The incidence of infectious spondylodiscitis has been shown to rise with age; however, they had not been extensively investigated in the very elderly.
Material and methodsThis retrospective, monocentric study included patients hospitalized in our department of rheumatology for primary infectious spondylodiscitis between 2000 and 2015, and compared over 75-year-olds with younger patients.
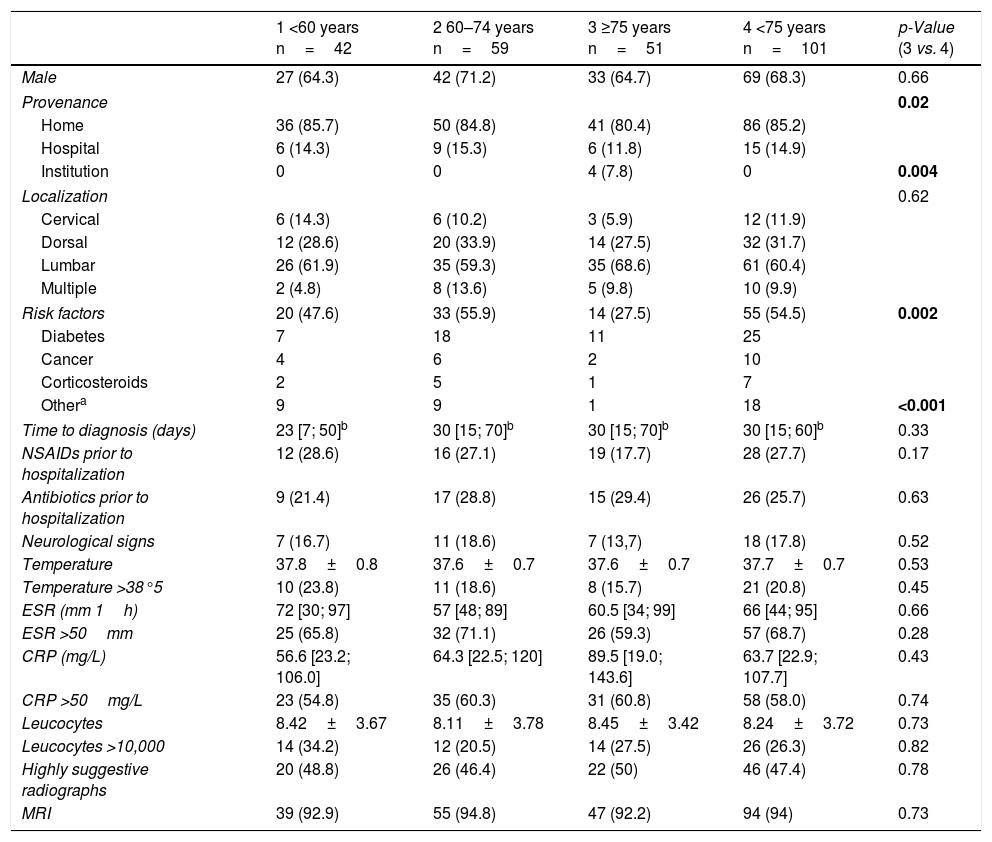
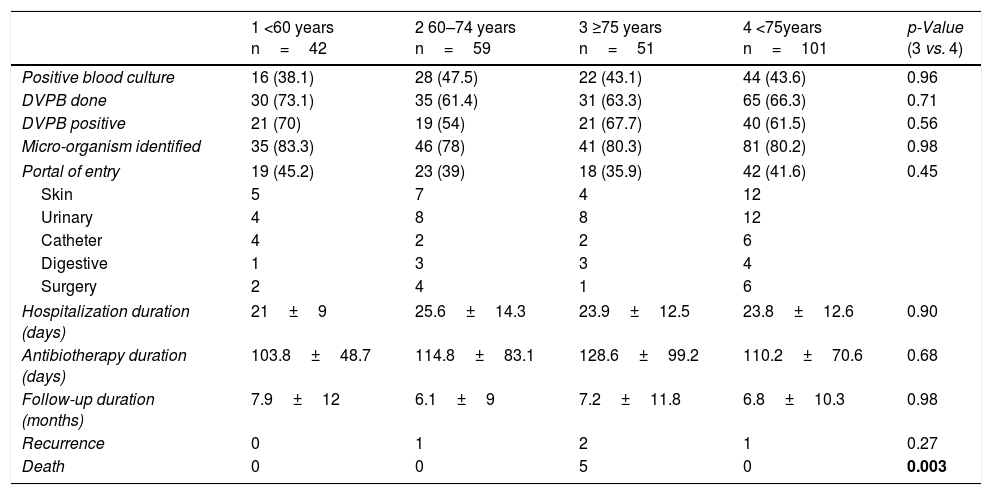
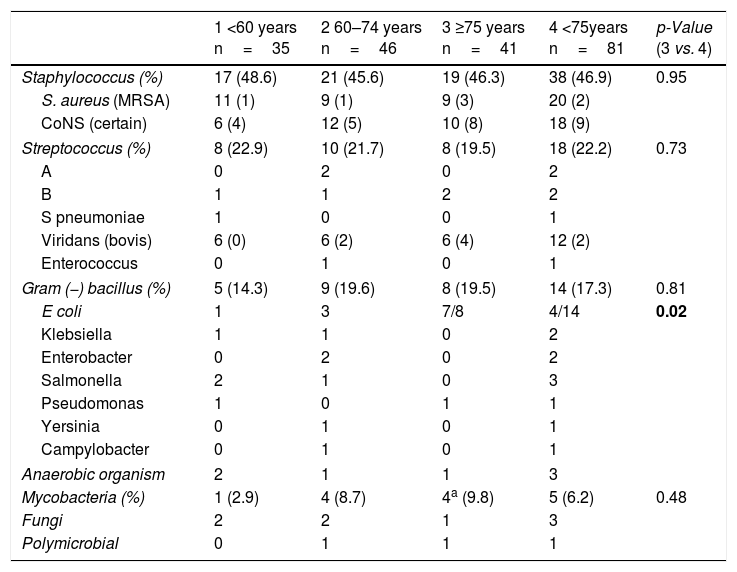
ResultsOf the 152 patients, 51 (33.6%) were≥75 years old, 59 were 61–74, and 42 were≤60. Patients≥75 years old were more often institutionalized (7.8 vs. 0; p=0.02), were less often subject to infection risk factors (27.5 vs. 54.5%; p=0.02), but did not differ from the others as regards the frequency of diabetes and cancer. Time to diagnosis was shorter for the under 60-year-olds (23 vs. 30 vs. 30 day for each age group, respectively; p<0.05). There were no differences among the age groups in terms of spondylodiscitis localization, frequency of neurological symptoms and fever, frequency or intensity of inflammatory syndrome, imaging use, frequency of microorganism identification, blood culture positivity, or use and efficacy of disco-vertebral biopsy. Microorganism distribution was comparable among the groups, except for Gram-negative bacilli, with Escherichia coli more common in over 75-year-olds (7/8 vs. 4/14; p=0.02). Duration of antibiotherapy and hospitalization was comparable across the age groups. Five patients died, all over 75 years old (5/51 vs. 0/101; p=0.001).
ConclusionAge is a risk factor for primary spondylodiscitis, associated with significant mortality in over 75-year-olds (10%). For these elderly patients, spondylodiscitis does not bear any other distinguishing features.
Se ha demostrado que la incidencia de la espondilodiscitis infecciosa se incrementa con la edad; sin embargo, esto no ha sido investigado ampliamente en los mayores.
Material y métodosEstudio retrospectivo, en un único centro, que incluyó a los pacientes hospitalizados en nuestro Departamento de Reumatología debido a espondilodiscitis infecciosa entre 2000 y 2015, y comparación de los pacientes mayores de 75 con los pacientes más jóvenes.
ResultadosDe los 152 pacientes, 51 (33,6%) eran≥75 años, 59 de entre 61 y 74, y 42≤60. Los pacientes≥75 estaban frecuentemente institucionalizados (7,8 frente a 0; p=0,02), estuvieron menos sujetos a los factores de riesgo de infección (27,5 frente a 54,5%; p=0,02), pero no difirieron del resto en cuanto a la frecuencia de diabetes y cáncer. El tiempo de diagnóstico fue menor para los pacientes menores de 60 años (23 frente a 30 frente a 30 días para cada grupo de edad, respectivamente; p<0,05). No se produjeron diferencias entre los grupos de edad en términos de localización de la espondilodiscitis, frecuencia de síntomas neurológicos y fiebre, frecuencia o intensidad del síndrome inflamatorio, toma de imágenes, frecuencia de identificación de microorganismos, positividad del hemocultivo, o uso o eficacia de la biopsia discovertebral. La distribución de los microorganismos fue comparable entre los grupos, exceptuando los bacilos gramnegativos, siendo Escherichia coli el más común en los pacientes mayores de 75 años (7/8 frente a 414; p=0,02). La duración del tratamiento antibiótico y la hospitalización fueron comparables entre los grupos de edad. Cinco pacientes fallecieron, todos ellos mayores de 75 años (5/51 frente a 0/101; p=0,001).
ConclusiónLa edad es un factor de riesgo para la espondilodiscitis primaria, que se asocia a una mortalidad significativa en los pacientes mayores de 75 años (10%). Para estos pacientes mayores, la espondilodiscitis no comporta otras características distintivas.