The anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis with renal involvement are associated with high morbi-mortality. In this study we analyse if the prognosis of these diseases have improved in recent years, and which factors influence the outcomes.
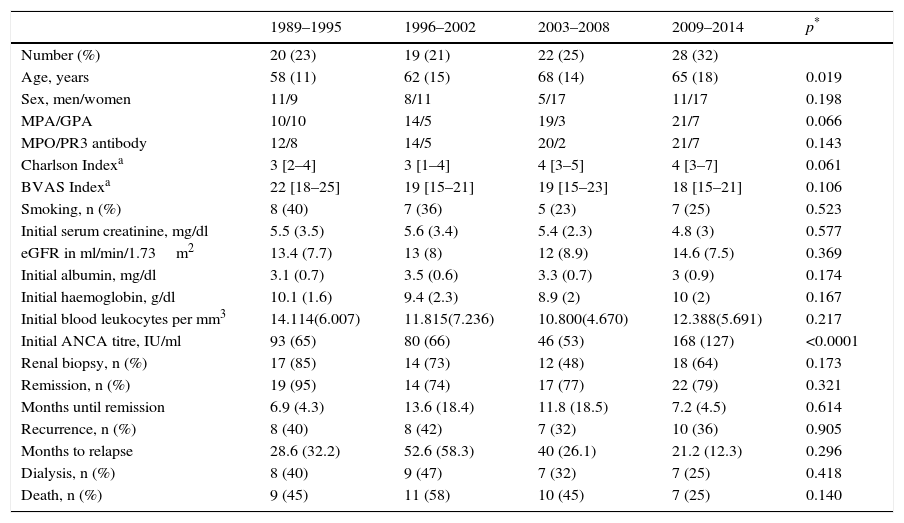
Material and methodsRetrospective single-centre observational study, which included all patients diagnosed with microscopic polyangiitis and granulomatosis with polyangiitis with renal involvement in the last 25 years. Demographic, clinical and biochemical parameters of prognostic interest were recorded. The differences between four chronological periods were analysed, along with the determinants of a poor outcome (death or end-stage renal disease).
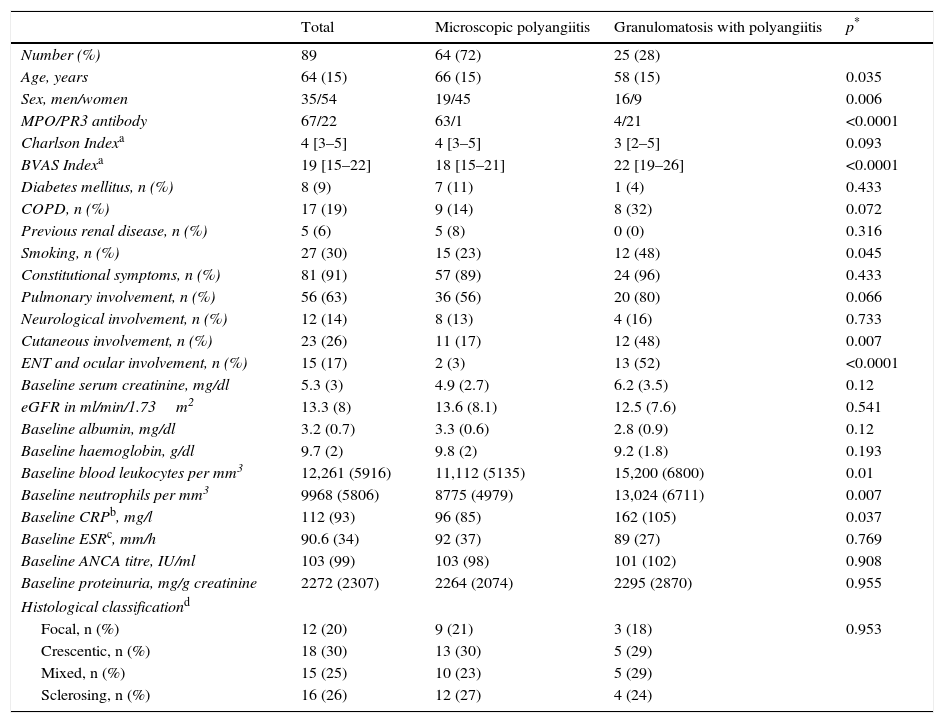
ResultsEighty-nine patients were included (mean age 64±15 years). Sixty-four patients (72%) had microscopic polyangiitis and 25 (28%) granulomatosis with polyangiitis.
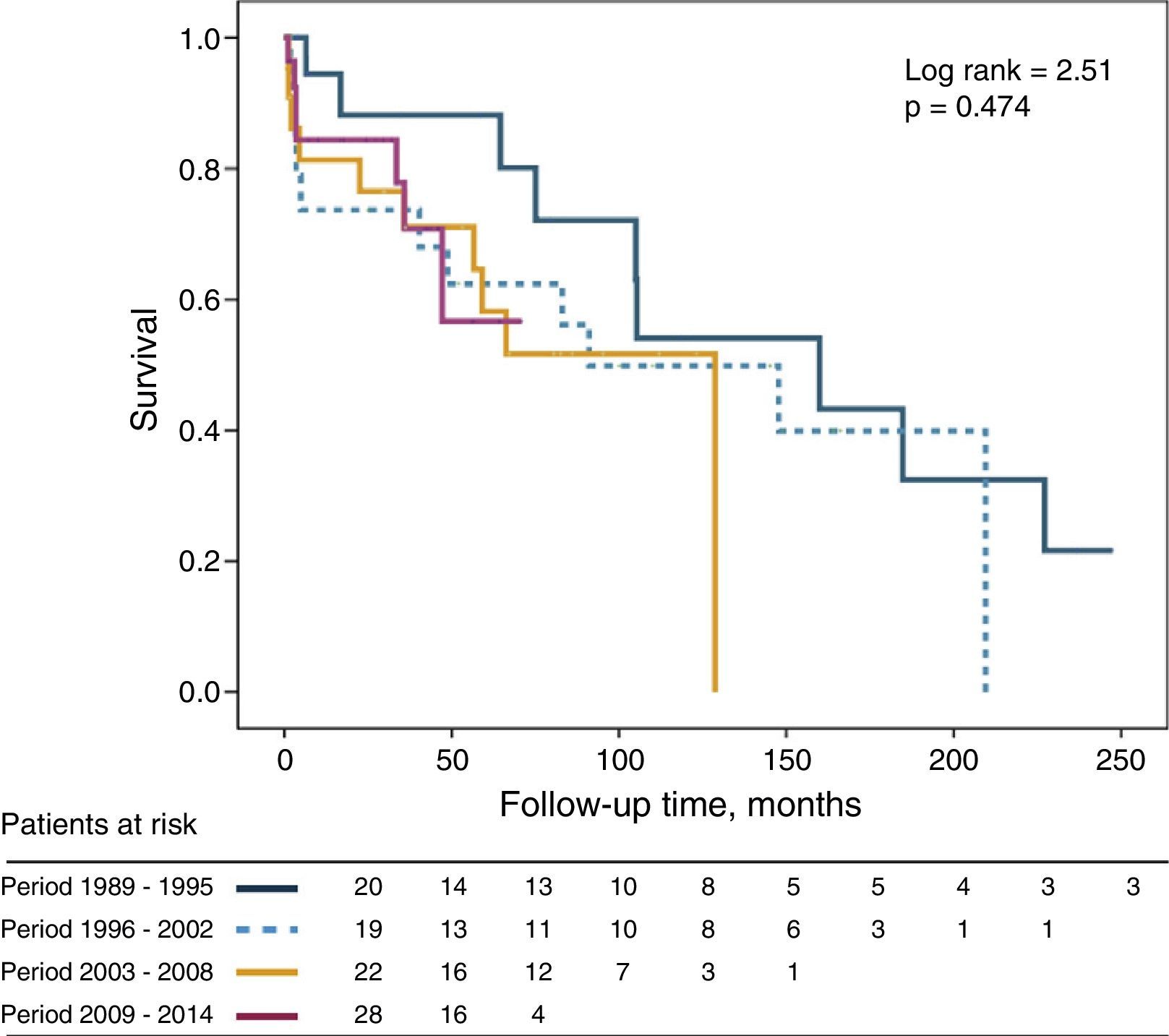
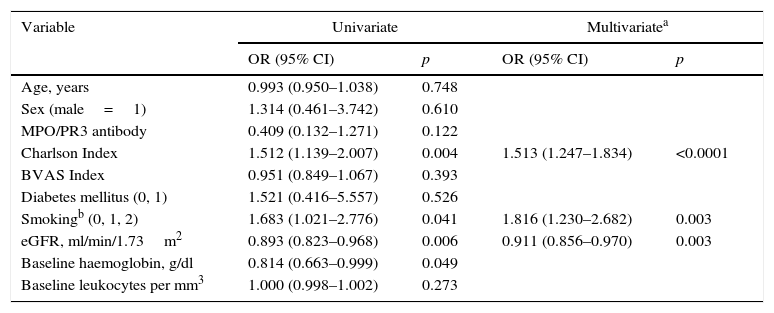
During the study period, 37 (42%) patients died. Through Cox regression analysis, the best determinants of mortality were the initial glomerular filtration rate (HR 0.911; p=0.003), Charlson comorbidity index (HR 1.513; p<0.0001) and tobacco smoking (HR 1.816; p=0.003).
35% developed end-stage renal disease, and the best determinants (by competing-risk regression) were: initial glomerular filtration rate (sub-hazard ratio [SHR]: 0.791; p<0.0001), proteinuria (SHR: 1.313; p<0.0001), and smoking status (SHR: 1.848; p=0.023).
No differences were found in patients’ mortality or renal survival between the different study periods.
ConclusionsPrognosis of anti-neutrophil cytoplasm antibodies vasculitis with renal involvement treated with conventional immunosuppressive therapy remains unsatisfactory, and continues to have increased long-term complications and mortality.
Las vasculitis con anticuerpos contra el citoplasma de neutrófilo con afectación renal se asocian con una elevada morbimortalidad. En este estudio se analiza si el pronóstico de estas vasculitis ha mejorado en los últimos años, y cuáles son los factores que condicionan su evolución.
Material y métodosEstudio retrospectivo de observación que incluyó a pacientes con poliangitis microscópica y granulomatosis con poliangitis con afectación renal diagnosticados en nuestro hospital durante los últimos 25 años. Se recogieron los parámetros demográficos, clínicos y bioquímicos de interés pronóstico, y se analizaron las diferencias según 4 períodos cronológicos, así como los determinantes de una peor evolución (muerte o insuficiencia renal terminal).
ResultadosSe incluyeron 89 pacientes (edad media 64±15 años). Sesenta y cuatro pacientes (72%) presentaban poliangitis microscópica y 25 (28%) granulomatosis con poliangitis.
Durante el período de estudio, 37 (42%) pacientes fallecieron. Mediante análisis de regresión de Cox, los determinantes de mortalidad fueron el filtrado glomerular basal (HR 0,911; p=0,003), índice de Charlson (HR 1,513; p<0,0001) y exposición al tabaco (HR 1,816; p=0,003).
El 35% desarrolló insuficiencia renal terminal. Los mejores determinantes de este acontecimiento (en competencia de riesgo por muerte) fueron: filtrado glomerular basal (sub-hazard ratio [SHR]: 0,791; p<0,0001), proteinuria (SHR: 1,313; p<0,0001), y hábito tabaco (SHR: 1,848; p=0,023).
No se observaron diferencias en la supervivencia total o renal en los diferentes períodos estudiados.
ConclusionesEl pronóstico de las vasculitis con anticuerpos contra el citoplasma de neutrófilo con afectación renal y tratamiento inmunosupresor convencional sigue siendo desfavorable, asociándose con numerosas complicaciones y elevada mortalidad.