproic acid (Table 5). Adverse reactions to AEDs were reported at some point during treatment in 140 patients (40%).
Antiepileptic drugs used in the 354 patients studied.
| Antiepileptic drugs | Monotherapy, n (%) | Bitherapy, n (%) | Polytherapy, n (%)a | Frequency, n (%) |
|---|---|---|---|---|
| Valproic acid | 39 (26) | 61 (42) | 48 (32) | 148 (42) |
| Levetiracetam | 18 (13) | 51 (37) | 68 (50) | 137 (39) |
| Carbamazepine | 26 (24) | 44 (40) | 40 (36) | 110 (31) |
| Lamotrigine | 10 (20) | 20 (40) | 20 (40) | 50 (14) |
| Lacosamide | 3 (7) | 17 (38) | 25 (55) | 45 (13) |
| Phenytoin | 12 (28) | 24 (56) | 7 (16) | 43 (12) |
| Clonazepam | 0 (0) | 12 (36) | 21 (64) | 33 (9) |
| Clobazam | 1 (3) | 3 (9) | 28 (88) | 32 (9) |
| Phenobarbital | 4 (14) | 15 (52) | 10 (34) | 29 (8) |
| Topiramate | 1 (5) | 8 (38) | 12 (57) | 21 (6) |
| Oxcarbazepine | 6 (31) | 3 (16) | 10 (53) | 19 (5) |
| Vigabatrin | 0 (0) | 2 (13) | 13 (87) | 15 (4) |
| Sodium divalproate | 5 (56) | 3 (33) | 1 (11) | 9 (3) |
| Gabapentin | 1 (50) | 0 (0) | 1 (50) | 2 (0.6) |
| None | 0 | 0 | 0 | 3 (0.8) |
Forty-eight patients underwent surgery: temporal lobectomy in 5 patients (10%), corpus callosotomy in 5 (10%), amygdalohippocampectomy in 8 (16%), lesionectomy in 11 (23%), vagus nerve stimulation in 4 (8%), hippocampal deep brain stimulation in 4 (8%), hemispherectomy in 3 (6%), other lobectomies in 3 (6%), tumour resection in 4 (8%), and frontal pericystectomy with subpial transection of the eloquent area and temporal lobectomy in one (2%).
DiscussionEpilepsy has numerous consequences for patients’ quality of life, healthcare systems, and society. In our setting, epilepsy has a prevalence of 11.3 cases per 1000 population,4 and poses a major challenge for healthcare professionals and public health. Our sample mainly includes adult patients with long disease progression times (first seizures occurring during adolescence), short interictal periods, and numerous comorbidities, particularly psychiatric disorders.
Regarding epilepsy type, 57% of patients had focal seizures and 38% had generalised seizures. In a series of Spanish patients with epilepsy, focal seizures were observed in 73% and generalised seizures in 19.5%.22 In a Chilean study, 55% of patients had focal epilepsy and 40% had generalised epilepsy.23 In Colombia, Vélez and Eslava-Cobos4 report partial seizures in 80% of the sample and generalised seizures in 12%. The most recent study conducted in Bogotá reported focal seizures in 77.2% of patients and generalised seizures in 22.6%.17 The epidemiology of epileptic seizures depends on a wide range of clinical, healthcare, sociodemographic, and technical factors that make it challenging to estimate the frequency of each type of seizure; in any case, most published studies agree that focal seizures are more frequent than generalised seizures.
In our sample, the most frequent aetiology was cryptogenic (21% of patients), followed by trauma (14%); in the study by Torres-Ferrús et al.,22 in contrast, the most common aetiology was vascular (33.8%), whereas trauma was only observed in 10% of patients. The study conducted in Bogotá identified structural and/or metabolic causes in 47.6% of patients, while the aetiology of epilepsy was unknown in 45.7% of patients.17 We are limited to describing aetiology, as these studies use different classification systems, sample sizes, and diagnostic criteria. The association between epileptic seizures and moon phases has previously been reported in 34% of epileptic patients, particularly during full-moon days.24 In our study, however, only 11% of patients reported this association. Several hypotheses have attempted to explain this phenomenon, which may have clinical relevance.
The REST-1 group25 studied a sample of epileptic patients from 7 European countries and found that patients were more likely than controls to be unemployed and unmarried. Only 13% of the patients in that study had university studies; this rate is similar to that observed in our sample (12.6%). In our sample, 48% of patients were unemployed; similar rates are reported in high-income countries and in other studies also conducted in Colombia, such as the one by Espinosa Jovel et al.,17 who found an unemployment rate of 76.7% in a low-income population from Bogotá. Other studies conducted in the Netherlands26 and Britain27 report unemployment rates of nearly 50%. According to Marinas et al.28 these high unemployment rates are directly associated with other variables, including education level, polytherapy, drug resistance, and occurrence of epileptic seizures in the previous 12 months.
Our sample showed a high rate of comorbidities (46%); this finding is consistent with the results of several epidemiological studies reporting higher prevalence of common chronic diseases in patients with epilepsy than in unaffected individuals.29 Like in other published studies, psychiatric disorders were frequent in our sample (18%).30
Previous studies of Colombian populations have shown that the great majority of patients are treated with valproic acid.18,19 Although the drug is indicated for epilepsy, it is not the first-line treatment for focal or generalised seizures in adults according to the ILAE.31 According to our results, although valproic acid has a broad spectrum of action, it was prescribed in monotherapy in only 7 out of 70 patients with focal seizures receiving the drug. Use of valproic acid for focal epilepsy was greater in bitherapy (35 patients) and polytherapy (28 patients): the drug's efficacy increases when it is combined with levetiracetam, carbamazepine, lacosamide, or lamotrigine, as combination therapy involves different action mechanisms.32,33
In our study, the drugs most frequently prescribed in monotherapy were valproic acid, carbamazepine, levetiracetam, phenytoin, and lamotrigine, as reported in other countries20,34–36; this is explained by their greater ability to control focal and generalised seizures and their good safety profiles. This increase in the use of levetiracetam may also be linked to its recent inclusion in the Colombian healthcare service's drug list for patients with drug-resistant epilepsy, avoiding the need for additional paperwork in order to dispense the drug.19
Monotherapy is generally recommended for patients with a recent diagnosis of epilepsy, with an initial effectiveness of around 50%.37–39 In our study, 36% of patients received monotherapy; this rate is lower than those reported by other studies.34,35,40 However, one previous study reported a similar rate (41%).19 This may be explained by the fact that Neurocentro is a reference centre for epilepsy in our region and receives more complex cases, associated with longer progression times and more comorbidities and adverse drug reactions.
Polymedication was less frequent in our sample (19.7%) than in previous Colombian studies into AED prescription.18,19 These differences may be due to the fact that these studies included different Colombian populations (including patients with diseases other than epilepsy) and used a database from a pharmaceutical distributor; these data are therefore not comparable to our own. Further research should be conducted to study this variable.
Polytherapy was frequent, increasing the risk of adverse events and drug-drug interactions.33 In our study, 40% of patients showed adverse drug reactions, a higher rate than that recently reported in Colombia.19 Similar rates have also been reported in other studies.41 We should highlight the great rigour with which clinical histories were completed, enabling us to choose drugs potentially effective for epilepsy management, thereby avoiding the prescription of multiple drugs.
According to the literature, drug-resistant epilepsy accounts for 15.6%42 to 25% of patients,43 whereas our study reports a rate of 37%. The exact prevalence of AED resistance is difficult to determine due to the different criteria established to define this concept. There is great concern about which factors are increasing AED resistance, considering that Neurocentro is the only reference centre in the region and therefore provides care to the most complex, refractory cases.
A large proportion (14%) of our patients underwent epilepsy surgery; a much lower rate is reported in the literature (1.2%).44 This may be explained by the fact that our reference centre performs individualised patient examinations, including an assessment of whether patients may benefit from surgery, where appropriate, whereas in other countries mean time from diagnosis to surgery may reach 20 years.45
ConclusionOur study analyses the clinical and sociodemographic characteristics of a sample of patients with epilepsy from the Colombian Coffee Triangle. Most patients were of working age and had long progression times, with epilepsy onset usually occurring during childhood. We also identified such other features as low level of schooling, unemployment, polytherapy, and multiple comorbidities; further research should address the influence of these factors on patients’ quality of life and social life.
Strikingly, nearly half of our patients presented adverse drug reactions, and a large percentage had drug-resistant epilepsy. Only 14% underwent epilepsy surgery. We should highlight the high prevalence of cognitive impairment, psychiatric disorders, and other comorbidities among patients in the Colombian Coffee Triangle; this should be considered in future studies.
Further research should be conducted in Colombia and in our region to determine the clinical, aetiological, pharmacological, and social characteristics of epilepsy patients in order to develop policies aimed at improving these patients’ quality of life.
FundingThis study has received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
To the Neurocentro institute for epilepsy and Parkinson's disease of the Colombian Coffee Triangle, for their support to this study. To Paula Andrea Moreno-Gutiérrez MD (Uppsala University), for her assistance with the English-language version of the abstract.
Please cite this article as: Orozco-Hernández JP, Quintero-Moreno JF, Marín-Medina DS, Castaño-Montoya JP, Hernández-Coral P, Pineda M, et al. Perfil clínico y sociodemográfico de la epilepsia en adultos de un centro de referencia de Colombia. Neurología. 2019;34:437–444.