Minimally invasive techniques have become the gold standard for a number of surgical procedures. The benefits include a decrease in morbidity, reducing the length of hospital stay and a faster return to daily activities.
Material and methodsAn experimental, longitudinal, comparative, prospective, non-blinded study. A training program of 4 weeks’ duration was carried out with an experimental group of first and second year General Surgery residents and social service medical interns (group A); at the end of the training there was a test, where a series of exercises compared the residents who took the training program with a control group (group B) composed of residents from the fourth and fifth year who did not take this training.
ResultsUpon analyzing the two groups, we observed a decrease in the average time by group A compared to group B. Overall, the 7 exercises show a difference in average time, with group A completing them in 5min compared to group B's 12min (p<0.05).
DiscussionThis study shows that training in a physical simulator for laparoscopic surgery, for at least two hours a week for a month, is sufficient to improve laparoscopic surgical skills, reducing turnaround times by more than half compared to those who did not undergo this training.
Minimally invasive techniques have become the gold standard for a number of surgical procedures. Benefits include a drop in morbidity, thus reducing hospital stay, and a faster return to everyday activities.1
The term “learning curve” was introduced in surgery to make a reference to the number of surgeries that a surgeon must perform in order to reach a level of experience with a low incidence of the range of complications. Depending on the type of surgery, between 15 and 100 procedures are required to reach the learning curve plateau. Even experienced laparoscopic surgeons have to go through the learning curve again when they train for new laparoscopic techniques or instruments.2
For a long time, surgical teaching and training has been based on a teacher–student model, applied mainly in the operating room. In recent years, however, there have been major changes in surgery. Additionally, the available time for residents in their first years has shortened, and new surgical techniques have emerged. These new techniques lead to new and significant demands in surgical teaching and training, resulting in new methods to acquire experience and skills.
The use of a visual feedback base in monitors or other types of screens gives laparoscopy a wide range of teaching and training possibilities based on computing systems.3
Intracorporeal knot-tying and suturing is amongst the most difficult tasks in laparoscopy, involving hand-eye coordination skills and knowledge of the proper steps. Proficiency in laparoscopic sutures is an important requirement for surgeons who wish to conduct advanced laparoscopy.4 A non-randomized study showed a significant improvement in intracorporeal suturing by acquiring skills training in a laparoscopic training box.5
There are virtual reality simulators or laparoscopic training boxes used for training,6 whose objective is the development of the necessary skills and understanding of the spatial-temporal frame of reference and required maneuvering to manipulate instruments and tissue in a bi-dimensional vision, camera manipulation and the ability to control instruments with both hands; thus being able to perform complicated surgical procedures with minimal invasion.7–9
The objective of this study is to prove that applying a training program using a laparoscopic training box during a general surgeon's residency will result in a shortening of time when performing laparoscopic techniques.
Material and methodsAn experimental, longitudinal, comparative, prospective non-blind study was conducted. A 4-week training program was carried out at the Department of General Surgery of a teaching Hospital in northeastern México. The program included an experimental group of first and second-year general surgery residents, as well as interns doing their social service (group A). At the end of the training, a test was conducted where they performed a series of exercises comparing the residents who completed the training program with those in the control group (group B), which included fourth and fifth-year residents who did not complete said training. The program began with the completion of a laparoscopic skills test in a training box, where 7 exercises were performed, bimanual transference using beads toward a post, beads transfer from one container to another, predetermined cut, traction and counter-traction, simulation of intestine inspection using a string, and points of the suture with intracorporeal and extracorporeal knots. This practice was conducted for at least 2h a week for 4 weeks. The exercises consisted of the following:
- I.
Intracorporeal knot: Two suture points will be done with a 4-lacing intracorporeal knot, the total time spent on this knot will be measured. Making an intracorporeal knot on a fixed surface is a common practice in laparoscopic surgery.
- II.
Beads 5/5: 10 beads will be placed (5 yellow and 5 blue) in a container at the center of the image, and there will be two posts, one on the right and another on the left of the container. Using the dominant hand, 5 beads of the same color will be placed on their opposite post, and with the non-dominant hand the rest of the beads which are a different color will be placed on the opposite post. The complete process will be timed from start to finish. This skill is required to perform fine movements and manage depth, necessary skills for staple placement.
- III.
Beads 10/10: Transfer 10 beads from one container to another using the dominant hand and return them to the first container using the non-dominant hand, the amount of time required to finish the exercise will be measured. This skill is necessary to perform fine movement and to moderate pressure strength similar to that required to extract lines from the abdominal cavity.
- IV.
Predetermined cut: A predetermined cut will be made (a circle in a piece of cloth) and the amount of time required to complete the circle will be timed. Skill required in the management of laparoscopic scissors with a single hand and presentation with the other hand is necessary for cuts in laparoscopic surgeries.
- V.
String: Simulation of intestine inspection using a meter-long string with 3 marks, measuring the amount of time it takes to reach the last one. Tests the ability to use both hands, as specified by the simulating intestine inspection.
- VI.
Grape decortication: An exercise in tension and strain relief will be made by decortication of a grape of medium size and the time required to completely peel it will be measured. This ability is required for the use of both hands, well-controlled use of force and pressure of the fine movements required for the detachment of ligaments and loose tissues and dissection and exposure of structures.
- VII.
Extracorporeal knot: A suture will be made with 4 extracorporeal knot loops and the time to finish is measured. Making an extracorporeal knot using the low knots is a common practice in laparoscopic surgery.
Upon completion of the four week training program, participants in the experimental group (group A) must have completed 90% of the previously specified hours (7.2h) and have performed at least 90% of the indicated time periods. A comparative test was performed where residents of Group A and Group B performed the specified exercises, time was taken with a stopwatch, and the two groups’ times were compared at the end of the study.
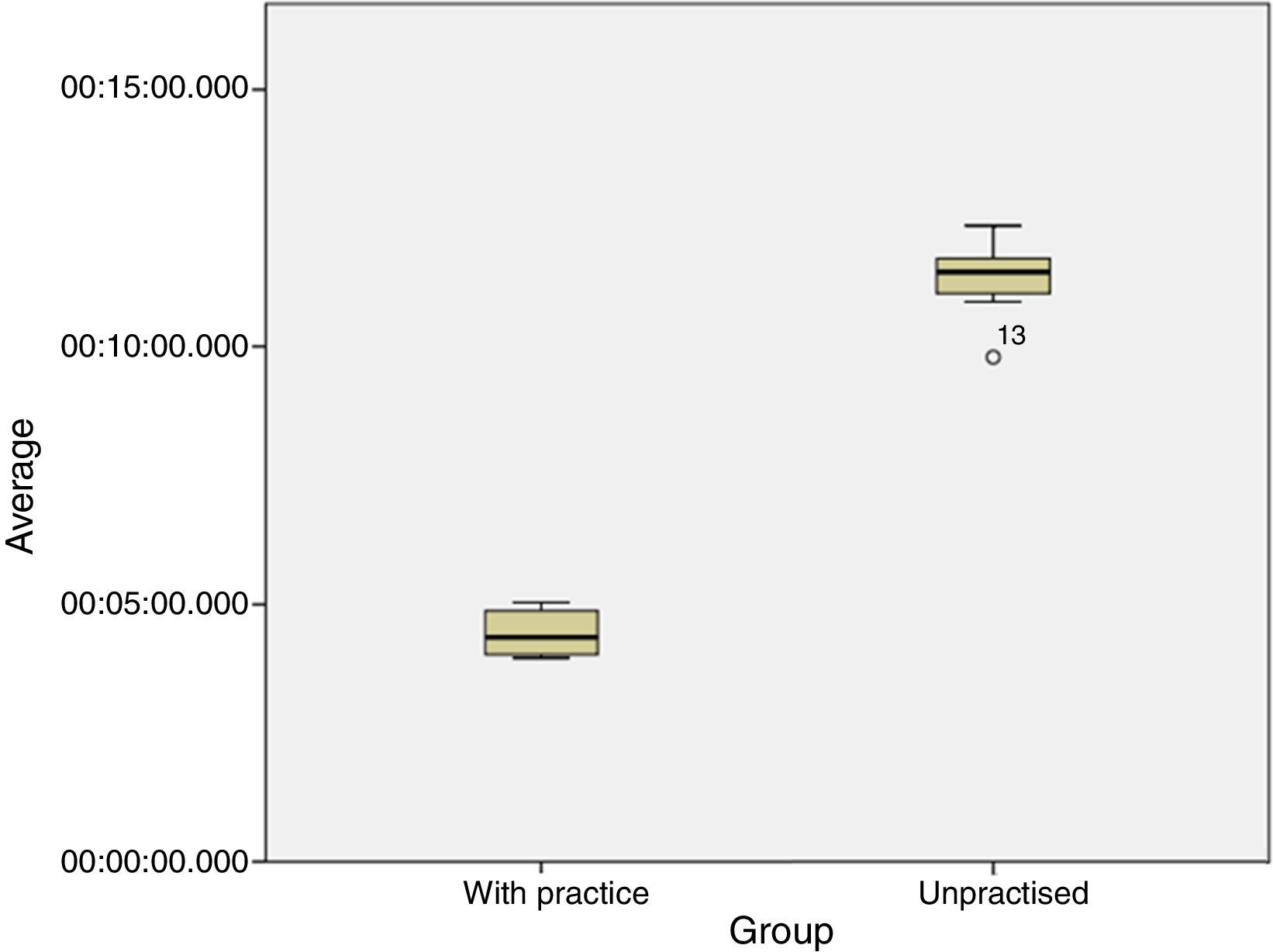
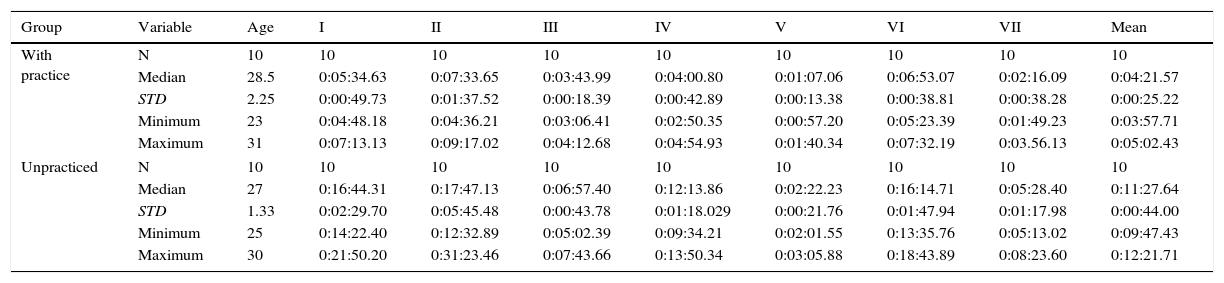
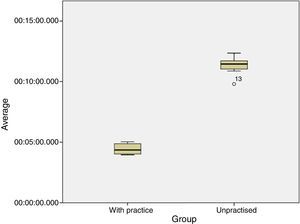
ResultsA total of 20 residents were analyzed, 10 in each group. 15 (75%) were male and 5 (25%) were female. The average age was 28 years. Upon analyzing the two groups, we observed a decrease in group A's average time compared to group B's average times (Table 1).
Descriptive characteristics according to group and exercise of 20 participants with practice and without practice.
| Group | Variable | Age | I | II | III | IV | V | VI | VII | Mean |
|---|---|---|---|---|---|---|---|---|---|---|
| With practice | N | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| Median | 28.5 | 0:05:34.63 | 0:07:33.65 | 0:03:43.99 | 0:04:00.80 | 0:01:07.06 | 0:06:53.07 | 0:02:16.09 | 0:04:21.57 | |
| STD | 2.25 | 0:00:49.73 | 0:01:37.52 | 0:00:18.39 | 0:00:42.89 | 0:00:13.38 | 0:00:38.81 | 0:00:38.28 | 0:00:25.22 | |
| Minimum | 23 | 0:04:48.18 | 0:04:36.21 | 0:03:06.41 | 0:02:50.35 | 0:00:57.20 | 0:05:23.39 | 0:01:49.23 | 0:03:57.71 | |
| Maximum | 31 | 0:07:13.13 | 0:09:17.02 | 0:04:12.68 | 0:04:54.93 | 0:01:40.34 | 0:07:32.19 | 0:03.56.13 | 0:05:02.43 | |
| Unpracticed | N | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | 10 |
| Median | 27 | 0:16:44.31 | 0:17:47.13 | 0:06:57.40 | 0:12:13.86 | 0:02:22.23 | 0:16:14.71 | 0:05:28.40 | 0:11:27.64 | |
| STD | 1.33 | 0:02:29.70 | 0:05:45.48 | 0:00:43.78 | 0:01:18.029 | 0:00:21.76 | 0:01:47.94 | 0:01:17.98 | 0:00:44.00 | |
| Minimum | 25 | 0:14:22.40 | 0:12:32.89 | 0:05:02.39 | 0:09:34.21 | 0:02:01.55 | 0:13:35.76 | 0:05:13.02 | 0:09:47.43 | |
| Maximum | 30 | 0:21:50.20 | 0:31:23.46 | 0:07:43.66 | 0:13:50.34 | 0:03:05.88 | 0:18:43.89 | 0:08:23.60 | 0:12:21.71 | |
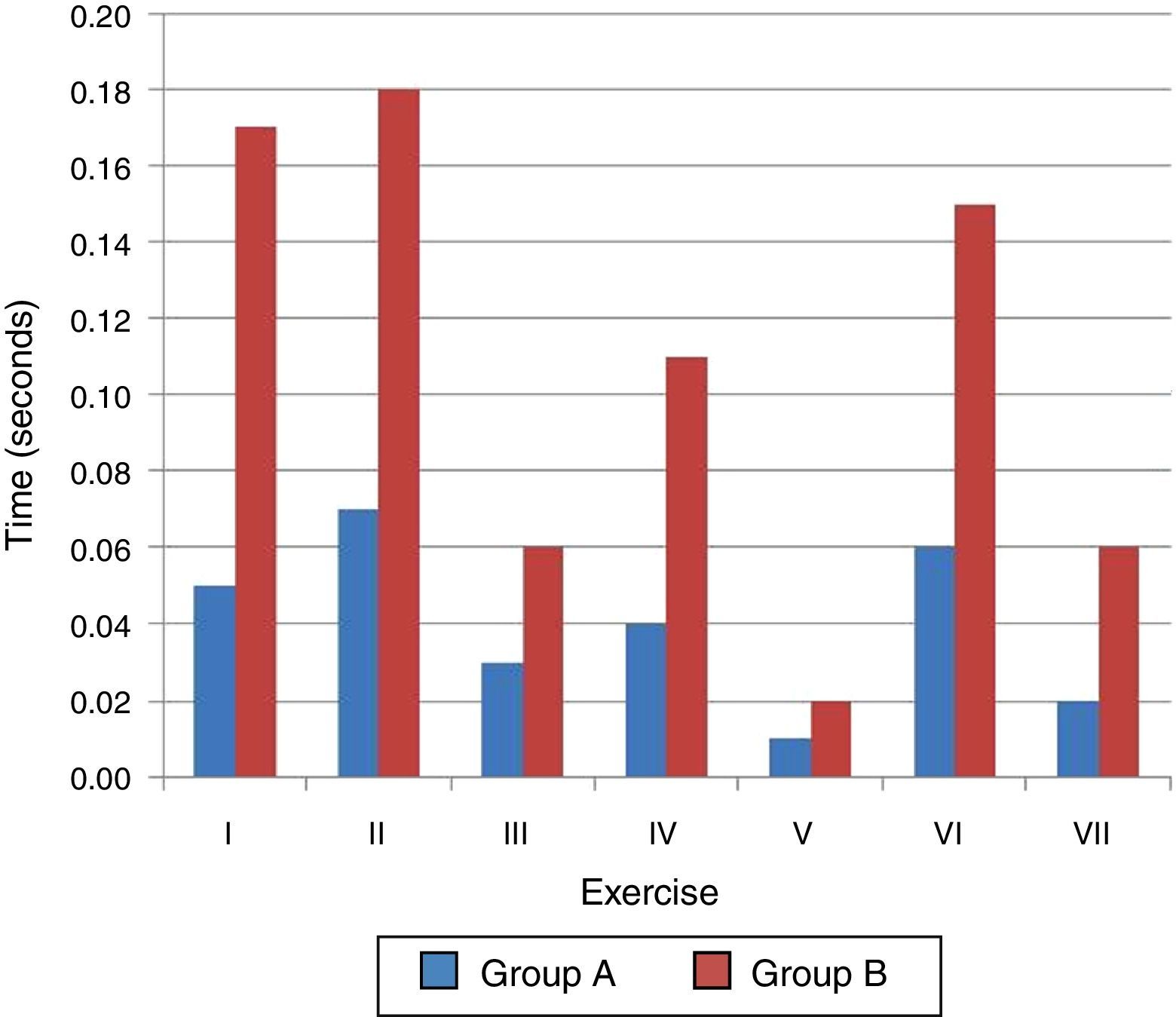
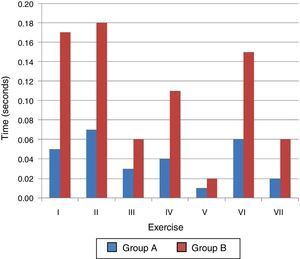
When comparing times, according to the exercise performed, we found the following: in exercise I (intracorporeal knot), there was a greater time difference shown between the two groups, and we found symmetry in subjects in group A and a slight asymmetry in subjects in group B. Exercise II (counts 5/5), was described by subjects as the most difficult. One subject in group B far exceeded the time achieved, on average, for the rest of the subjects in the same group. However, we observed an obvious decrease in group A's average time. In Exercise III (10/10 accounts), a large difference was observed, where group A ended with an average of 4min and group B ended with an average of 7min. Exercise IV (default cut) shows the clear time difference between the two groups, where group A has a shorter time. Exercise V (string), shows that this exercise had the shortest time for the two groups. In group A, there was no decrease in time, with symmetry subjects, contrary to group B, where it took longer and there is asymmetry. Exercise VI (decorticate grape), less time is observed in group A. Exercise VII (low knot knots), shorter time is observed in group A compared to group B, and the latter showed more asymmetry between subjects.
These 7 exercises together show a lower average time difference in group A with 5min, compared to group B with 12min, p<0.05 (Figs. 1 and 2).
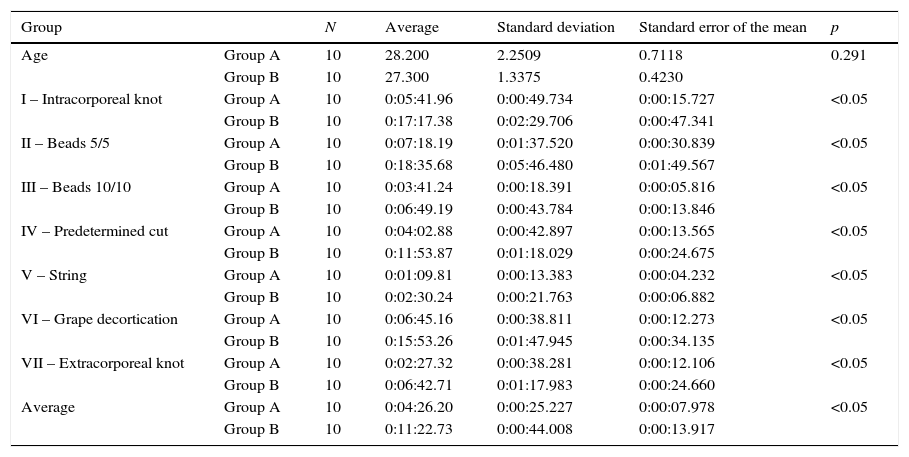
Therefore, we stress that exercise II presented greater difficulty, showing increased consumption of time, and exercise number V shows the least difficulty. Of the 7 exercises, we can observe a difference in the performance time in both groups, with significant differences (Table 2).
Descriptive analysis between the two groups according to performance times.
| Group | N | Average | Standard deviation | Standard error of the mean | p | |
|---|---|---|---|---|---|---|
| Age | Group A | 10 | 28.200 | 2.2509 | 0.7118 | 0.291 |
| Group B | 10 | 27.300 | 1.3375 | 0.4230 | ||
| I – Intracorporeal knot | Group A | 10 | 0:05:41.96 | 0:00:49.734 | 0:00:15.727 | <0.05 |
| Group B | 10 | 0:17:17.38 | 0:02:29.706 | 0:00:47.341 | ||
| II – Beads 5/5 | Group A | 10 | 0:07:18.19 | 0:01:37.520 | 0:00:30.839 | <0.05 |
| Group B | 10 | 0:18:35.68 | 0:05:46.480 | 0:01:49.567 | ||
| III – Beads 10/10 | Group A | 10 | 0:03:41.24 | 0:00:18.391 | 0:00:05.816 | <0.05 |
| Group B | 10 | 0:06:49.19 | 0:00:43.784 | 0:00:13.846 | ||
| IV – Predetermined cut | Group A | 10 | 0:04:02.88 | 0:00:42.897 | 0:00:13.565 | <0.05 |
| Group B | 10 | 0:11:53.87 | 0:01:18.029 | 0:00:24.675 | ||
| V – String | Group A | 10 | 0:01:09.81 | 0:00:13.383 | 0:00:04.232 | <0.05 |
| Group B | 10 | 0:02:30.24 | 0:00:21.763 | 0:00:06.882 | ||
| VI – Grape decortication | Group A | 10 | 0:06:45.16 | 0:00:38.811 | 0:00:12.273 | <0.05 |
| Group B | 10 | 0:15:53.26 | 0:01:47.945 | 0:00:34.135 | ||
| VII – Extracorporeal knot | Group A | 10 | 0:02:27.32 | 0:00:38.281 | 0:00:12.106 | <0.05 |
| Group B | 10 | 0:06:42.71 | 0:01:17.983 | 0:00:24.660 | ||
| Average | Group A | 10 | 0:04:26.20 | 0:00:25.227 | 0:00:07.978 | <0.05 |
| Group B | 10 | 0:11:22.73 | 0:00:44.008 | 0:00:13.917 |
There is a homogeneity between the two groups with regard to distribution by age and gender. The study involved a total of 20 subjects, 10 were subjected to training two hours a week for four weeks, and finally, were subjected to the application of the 7 exercises mentioned in Table 1, while the other 10 only underwent the implementation of the 7 exercises already mentioned. A considerable time difference was demonstrated in the performance of laparoscopic tasks between the two groups. We found that, of the seven tasks applied and measured, exercise II, where the subjects must place 5 beads of the same color on their opposite post and vice versa, as presenting the greatest difficulty to implement, and exercise V, mobilization of the string, as the simplest, as can be seen in Table 1. At the end, we obtained significant statistical p values in the 7 exercises between the two groups.
In a German study, which involved eight expert surgeons and 24 rookies (inexperienced medical students), in which they performed exercises on two physical laparoscopic training simulators, a virtual endoscopic surgery trainer, and a conventional video training device, both groups showed improvement in their times upon completion of their training, as opposed to at the beginning. However, the skilled surgeons had the best times in all exercises, unlike our study, where those who underwent the laparoscopic training without previous experience had better times.1
In another study in Australia with 26 participants involving the use of a conventional laparoscopic simulator compared to a virtual simulator, greater consistency in learning was observed with the conventional laparoscopic simulator, which was also used in our study so that we could provide a good training tool.10
In a study conducted in Spain with a laparoscopic simulator, it was observed that the residents’ level of confidence in the practice of laparoscopic procedures after completion of training increased by 70%, thus, just as in our study results in better surgical times.11
Conducting training in laparoscopic surgery skills with a physical simulator significantly reduces turnaround times in the tasks involved in such procedures. It showed that training in a physical laparoscopic surgery simulator, for at least two hours a week for a month, is sufficient to improve laparoscopic surgical skills and reduce turnaround times by more than half compared to the times of those that do not undergo the training. This lead us to believe that, as the surgeon undergoes more training from the early stages of his residency in general surgery, he will be able to show a better perform with safer skills when met with the situation of performing a laparoscopic procedure on a living person, thus achieving a reduction in the risk of complications arising from a lack of technique or skills in this type of procedure. Yet we must always keep in mind that physical simulators for laparoscopic training are just a tool to enhance one's ability, and must never replace training and experience in actual surgery assisted by teachers and expert surgeons.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo financial support was provided.
Conflict of interestThe authors have no conflicts of interest to declare.