Meibomian gland dysfunction (MGD) is the most common cause of dry eye and is recommended to be treated by warm and moist compresses followed by lid massage and lid scrub. This case report describes changes of ocular sign, tear film and meibomian gland morphology of a non‐obvious MGD patient (lid margin, meibomian gland orifices and ocular signs appeared to be normal) undergoing MGD treatment. Without gland expression and/or meibography this form of MGD would have been overseen. Tear film, ocular signs and symptoms improved significantly after treatment. Expressibility of glands was improved with treatment although the MGD accompanying loss of meibomian glands —evaluated by non‐contact meibography— was unchanged. Loss of meibomian glands might either be irreversible or would need more extended treatment.
La disfunción de las glándulas de Meibomio (DGM) es la causa más frecuente de ojo seco y se recomienda tratarla con compresas tibias y húmedas y a continuación un masaje y fregado de párpados. En este caso clínico se describen los cambios de signos oculares, de la película lagrimal y la morfología de las glándulas de Meibomio de un paciente con DGM no obvia (el margen del párpado, los orificios de las glándulas de Meibomio y los signos oculares parecían normales) sometido a tratamiento para la DGM. Sin la expresión de las glándulas y/o la meibografía, esta forma de DGM se habría examinado. La película lagrimal y los signos y síntomas oculares mejoraron de manera significativa tras el tratamiento. La expresividad de las glándulas mejoró con el tratamiento, aunque la DGM que iba unida a la pérdida de glándulas de Meibomio ¿evaluadas mediante meibografía sin contacto¿ permaneció sin cambios. La pérdida de glándulas de Meibomio puede ser irreversible o requerir un tratamiento más extenso.
Meibomian gland dysfunction (MGD) is one of the most common abnormalities in ophthalmic practice1 causing an abnormality of the tear film lipid layer2 resulting in the evaporative dry eye.3 MGD can be diagnosed by lid morphology, MG mass, gland expressibility, lipid layer thickness and loss of MG by meibography.3 Meibography is a technique to visualize the morphology of the meibomian glands. One principal is the transillumination of the everted lid4–6 the other one the direct illumination, named the non‐contact meibography.7–10 In transillumination the lid is everted over a light source5,11 while non‐contact meibography10 consist of a slit lamp equipped with an infrared charge‐coupled device video camera and an infrared transmitting filter10 to allow the observation of the everted lid without contact to the instrument. Recently our group described using a normal IR CCD camera in meibography instead12,13 or the built‐in IR cameras of common ophthalmic instruments to be designed for pupillometry (Figure 1).12,14,15 Later on this idea was used by Srinivasan et al.14,16
An example of normal meibomian glands morphology. Photograph was taken by a modified Sirius® Scheimpflug Camera using the pupillometry option (C.S.O, Construzionne Strumenti Oftalmici, Florence, Italy; bon Optic VertriebsgmbH, Lübeck, Germany).12,15.
Blackie et al17 were first describing the “non‐obvious MGD”. A form of MGD where inflammation and ocular signs of pathology may be minimal and thus non‐obvious or absent altogether.17 This form of MGD would only be detectable by evaluating the expressibility of glands and extend of gland drop‐out.17 Additionally to gland expression meibography give the practitioner further information of the subjects meibomian gland morphology and long‐term effect of MGD.10,11
Loss of meibomian glands analyzed by meibograpy is significantly correlated to dry eye symptoms and tear film.13 Daily application of warm and moist compresses, followed by appropriate lid hygiene improves MGD.18,19 While tear film, ocular signs, symptoms and expressibility of glands can improve applying this treatement19,20 its unknown the effect on in the meibomian glands loss criteria.
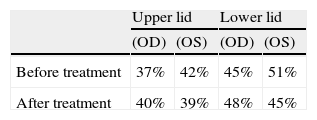
Case reportA 42 year old white female claimed dry eye. Symptoms were assessed by the Ocular Surface Disease Index (OSDI). OSDI score was 37.5. Lid margin and meibomian gland orifices appeared to be normal (Figure 2), no meibomian gland plugging, no conjunctival or corneal staining or redness (Efron Grading Scale21: Grade <1), however meibomian glands were poorly expressible and expressed fluid was turbid. Loss of meibomian glands was evaluated by the portable non‐contact infra‐red (IR) meibograph (PNCM)13 and computerized grading (ImageJ 1.42q, Wayne Rasband, National Institute of Health, USA)13 and resulted in 37% (OD) loss of glands of the upper lid (Table 1). Non‐invasive break‐up time (NIBUT) was measured with the Tearscope® (Keeler, UK Ltd.) with a fine grid insert. The median of three consecutive measurements was 7.1 seconds (OD).22 Lipid layer thickness was less than 30 nm23 evaluated using the Tearcsope (without grid). Schirmer test I was 16 mm (OD).
Hyper‐evaporative dry eye caused by MGD was diagnosed because of OSDI scores,24,25 the poor expressibility of the glands,17,25 the reduced tear film stability25 and lipid layer thickness25 and meibomian gland loss of more than 30%7,8,13,25 but normal Schirmer test. Since lids appeared to be normal (no obvious inflammation and other signs of pathology17) MGD was classified as “non‐obvious MGD”.17
The response to treatment was evaluated by expressibility, character of secretion and loss of glands determined by meibography.17,20 Daily use of Blephasteam® eye lid warming device (Thea Laboratoires, Clermont‐Ferrand, France) followed by lid massage and lid scrub using Blepha Cura® (Optima Pharmazeutische GmbH, Moosburg/Wang, Germany) was recommended.
At the follow‐up after 3 weeks, expressibility of the meibomian glands was normal and the expressed meibom oil was clear and fluid. NIBUT improved to 11.2 seconds (OD), OSDI scores decreased significantly to 2.8. Lipid layer thickness was 75 nm. Schirmer test (17 mm) and loss of meibomian glands (OD, 40%) (Figure 3, Table 1) was unchanged.
Loss of meibomian glands before (right) and after 3 weeks treatment (left). Meibographs were taken by the portable non‐contact IR meibograph (PNCM).13.
The daily use of the eyelid warming device —followed by lid massage and lid scrub— over a 3 week period significantly improved the patient‘s dry eye symptoms, as well as tear film stability and meibomian gland dysfunction (MGD) scores. The lipid layer thickness increased significantly even though 75 nm thickness is still borderline.23 The tear film stability measured by the tearscope approached normal values.26 However loss of meibomian glands was unchanged (Figure 3).
These findings are of interests, since MGD might have been overseen without expression of the glands and/or meibography. Expression and the evaluation of gland loss is essential in evaluating MGD, especially in the non‐obvious form.17 Meibography images let us assume a long history of MGD10 of this 42 year old patient. Lid hygiene as described is able to improve function of the remaining meibomian glands to improve tear film stability and function in relief of symptoms of dry eye. Furthermore these findings let us assume that loss of meibombian glands might be irreversible or would need longer and advanced treatment. However, MGD treatment by lid warming, lid massage and lid scrub was effective and might reduce or stop progression of the meibomian glands degeneration even in early MGD status.
Longitudinal investigation is ongoing to confirm this hypothesis in an appropriate sample size.