A 64-year-old man complained of difficulty with far vision in the right eye after blunt trauma by his hand during sleep. He had undergone uneventful phacoemulsification and intraocular lens (IOL) implantation of both eyes one week before the event. On slit lamp examination, the anterior chamber was shallow compared to postoperative one day or the left eye. After mydriasis, IOL position was perfect, within the capsulorrhexis margin, and no haptics were protruded. SE of his right eye was −4.00 diopter after trauma, although spherical equivalent (SE) of both eyes was near emmetropia one day after cataract surgery. We decided on IOL reposition or exchange. Intraoperatively, we pushed the IOL posteriorly; the IOL was vaulted posteriorly, as expected. After surgery, his SE was +0.25 with the same diopter IOL. We report the case on the possibility of 4-point haptic IOL vaulting anteriorly by blunt trauma within the capsular bag.
Se presenta el caso de un varón de 64 años con dificultad en visión lejana en el ojo derecho tras tratamiento contuso con su propia mano durante el sueño. Se había sometido sin incidentes a una facoemulsificación y a un implante de lentes intraoculares en ambos ojos una semana antes del suceso. En el examen de la lámpara de hendidura la cámara anterior se mostraba plana en comparación al día siguiente a la operación así como en comparación al ojo izquierdo. Tras la midriasis, la posición de la lente intraocular era perfecta dentro del margen de la capsulorrhexis, sin sobresalir los hápticos. El equivalente esférico de su ojo derecho era de -4,00 dioptrías tras el traumatismo, aunque el equivalente esférico de ambos ojos era casi emetrópico al día siguiente de la cirugía de catarata. Se optó por la reposición o cambio de la lente intraocular. Intraoperatoriamente la lente intraocular fue empujada posterioremente, y dicha lente se posicionó posteriormente, según lo previsto. Tras la cirugía, el equivalente esférico era de +0,25 empleando la misma potencia de lente intraocular. En este caso se reporta la posibilidad de un desplazamiento anterior de una lente intraocular con hápticos de 4 puntos, debido a un traumatismo contuso dentro del saco capsular.
In recent decades, technological developments in cataract surgery have progressed toward the use of microincisions. According to developments, new intraocular lens (IOL) designs and biomaterials are available. The Akreos MI60 (Bausch & Lomb) IOL is among a new generation of flexible IOLs, designed thinner than 30% compared to its patent design. This is a single-piece acrylic IOL consisting of a 6.0mm optic and 4 flexible haptics with a posterior angulation of 10°. Most studies on the Akreos MI60 IOL report successful outcomes1; however, despite the stability of capsular bag implantation, some complications have been reported with the Akreos MI60 IOL.2 Here, we present a case of an Akreos MI60 IOL vaulting anteriorly within the capsular bag after blunt trauma.
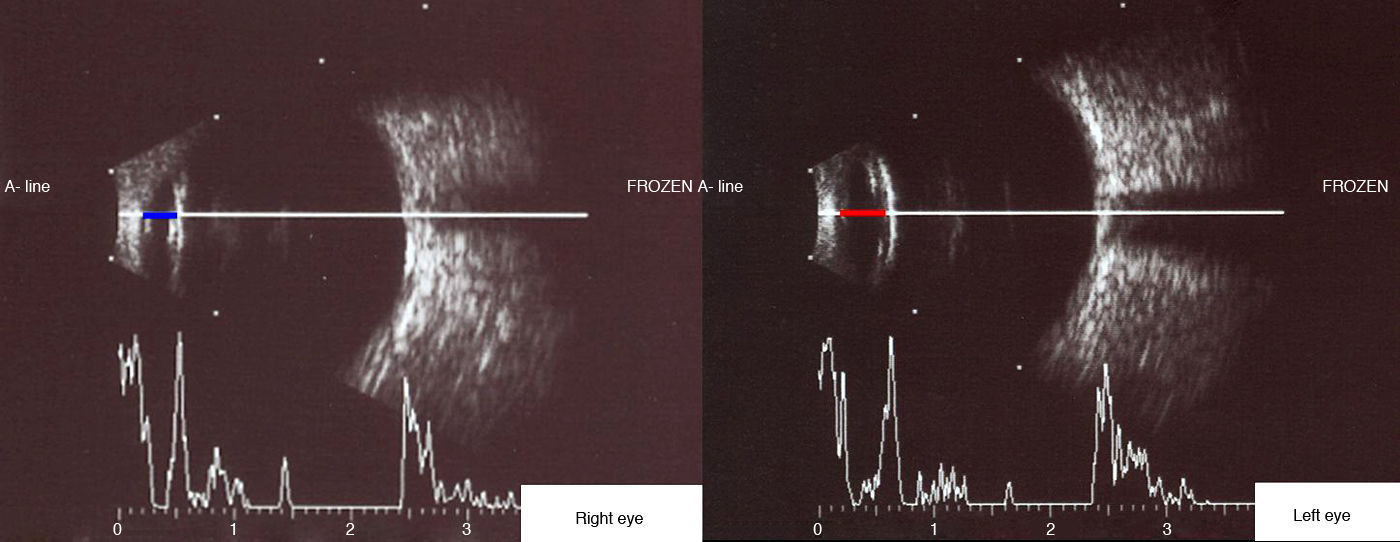
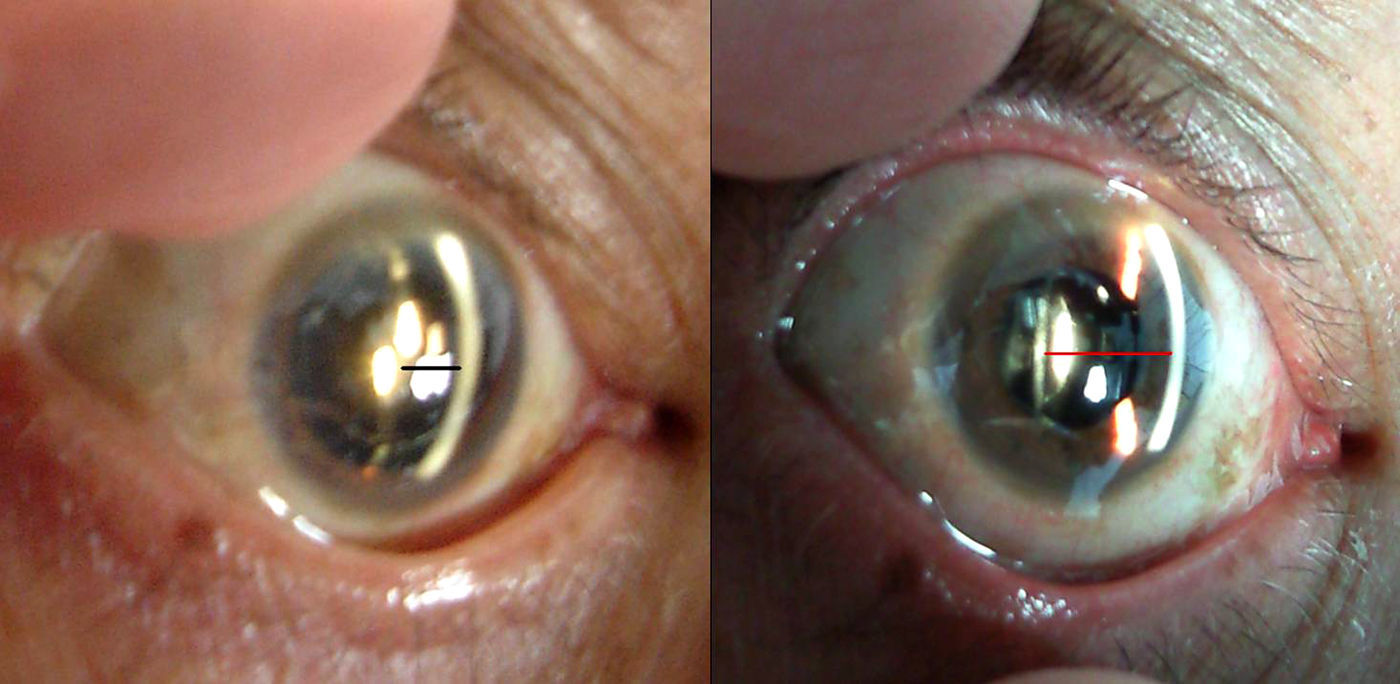
A 64-year-old man complained of difficulty with far vision in the right eye after blunt trauma by his hand during sleep. He underwent uneventful cataract phacoemulsification and in-the-bag implantation of the Akreos MI60 IOL (+22.0D) of both eyes one week before the event. The patient was in good health, without significant systemic or ocular disease. On slit lamp examination, the anterior chamber was shallow compared to postoperative one day or the left eye. After mydriasis, IOL position was perfect, within the capsulohexis margin, and no haptics of the IOL were protruded. Although spherical equivalent (SE) of both eyes was almost emmetropia one day after cataract surgery, SE of his right eye was −4.00 and SE of his left eye was −0.375 diopter after trauma. Best corrected visual acuity was 20/20 in both eyes. B-scan showed shallower anterior chamber depth in his right eye than in his left eye (Fig. 1).
We decided to perform surgery for IOL reposition or exchange. After retrobulbar anesthesia and routine dressing, we injected viscoelastics into the anterior chamber through the previous corneal incision site. We then pushed the IOL posteriorly; the IOL was vaulted posteriorly, as expected. We thought that IOL repositioning could solve the patient's problem; however, we performed IOL exchange due to possible defectiveness of the IOL and the patient's desire. The IOL was removed after division by an IOL cutter, paying attention not to change the upside downward, in order to check IOL position after surgery. We performed uneventful implantation of the same diopter Akreos MI60 IOL. One week after surgery, his SE of the right eye was +0.25 diopter with the same diopter Akreos MI60 IOL and the anterior chamber of his right eye was deepened (Fig. 2). No postoperative complications developed.
There have been some reports of capsule contraction syndrome or capsulorhexis phimosis with in-the-bag implantation of the single-piece IOL consisting of a central optic and 4 flexible haptics.2,3 However, there have been no case reports of 4-haptic-single piece IOLs with posteriorly vaulted optics vaulting anteriorly by mild trauma.
According to the manufacturer's instructions, Akeos MI60 IOL is based upon the 4-point haptic design of the Akreos AO with a novel haptic shape to compensate for the reduction in the thickness of the lens. Thinner yet with a design that complements the stability, Akeos MI60 IOL shows stable results in normal condition1 but as this case, it can be vulnerable in traumatic condition compared to the conventional thick IOL.
Instability of the IOL could be associated with the time of trauma after cataract surgery as well as the design. Hideyuki et al.,4 showed that the anterior capsule first comes into contact with the IOL optic about 6 days after surgery. Full contact of the posterior capsule is then completed within approximately 11 days with the acrylic IOL. In our case, trauma occurred 7 days after cataract surgery, which was not enough time for completion of capsular contact.
Koeppl et al.5 reported myopic eyes with large capsular bags showed less IOL shift in the early postoperative period than hyperopic eyes with smaller capsular bags. They observed a linear forward movement of the IOL during the first postoperative week. Our patient underwent blunt trauma one week after cataract surgery, so this time point was prone to the optic-haptic junction bowing forward. He had normal range of axial length, there was little influence of capsular bag size.
When we exchanged the IOL, it was removed successfully without capsular damage. We removed the IOL carefully. Under microscopy, we examined the removed IOL, including haptic shape, and confirmed the IOL was initially inserted the correct way.
In conclusion, we described an unreported case of possible thin 4-point haptic IOL vaulting anteriorly by blunt trauma. To the best of our knowledge, no case of these characteristics has been reported. It is important to scrutinize haptic–optic junction design of IOL in the light of this newly described complication. Postoperative care after cataract surgery is important, and there is not an exception to use eye shield at bedtime until the IOL becomes stable.