We present the case of a 74-year-old woman with no relevant history who visited the emergency department due to a 2-week history of progressive symptoms of behavioural alterations associated with asthenia and hyporexia. She was initially seen by psychiatrists and was diagnosed with depressive disorder, which was treated with desvenlafaxine at 50mg/day. Two weeks later, symptoms intensified and she returned to the emergency department, where she was administered haloperidol intravenously; mechanical restraint was used due to psychomotor agitation.
The patient was admitted for examination and sedative medication was suspended; during the neurological examination, the patient presented stupor and could only utter incoherent phrases when strongly stimulated. No other significant alterations were observed.
A complete blood count, coagulation study, kidney and liver function studies, total protein test, thyroid hormone measurement, rheumatoid factor tests, antineuronal and anti-thyroid antibody studies, tumour markers, urine sediment, and serology test for HIV and syphilis all returned negative results.
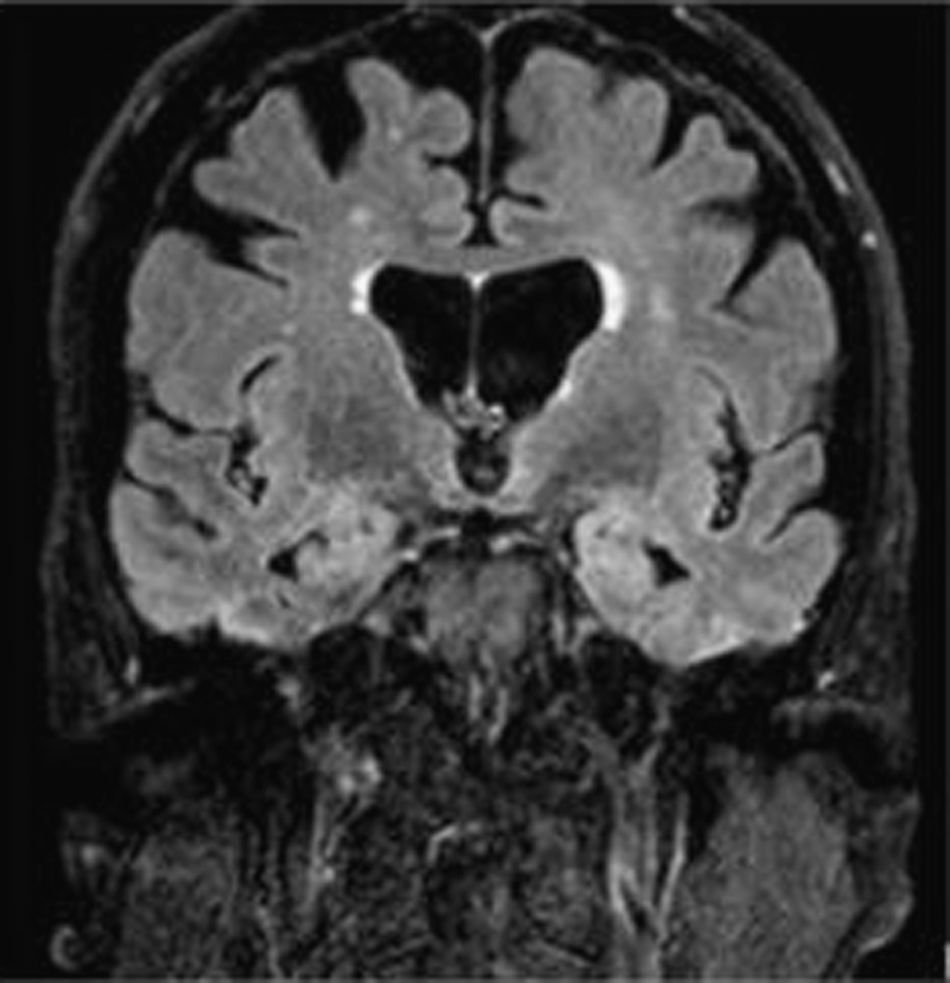
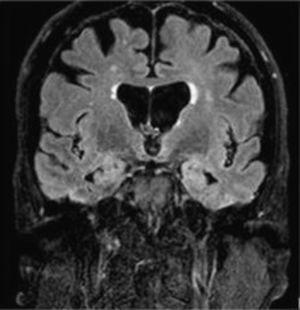
The cerebrospinal fluid study showed no cellularity, with protein and glucose levels within normal ranges. A brain MRI scan (FLAIR) (Fig. 1) revealed a bilateral medial temporal hyperintensity, predominantly on the left side. Chest, abdomen, and pelvis CT (Fig. 2) showed a peripancreatic tumour, for which differential diagnosis between adenocarcinoma and lymphoma was considered due to its appearance.
Given suspicion of paraneoplastic limbic encephalitis,1–3 we started treatment with immunoglobulins dosed at 0.4g/kg/day.4 A subsequent screening for onconeural antibodies in the cerebrospinal fluid yielded positive results for NMDA-receptor antibodies. The anatomical pathology study confirmed small-cell neuroendocrine carcinoma of the pancreas, with a proliferation index of 70%. Given the lack of response to the initial treatment, we decided to administer rituximab,4 which improved the patient's level of consciousness and cognitive processing in the following weeks.
The tumour was localised (T3), did not invade adjacent organs, and was not associated with adenopathy. First-line treatment with carboplatin and etoposide achieved partial response after 6 cycles, with significant cognitive improvement after the first 2 cycles. However, after local radiotherapy and 4 lines of chemotherapy, the patient presented local, ganglion, and metastatic recurrence at 6 months, and died 18 months after diagnosis.
Anti-NMDA receptor encephalitis clinically manifests with subacute symptoms of behaviour disorders, choreic movements, seizures, and autonomic dysfunction. It classically occurs in young women and children; approximately half of all cases are associated with tumours, mainly ovarian teratoma.3 Manifestation in patients older than 45 is unusual and features a more prominent psychiatric component; therefore, diagnosis is a challenge. Since its first description by Dalmau et al.,1 in 2007, the condition has been associated with different tumours, including breast cancer, neuroendocrine tumours, pancreatic cancer, gonadal tumours, and small-cell lung cancer. This is the first case of undifferentiated neuroendocrine pancreatic tumour associated with anti-NMDA receptor antibodies to be published in the literature.5
Please cite this article as: García-Ull J, Cañizares-Ledo E, Gómez-Martínez J, Gómez IV, Masegosa AG. Encefalitis anti-NMDA en mujer anciana. A propósito de un caso. Neurología. 2018;33:482–483.
This study was presented in poster format at the 33rd Annual Meeting of the Valencian Society of Neurology.