Corneal refractive therapy is a non-surgical procedure whose main purpose is to improve uncorrected visual acuity during the day, without spectacles or contact lenses. We report an adult woman who shows contact lens intolerance and does not want to wear eyeglasses. We used dual axis contact lens to improve lens centration. We demonstrate a maintained unaided visual acuity during one year of treatment. In conclusion, we can consider refitting with dual axis lens for corneal refractive therapy as a non-surgical option for patients who show contact lens intolerance.
La terapia refractiva corneal es un procedimiento no quirúrgico cuyo objetivo principal es mejorar la agudeza visual no corregida durante el día sin necesidad de gafas ni lentes de contacto. Presentamos el caso de una mujer adulta con intolerancia a las lentes de contacto que no quiere llevar gafas. Utilizamos una lente de contacto de doble eje para mejorar el centrado de la lente. Demostramos una agudeza visual espontánea mantenida durante un año de tratamiento. En conclusión, podemos considerar la readaptación con lente de doble eje para terapia refractiva corneal como una opción no quirúrgica para pacientes que presentan intolerancia a las lentes de contacto.
Corneal refractive therapy (CRT) is a non-surgical procedure that consists on corneal reshape while the patient is sleeping. The practitioner can achieve a temporarily reduction of the refractive error by the overnight wear modality of a special therapeutic contact lens (CL).
The main CRT purpose is to improve uncorrected visual acuity (VA) during the day, without spectacles or CL. So it could be considered as a reliable non-surgical option to refractive surgery.1
Nowadays, there are more than 20 different kinds of inverse geometry CL, with different fitting protocols. However, Paragon CRT® was the first overnight wear CL approved by the Food and Drug Administration (FDA) for CRT on June 2002,2,3 to correct myopia up to about 6.00 D even with a myopic astigmatism of 1.75 D regardless of the orientation.
This paper describes a case of CRT fitting with Paragon CRT® Dual Axis™ CL for overnight orthokeratology (OK).
Case reportA 37-year-old daytime CL wearer woman came to be informed of overnight OK. She was contact lens intolerant and wanted to be relieved from complete dependence on eyeglasses. The patient wore CL for 22 years. First, she wore rigid gas-permeable lenses (RGP), being the normal average wearing time more than 14 hours on 7 days per week. Sometimes she slept with the CL. After that, the patient started to wear soft CL (vifilcon A), and the normal average wearing time was 4–5 hours, because she experienced dryness symptoms and she preferred wearing spectacles rather than CL, probably due to her previous experience of RGP lens wearing. We tried to refit with other materials such as silicone hydrogel but her symptoms did not improve. She complained of discomfort and blurred vision after a few hours of CL wearing. She was informed about CRT and as she was an appropriate candidate, an appointment was arranged to determine her best fit lens option.
The patient had an unremarkable ocular and general health history. Results of pre-CRT examination were:
- 1.
Ocular examination:
- –
Slit-lamp examination did not evidence any problem that adviced against CRT CL wear.
- –
Tear meniscus deficit (0.1mm).
- –
Tear film break-up time (TFBUT):<8 sec.
- –
Corneal eccentricity was: OD: 0.41 OS: 0.35.
- –
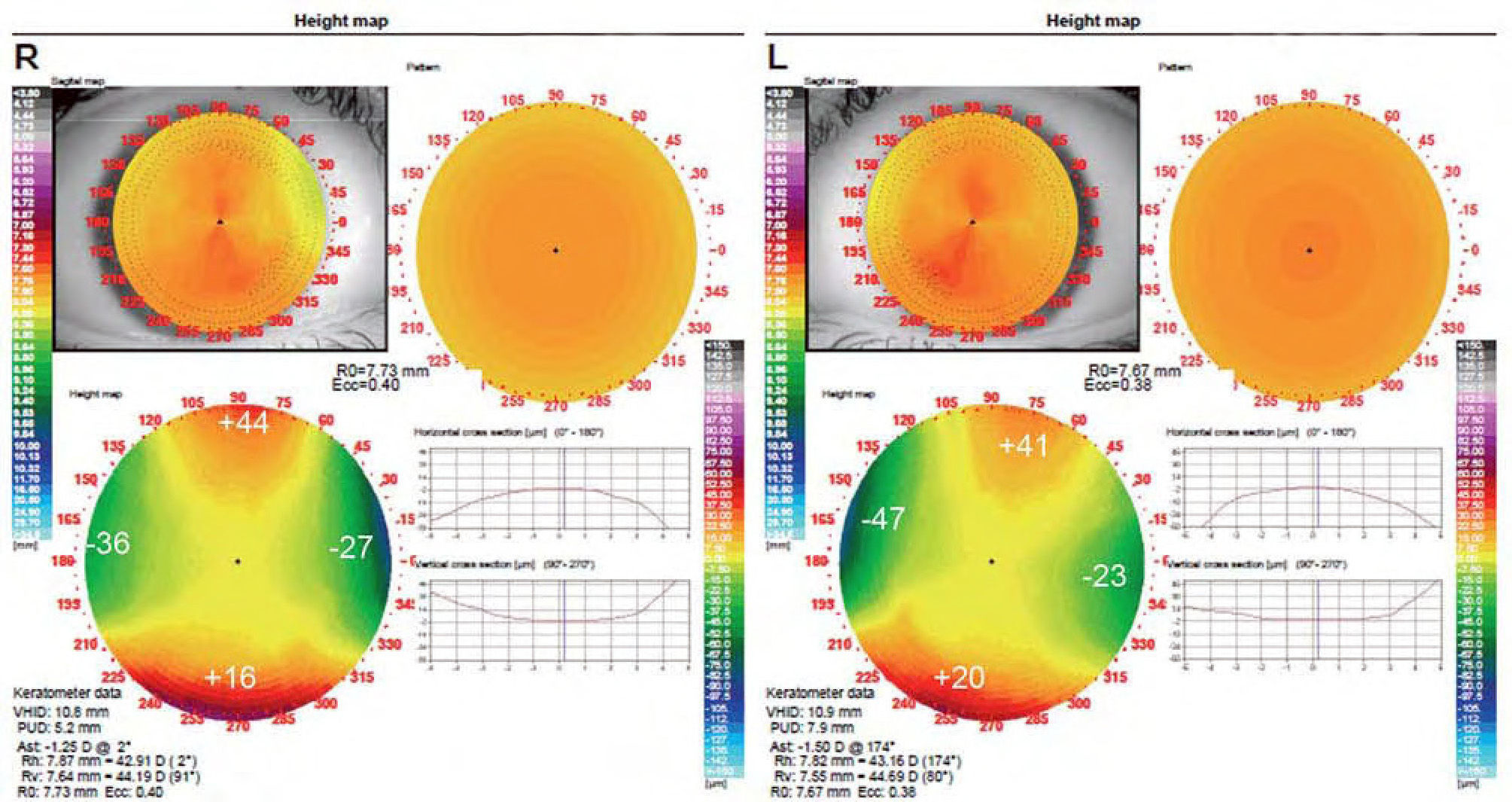
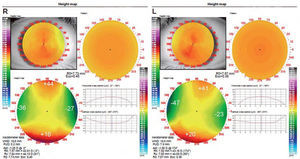
Corneal topography was measured using a topographer (Optopol CT110, Optopol, Poland). In her pre-CRT topography a 1.25 D and a 1.50 D with the rule (WTR) corneal astigmatism was found in OD and OS, respectively (Figure 1).
Figure 1.Pre-treatment topographical elevation maps of the right (R) and left (L) eyes. Those elevation maps reveals: OD: a difference of 61.5μm between meridians, OS: a difference of 65.5μm between meridians. According to general guidelines these differences justify the use of Dual Axis lens.
(0.38MB). - –
Pupil size was measured with a ruler under mesopic conditions: 4.25mm in both eyes.
- –
Horizontal visible iris diameter was measured with a ruler and with the topographer: OD: 10.8mm, OS: 10.9mm.
- –
- 2.
Visual examination. Subjective refraction:
- –
Refraction was first measured using an autorefractometer (Topcon RMA7000B, Topcon, Japan), and subjective was done by a foropter (Reichert, 11625, Leica Inc, USA).
- –
OD: −3.00-0.75×10 visual acuity (VA) 20/20; OS: –4.00-1.00×165 VA 20/20.
- –
According to this preliminary examination the patient exhibited a moderate myopia with low amount of astigmatism in both eyes. Because WTR astigmatism up to −1.75 D can be treated by CRT, we proposed to fit a Paragon CRT® CL, manufactured in Paragon HDS 100 material.
To fit the lens, the diagnostic device system provided by the manufacturer was used. This device gave the first diagnostic lens: Base curve radius (BCR), return zone depth (RZD) and landing zone angle (LZA), standard CRT lens diameter (10.5mm) was used. The patient exhibited a fluctuating VA with poor lens centration with spherical lenses (Table 1), we ruled out the possibility that poor lens centration was due to the lens diameter, as the lens covered 85–90% of corneal diameter, in agreement with general guidelines. So, it was decided to try the Paragon CRT® Dual Axis™ which provides an improved lens alignment and centration (see discussion for details). When we examined pre-treatment topographical elevation maps, in which the difference between the sagital height of the horizontal and vertical meridians is calculated (Figure 1), data obtained were: OD: a difference of 61.5 μm between meridians, OS: a difference of 65.5 μm between meridians. These differences in elevation were obtained from the average of elevation at 4mm chord diameter along the steepest and flattest keratometric meridians, and were used to determine the first Dual Axis trial lens. According to general guidelines these differences justify the use of Dual Axis lens.
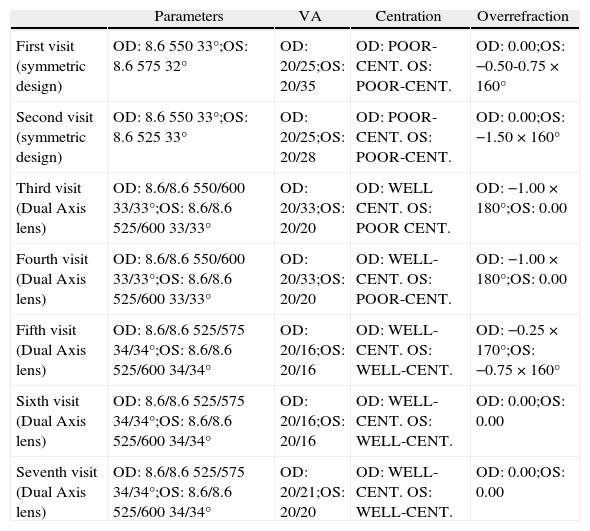
Number of visits performed and explained in the text. Some other visits took place between them, it is clarified in the text, but those visits were not included due to lack of interest they had for final contact lens prescription
| Parameters | VA | Centration | Overrefraction | |
| First visit (symmetric design) | OD: 8.6 550 33°;OS: 8.6 575 32° | OD: 20/25;OS: 20/35 | OD: POOR-CENT. OS: POOR-CENT. | OD: 0.00;OS: −0.50-0.75 × 160° |
| Second visit (symmetric design) | OD: 8.6 550 33°;OS: 8.6 525 33° | OD: 20/25;OS: 20/28 | OD: POOR-CENT. OS: POOR-CENT. | OD: 0.00;OS: −1.50 × 160° |
| Third visit (Dual Axis lens) | OD: 8.6/8.6 550/600 33/33°;OS: 8.6/8.6 525/600 33/33° | OD: 20/33;OS: 20/20 | OD: WELL CENT. OS: POOR CENT. | OD: −1.00 × 180°;OS: 0.00 |
| Fourth visit (Dual Axis lens) | OD: 8.6/8.6 550/600 33/33°;OS: 8.6/8.6 525/600 33/33° | OD: 20/33;OS: 20/20 | OD: WELL-CENT. OS: POOR-CENT. | OD: −1.00 × 180°;OS: 0.00 |
| Fifth visit (Dual Axis lens) | OD: 8.6/8.6 525/575 34/34°;OS: 8.6/8.6 525/600 34/34° | OD: 20/16;OS: 20/16 | OD: WELL-CENT. OS: WELL-CENT. | OD: −0.25 × 170°;OS: −0.75 × 160° |
| Sixth visit (Dual Axis lens) | OD: 8.6/8.6 525/575 34/34°;OS: 8.6/8.6 525/600 34/34° | OD: 20/16;OS: 20/16 | OD: WELL-CENT. OS: WELL-CENT. | OD: 0.00;OS: 0.00 |
| Seventh visit (Dual Axis lens) | OD: 8.6/8.6 525/575 34/34°;OS: 8.6/8.6 525/600 34/34° | OD: 20/21;OS: 20/20 | OD: WELL-CENT. OS: WELL-CENT. | OD: 0.00;OS: 0.00 |
By fitting spherical Paragon CRT® CL it was possible to obtain the dual axis design that best fitted the cornea. The first CL option was: OD: 8.6mm BCR 550 μm RZD 33° LZA, OS: 8.6mm BCR 575 μm RZD 32° LZA. After one night of lens wear the patient exhibited a high value of overrefraction and poor centration in OS. After several follow-up visits in which the CL of the OS was changed, it was finally decided to refit the patient with the following lens parameters: OS: 8.6mm BCR 525 μm RZD 33° LZA. The patient was appointed for a follow-up in one week.
Once the best unaided VA with spherical CL (OD: 8.6mm BCR 550 μm RZD 33° LZA, OS: 8.6mm BCR 525 μm RZD 33° LZA) were obtained OD: 20/25 OS: 20/28, we sent the manufacturers the diagnostic lens data, last topography of both eyes and overrefraction to obtain dual axis lens parameters. The manufacturer calculated and sent us the lenses.
Dual axis lens parameters selected for our patient was as follows: OD: 8.6/8.6mm BCR 550/600 μm RZD 33/33° LZA, OS: 8.6/8.6mm BCR 525/600 μm RZD 33/33°. Change from symmetric design to Dual Axis lens was consecutive. However, we waited 10 days to take a decision to avoid distorting the results.
First follow-up visit took place when the lenses had been worn only one night. The examination details of this visit were: manifest subjective refraction: OD: —1.00 × 180° OS 0.00 D. Unaided visual acuity: OD: 20/33, OS: 20/20.
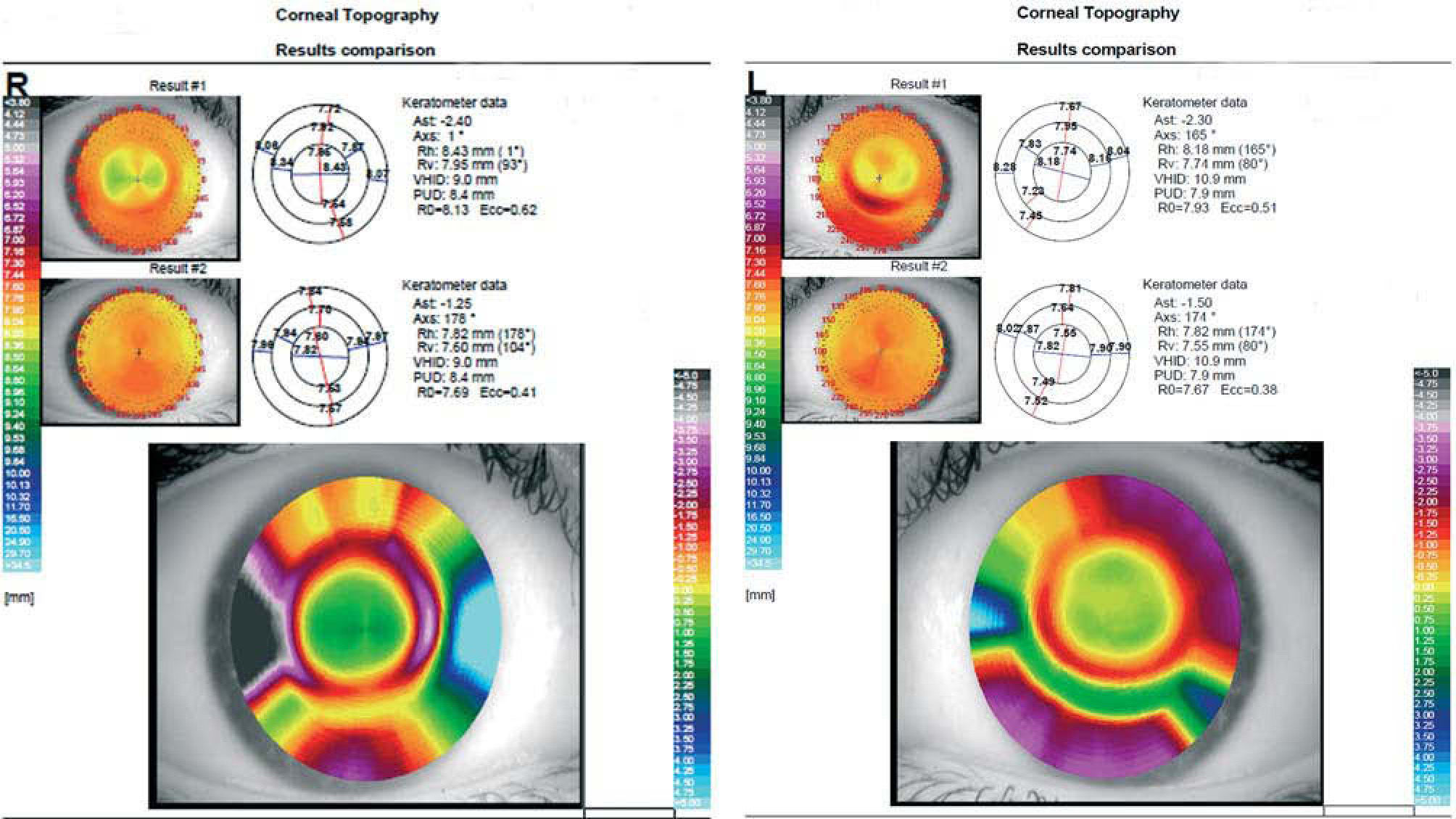
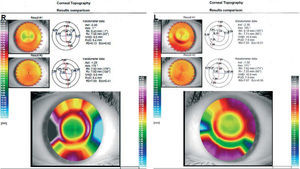
In the postwear corneal topography (Figure 2) it was observed that OD showed a well-centered treatment zone, whilst OS lens exhibited a poor centration.
The first follow-up visit gave these results: OD: VA had diminished when comparing with the obtained with the spherical lens (value was 20/33), however lens fitting was better. OS: Although OS exhibits a 20/20 VA, lens centration was poor. The patient was seen for follow-up 10 days later with the same examination results. Therefore, it was decided to use these new parameters: OD: to flatten RZD and change LZA to improve fitting and VA results, OS: to change LZA to improve lens centration. After several follow-up visits the final prescription lenses were designed as follows: OD: 8.6/8.6mm BCR 525/575 μm RZD 34/34° LZA, OS: 8.6/8.6mm BCR 525/600 μm RZD 34/34° LZA. Unaided VA after one night of wearing of this lens was: OD: 20/16, OS: 20/16. Lens-positioning showed a well-centered treatment zone. The patient was seen for follow-up 2 weeks later.
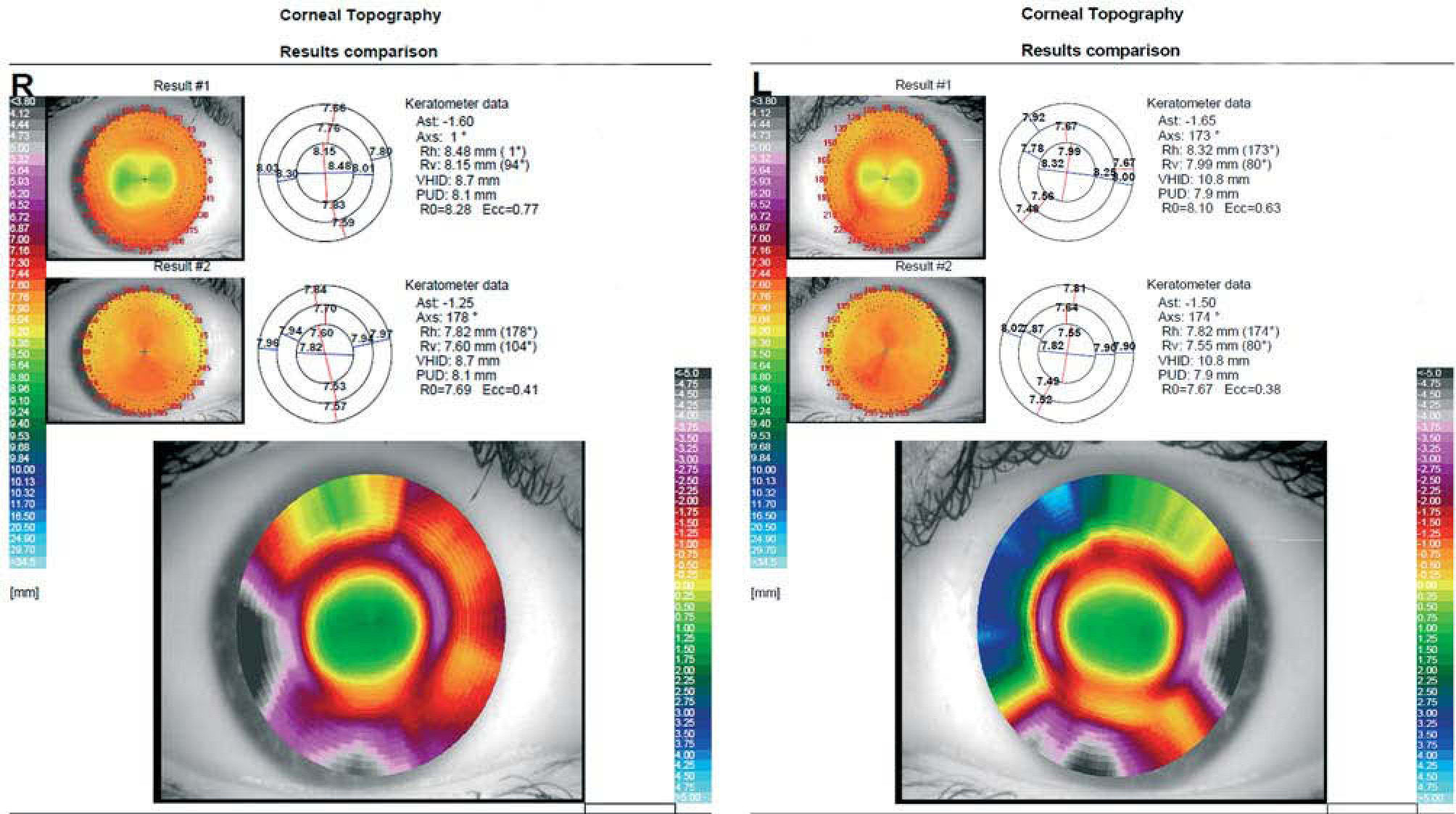
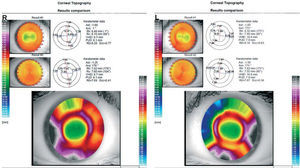
The examination details after 2 weeks of night wearing of the lens were: manifest subjective refraction: OD: 0.00 D, OS: 0.00 D. Unaided VA: OD: 20/16, OS: 20/16. Two weeks postwear, corneal topography showed an almost perfect CL fitting (Figure 3).
In this follow-up revision the patient exhibited both great unaided VA: OD: 20/16, OS: 20/16, and fitting in both eyes. Those lenses were settled as our final prescription. The patient was checked again in one month and then every three months.
Last follow-up took place one-year after lens fitting. In this visit slit-lamp evaluation did not show any remarkable problem, the patient was satisfied and felt comfortable with the lens and with her unaided VA.
DiscussionOK have been used by practitioners since Jessen tried to reduce eye refractive error with a rigid CL.4 At first, patients worn the lenses during waking hours, being then able to enjoy an improved unaided VA during the evening.5
After that, the technique was reported to be safe but its effect was temporary.6,7 Then, the development of the reverse-geometry lenses improves the speed of corneal changes, and new lens materials with high oxygen permeability make possible to wear the lenses while patients are sleeping, which allowed practitioners to obtain a higher degree of corneal reshaping, thus resulted in an increased interest in OK.8
Mountford was the first to report benefits of overnight OK.9 After him, other authors have reported clinical benefits of the technique and the amount of reduced myopia. Sorbara et al, showed an important reduction of myopia lasting 4 weeks, using Paragon CRT® CL.10
Traditionally OK have been used mainly to reduce myopia, but nowadays there are some lens designs that also reduce other refractive errors, such as hyperopia11 or astigmatism12.
The main difference between CRT and previous OK is that CRT involves the use of a specially designed high-Dk/L RGP lens manufactured by Paragon. Villa-Collar et al (2009) have described a significant corneal flattening as soon as 30 minutes after fitting this type of CL.13 Other authors1 have showed that CRT can successfully correct the 80% of the myopic refraction after the first night of lens wear, which is a similar period to that observed for patients 1 day after laser in situ keratomileusis (LASIK); in this case we showed an important VA improvement after one night of CRT Dual Axis lens wearing, which means this new lens can correct a similar amount of myopic refraction than previous Paragon CRT models after one night of lens wear.
In our case, symmetric design failure may be due to corneal peripheral astigmatism; although corneal astigmatism is within the normal range, we see that corneal astigmatism is limbus-to-limbus rather than central; this fact prevents the lens to land peripherally 360 degrees around the cornea, so the desired topographical changes cannot occur. Dual Axis lens allow us to improve lens centering and to obtain a well-centered treatment zone.
Comparison between CRT symmetric design and CRT Dual Axis geometry, reveals that this new lens allows for modulation of the lens periphery in two meridians when corneal elevation or curvature differences limit the success of a fit (The design incorporates a dual return zone depth system with a shallower return zone depth to align the flat corneal meridian and a deeper return zone depth to align the steeper corneal meridian). Those lenses permit independent manipulation of a second RZD and LZA, that doesn’t alter the dimension found optimum in a first meridian. Whilst in symmetric design, if we change a value (RZD, LZA or both), this is varied throughout the lens diameter.
Gonzalez-Méijome et al (2007) have analyzed the fitting success rates of nomograms provided by the manufacturer to choose the first CRT lens to be fitted.3 They showed that 92% of the fittings were achieved by changing only two parameters or less. In our case, using CRT Dual Axis Lens, we must change two parameters in one eye and three on the other, so in this case CRT Dual Axis Lens shows a similar relationship between the first selected lens and the lens finally prescribed to that showed for previous CRT models.
In this case we have shown a maintained unaided VA during 1 year of CRT dual axis treatment, showing those CL as a good option in the presence of poor centering and/or low unaided VA instead of the amount of astigmatism
An advantage of OK over surgical procedures may be the temporality of changes.9 If a patient leaves the treatment, the refraction will return to baseline; this fact could be important for presbyopic patients who want to reduce the amount of compensated myopia to improve unaided VA for near vision. Moreover, for CRT treatment, refractive error does not have to be stable, making it an useful treatment for childs or youngs.
We thank the patient for giving us permission to publish this case report and Dr. Marta Agudo-Barriuso for her kind assistance with English.