Background/Objective: To examine the effect of using the DSM-5 preschool criteria to diagnose posttraumatic stress disorder (PTSD) in school-age children (ages 7-11). Method: Children exposed to Hurricane Ike (N=327) were assessed for symptoms of PTSD and other trauma-related factors eight months post-disaster. Results: About twice as many children were identified as having PTSD using the DSM-5 preschool criteria compared to the DSM-5 adult criteria. The preschool criteria identified all children diagnosed by the adult criteria and many additional children. Although children who met both the adult and the preschool criteria reported the most functional impairment, children identified by the preschool criteria only reported greater impairment than children not diagnosed. The effect of including impairment in the diagnostic criteria was more marked for the preschool criteria than for the adult criteria. Additionally, PTSD defined by the preschool criteria was significantly associated with more PTSD risk factors than PTSD as defined by the adult criteria. Model fit was similar for both sets of criteria. Conclusions: The preschool criteria may be advantageous for screening for PTSD risk in school-age children. Further research is needed to optimize developmentally-appropriate PTSD criteria for school-age children.
Antecedentes/Objetivo: Examinar el uso los criterios preescolares del DSM-5 para diagnosticar el trastorno de estrés postraumático (TEPT) en niños de edad escolar (7-11 años). Método: Niños expuestos al huracán Ike (N=327) fueron evaluados respecto a los síntomas de TEPT, ocho meses después del desastre. Resultados: Aproximadamente el doble de niños fueron diagnosticados con TEPT usando los criterios preescolares del DSM-5 comparado a los de adultos. Los criterios preescolares identificaron todos los niños diagnosticados usando los criterios de adultos y muchos más. Aunque los niños que cumplieron ambos criterios reportaron el mayor deterioro funcional, los niños identificados solamente por los criterios preescolares reportaron más deterioro que los niños no diagnosticados. El efecto de incluir el deterioro en los criterios diagnósticos fue más intenso para los criterios preescolares. Además, el TEPT definido por los criterios preescolares fue asociado significativamente con más factores de riesgo que TEPT definido por los criterios de adultos. El ajuste del modelo fue similar en ambos conjuntos de criterios. Conclusión: Los criterios preescolares pueden ser útiles para detectar el riesgo de TEPT en niños de edad escolar. Se necesitan más investigaciones para optimizar los criterios de TEPT de acuerdo al nivel de desarrollo para los niños en edad escolar.
Posttraumatic stress disorder (PTSD) is frequently diagnosed in children postdisaster (Pfefferbaum, Jacobs, Griffin, & Houston, 2015). However, research on the diagnosis of PTSD has historically focused on adults. Recently, increasing attention has been paid to the diagnosis of PTSD in very young children (preschool-age youth). Because some aspects of the traditional PTSD criteria (i.e. DSM-IV) may not be appropriate for young children (Scheeringa, Zeanah, & Cohen, 2011), DSM-5 released new PTSD criteria developed for children ages six and younger (i.e. the preschool criteria; American Psychiatric Association, APA, 2013). At present, school-age children (ages 7-11 years) are diagnosed using the DSM-5 adult criteria, despite evidence that their developmental level might make their PTSD presentations more similar to that of preschool children than adults (Danzi & La Greca, 2016). This study examined the effect of using the DSM-5 preschool criteria in a sample of school-age children exposed to a natural disaster.
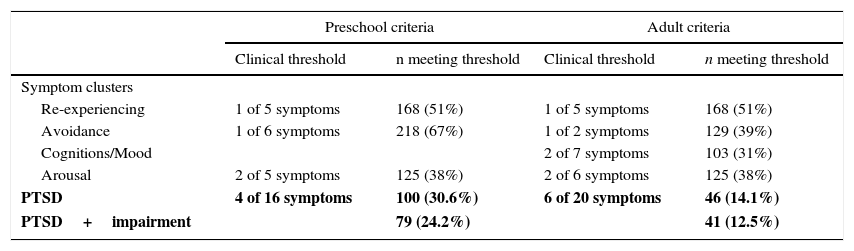
There are several reasons why the preschool criteria may be more suitable for school-age children than the adult criteria. Although factor analytic studies of adolescents and adults have supported a four-factor model of PTSD (re-experiencing, avoidance, cognitions/mood, and arousal), a three-factor model (re-experiencing, avoidance, arousal) is commonly found to be best-fitting in children (Friedman, Resick, Bryant, & Brewin, 2011; Scheeringa et al., 2011). The four-factor model requires a higher threshold of endorsed symptoms, which may be too stringent for children whom may have less insight about their symptoms. Thus, the three-factor model of PTSD used in the preschool criteria (see Table 1) may be more appropriate for school-age children than the four-factor model used in the adult criteria.
Children meeting clinical thresholds for PTSD symptom clusters.
| Preschool criteria | Adult criteria | |||
|---|---|---|---|---|
| Clinical threshold | n meeting threshold | Clinical threshold | n meeting threshold | |
| Symptom clusters | ||||
| Re-experiencing | 1 of 5 symptoms | 168 (51%) | 1 of 5 symptoms | 168 (51%) |
| Avoidance | 1 of 6 symptoms | 218 (67%) | 1 of 2 symptoms | 129 (39%) |
| Cognitions/Mood | 2 of 7 symptoms | 103 (31%) | ||
| Arousal | 2 of 5 symptoms | 125 (38%) | 2 of 6 symptoms | 125 (38%) |
| PTSD | 4 of 16 symptoms | 100 (30.6%) | 6 of 20 symptoms | 46 (14.1%) |
| PTSD+impairment | 79 (24.2%) | 41 (12.5%) | ||
Note. Each cell describes the minimum clinical threshold (in italics) required for each cluster and the number of children (% of sample) meeting the threshold for each cluster. Children must meet thresholds for all clusters (three for preschool criteria; four for adult criteria) to receive a diagnosis of PTSD. For the preschool criteria, either an avoidance or a cognitions/mood symptom may be present to meet the minimum threshold for that cluster. Note that for the adult criteria arousal cluster, one symptom (reckless or self-destructive behavior) was unable to be assessed. The final row indicates that number and percentage of children that would be diagnosed with PTSD when including the requirement of impairment along with the criteria.
Further, the preschool criteria place less emphasis on symptoms requiring advanced cognitive development; in this domain, school-age children may be more similar to preschool children than to adults. The preschool criteria combine and reduce the symptom clusters for avoidance and cognitions/mood, both of which contain many highly internalized or cognitively sophisticated symptoms deemed difficult for young children to report or experience (Scheeringa et al., 2011). For example, symptoms such as persistent negative beliefs (about oneself/others/world) may be difficult for young children with emerging verbal skills to report given their developing cognitive capacities. Such symptoms also may be challenging for school-age children. In fact, many studies have indicated that school-age children are less likely to report symptoms found in the DSM-IV avoidance and DSM-5 cognitions/mood clusters (e.g., Danzi & La Greca, 2016; Keppel-Benson, Ollendick, & Benson, 2002; La Greca, Silverman, Vernberg, & Prinstein, 1996; McDermott & Cvitanovich, 2000). For example, among children in motor vehicle accidents, only 8% met criteria for the DSM-IV avoidance cluster (compared to 40% for re-experiencing and 28% for arousal). Because all clusters are required for diagnosis, this resulted in only 8% of children being diagnosed with PTSD (McDermott & Cvitanovich, 2000). Less emphasis on avoidance and cognitions/mood symptoms, as done in the preschool criteria, would likely result in more children being identified with PTSD.
Why were the more developmentally-sensitive preschool criteria not extended to school-age children? One critical factor was the dearth of research on PTSD diagnostic considerations in school-age children. Although alternative diagnostic criteria have been well-studied in preschoolers, this hasn’t been the case for school-age children (Scheeringa et al., 2011). In the absence of data for this age group, the adult criteria were extended to school-age children. However, it is not known how well the adult model fits school-age children and, in fact, there is some evidence to suggest that the preschool criteria may be more developmentally-appropriate for school-age children (Scheeringa et al., 2011).
This study investigated the effects of extending the preschool PTSD criteria to school-age children (ages 7-11 years). To eliminate potential confounds from pooling multiple types of trauma, we investigated children exposed to the same traumatic event—a natural disaster. The study builds on and extends our findings that different criteria for identifying PTSD (e.g. DSM-IV, DSM-5, and ICD-11) show low agreement (Danzi & La Greca, 2016). Further, we found that some aspects of the DSM-5 (adult) criteria may not be appropriate for children (e.g., the requirement of the fourth symptom cluster emphasizing changes in cognitions; Danzi & La Greca, 2016). The current study investigates the preschool criteria as a potential alternative to using the DSM-5 adult criteria with school-age children.
Our first aim was to investigate rates of “probable” PTSD using diagnostic algorithms based on clinical thresholds for the DSM-5 adult and preschool criteria (see Table 1). We hypothesized that more children would be identified using the preschool criteria than the adult criteria. To provide context, we also provided rates of PTSD for DSM-IV. Our second aim was to compare the functional impairment of children identified by the adult and preschool criteria. We hypothesized that children identified by the adult criteria would report more severe impairment, based on the more stringent clinical thresholds. Our third aim was to evaluate whether the children identified by each set of criteria had characteristics expected of children likely to be diagnosed with PTSD. To address issues of criterion validity, we assumed that “true” PTSD cases would be more likely to be predicted by risk factors identified in prior research as being associated with PTSD. Thus, we determined the extent to which the adult and preschool criteria were predicted by these risk factors. In prior studies, girls have been found to be more at risk for developing PTSD than boys (Banks & Weems, 2014; McLaughlin et al., 2013; Pfefferbaum et al., 2015). Similarly, research indicates that ethnic/racial minority children are more at risk for developing PTSD than White children (La Greca, Silverman, Vernberg, & Prinstein, 1996; Pfefferbaum et al., 2015). Additionally, hurricane-related life threat (perceived threat and the number of life-threatening events), hurricane-related loss/disruption, and other major stressful life events have been found to be related to PTSD symptom severity (Banks & Weems, 2014; La Greca et al., 1996; Pfefferbaum et al., 2015). Based on our expectation that the preschool criteria would capture the PTSD construct well in school-age children, we hypothesized that the preschool criteria would be predicted by as many or more risk factors for PTSD compared to the adult criteria. Our final aim was to evaluate model fit for the adult and preschool criteria using confirmatory factor analyses. Because the preschool and adult models are not nested, they could not be directly compared. We expected good fit for the preschool model, which has three factors (re-experiencing, avoidance/cognitions/mood, and arousal), given the support for three factors in previous child research. It was unclear whether the adult model with four factors (re-experiencing, avoidance, cognitions/mood, and arousal) would fit children's responses.
MethodParticipantsParticipants were 327 children (ages 7-11) from all six elementary schools in Galveston, Texas (USA) that were directly in the path of Hurricane Ike. This hurricane was at the upper end of Category 2 intensity when it made landfall in Texas in September 2008. Hurricane Ike was responsible for 103 deaths and is considered among the most costly hurricanes in U.S. history (Berg, 2008). Participants were racially/ethnically diverse (36% Hispanic, 27% White, 19% Black, 18% Other/Mixed) and 52% were female.
ProceduresStudy procedures were approved by Institutional Review Boards for the University of Miami and University of Texas Medical Branch, as well as the Galveston Independent School District. Parent consent and child assent were obtained prior to participation. Questionnaires were administered to groups of children, with all items read aloud to children and multiple team members available to assist them. Children were assessed eight months postdisaster. Additional procedural details are available elsewhere (La Greca, Lai, Joormann, Auslander, & Short, 2013; Lai, La Greca, Auslander, & Short, 2013).
MeasuresThe primary study measures assessed demographics (gender, age, race/ethnicity), hurricane exposure, hurricane-related and life stressors, impairment, and PTSD symptoms, as described below. All measures were completed by child report.
Life Threat and Stressors. The Hurricane Related Traumatic Experiences–Revised (HURTE-R; La Greca et al., 1996) assessed life threat and postdisaster stressors. The full measure contains 34 items about hurricane experiences. However, only the following subscales were used in this study: Perceived life threat (e.g. thinking you might die during the hurricane; an item scored Yes=1, No=0), actual life threat (e.g. hit by an object; 6 Yes/No items; scores ranged from 0-6), and immediate loss/disruption (e.g. home destroyed; 10 Yes/No items; scores ranged from 0-10). Internal consistency was acceptable (α=.77) in this sample. Additionally, a short version of the Life Events Checklist (LEC; Johnson & McCutcheon, 1980) assessed major life events that happened since the hurricane (e.g. divorce, death of family member) using 14 items with Yes/No response options. Items were summed to yield possible scores ranging from 0 to 14, with higher scores indicating more life events. Both the LEC and HURTE-R have been used with youth in prior disaster research (Banks & Weems, 2014; La Greca et al., 1996).
Impairment. Functional impairment was measured using items adapted from the Anxiety Disorders Interview Schedule for DSM-IV: Child Version (ADIS-C; Silverman & Albano, 1996). Four items using a four-point scale (0=None to 3=Very Much) assessed how much PTSD symptoms caused by the hurricane interfered with functioning with friends, family, school, and “enjoying or doing other things”. These items were summed to yield possible scores ranging 0 to 12, and a cutoff score of 3 was used to indicate impairment. Internal consistency was good (ordinal α=.84).
PTSD Symptoms. The Posttraumatic Stress Disorder–Reaction Index, Revision 1 (PTSD-RI-R; Steinberg, Brymer, Decker, & Pynoos, 2004) is one of the most widely-used instruments for assessing PTSD symptoms in youth who have experienced trauma, including natural disasters (Keppel-Benson et al., 2002; La Greca, Lai, Llabre et al., 2013; Lai et al., 2013). It has strong psychometric properties, with test-retest reliability of .84 and alphas around .90 for several studies (Steinberg et al., 2004, 2013). Internal consistency was high in this sample (ordinal α=.92). The PTSD-RI-R includes 22 items on a 3-point scale (0=None of the time, 2=Some of the time, 4=Most of the time). We used a conservative approach to indicate symptom presence (consistent with recommendations; Steinberg et al., 2004), and counted the symptom as present if the child endorsed “most of the time”.
The algorithm and items used to evaluate the DSM-5 adult criteria have been previously described in detail (Danzi & La Greca, 2016; La Greca, Danzi, & Chan, 2017). In brief, all 20 symptoms were assessed by the PTSD-RI-R except three, which were negative beliefs, negative emotional state, and reckless/self-destructive behavior. Thus, we used items from the Children's Depression Inventory (CDI; Kovacs, 1981) and the Revised Children's Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1985) to approximate these symptoms. The negative beliefs symptom was assessed by an item from the CDI and negative emotional state was assessed by an item from the RCMAS. No item had adequate face validity to represent reckless/self-destructive behavior; thus, we were unable to assess this symptom. However, this symptom (designed to capture risky sexual behaviors and reckless driving observed in adult samples) is unlikely to be reported by many school-age children (Friedman et al., 2011; Riesch et al., 2013).
Because a self-report assessment of the DSM-5 preschool criteria was not available, symptoms were assessed using the corresponding items from the PTSD-RI-R. The preschool criteria have one unique symptom not assessed by the PTSD-RI-R: socially withdrawn behavior. An item from the RCMAS about feeling alone was used to approximate this symptom. Children who responded “Yes” were considered to meet this criterion. The symptom thresholds required to meet criteria for a cluster are described in Table 1.
Statistical analysisMost study analyses were conducted using SPSS Version 22. Missing data (<3% across study variables) were imputed using multiple imputation, specifically an iterative Markov chain Monte Carlo method that involved generating 20 imputations at an item level with 100 burn-in iterations. Reported findings were based on the pooled results of the 20 separate imputations. For aim one, we calculated rates of PTSD using diagnostic algorithms based on the adult and preschool criteria. For aim two, one-way analysis of variance (ANOVA) procedures were used to compare the level of impairment for children meeting criteria using the adult versus preschool criteria. Because the assumption of homogeneity of variances was not met, we used the more robust Welch's test and conducted post-hoc comparisons using Games-Howell. First, two separate ANOVAs (one for adult; one for preschool criteria) were conducted to compare the impairment of children identified with PTSD (as defined by the adult versus preschool criteria) to those without PTSD. Next, we compared the impairment of children identified by the preschool criteria only, the adult criteria only, both, and neither. Then, we determined rates of PTSD for the adult and preschool criteria with impairment added to the criteria. For aim three, hierarchical binary logistic regressions were used to evaluate which risk factors predicted PTSD, as defined by the adult and preschool criteria. Odds ratios and confidence intervals are reported at every step, controlling for variables entered in the model in concurrent and prior steps. Finally, for our last study aim, confirmatory factor analyses were conducted using Mplus Version 7.31. Model fit for the adult and preschool criteria was evaluated based on recommended guidelines (Kline, 2011): RMSEA<.05, SRMR<.08, CFI>.90, TLI>.90. Model fit also was considered to be good if the chi-square was non-significant and the AIC had a lower value, indicating a superior trade-off between model fit and complexity (Kline, 2011).
ResultsComparing rates of PTSD for the adult and preschool criteriaDiagnostic algorithms based on the DSM-5 adult and preschool criteria for PTSD were used to determine how many children would be identified as having PTSD based on each set of criteria (see Table 1). As hypothesized, a larger percentage of children were identified using the preschool criteria than the adult criteria. Results indicated that 100 children (30.6% of the sample) were identified with PTSD using the preschool criteria; 46 (14.1%) were identified using the adult criteria. For comparison, 50 children in this sample (15.3%) were identified using DSM-IV (Danzi & La Greca, 2016). Thus, rates of PTSD based on the preschool criteria doubled compared to rates of PTSD using DSM-IV or DSM-5 adult criteria. Findings indicated that the group identified by the preschool criteria encompassed all the children identified by the adult criteria; that is, all 46 children who met the adult criteria also met the preschool criteria. However, the preschool criteria identified an additional 54 children who were not identified by the adult criteria.
ImpairmentIn terms of the functional impairment of children identified by the adult and preschool criteria, analyses revealed that greater impairment was reported by children identified by the preschool criteria (M=5.38, SD=3.26) compared to children not diagnosed (M=1.90, SD=2.55, Welch's F[1,155.29]=90.16, p<.001). Similarly, greater impairment was also reported by children identified by the adult criteria (M=6.43, SD=3.20) compared to those not diagnosed (M=2.39, SD=2.84, Welch's F[1,57.78]=65.52, p<.001). Significant differences were found in the impairment of children identified by only the preschool criteria, those identified by both the preschool and adult criteria, and those identified by neither (Welch's F[2,82.12]=51.55, p<.001); there were no children identified by the adult criteria alone. Games-Howell post hoc comparisons (ps<.01) indicated that children identified by both the preschool and adult criteria had greater impairment (M=6.43, SD=3.20) than children identified by only the preschool criteria (M=4.48, SD=3.06). However, children identified by only the preschool criteria had greater impairment than children not diagnosed (M=1.90, SD=2.55). Because impairment is an important part of PTSD diagnosis, we also determined the effect of including impairment as part of the diagnostic criteria. Including impairment had a small effect on rates for the adult criteria, reducing the number of children identified from 46 (14.1% of the sample) to 41 (12.5%). The effect of including impairment appeared stronger for the preschool criteria, reducing the number of children identified from 100 (30.6%) to 79 (24.2%). With impairment included, the group identified by the preschool criteria still encompassed those identified by the adult criteria, as was the case when impairment was not included.
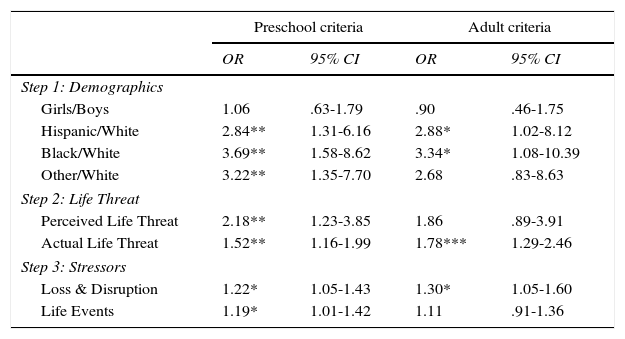
Comparison of child characteristics predictive of PTSDTo evaluate criterion validity, risk factors identified by prior research as being important for the emergence of PTSD were examined to determine how well they predicted the preschool or adult criteria (see Table 2). There was low multicollinearity (variance inflation factors below 1.5 for all predictors) and low autocorrelation (Durbin-Watson=2.01). The Hosmer and Lemeshow test indicated good fit for the preschool model (χ2[8]=8.68, p=.41) and adult model (χ2[8]=5.03, p=.75). Analyses revealed that the preschool-defined PTSD cases were predicted by more risk variables (seven) than the adult-defined PTSD cases (four), as shown in Table 2. No significant gender differences emerged for either set of criteria. However, the odds ratio for the preschool criteria was in the expected direction, whereas the odds ratio for the adult criteria was not. Significant differences emerged for Hispanic and Black children for both the preschool and adult criteria. Significant differences for other racial minority children (which included Asian, Native American, and biracial children) emerged for the preschool criteria (OR=3.22, p< .01), but not for the adult criteria (p>.05). Hurricane-related life threatening events and loss/disruption were related to both sets of PTSD criteria. However, perceived life threat was only associated with the preschool criteria (OR=2.18, p<.01). Stressful life events were associated with the preschool criteria (OR=1.32, p<.01), but not the adult criteria (p>.05).
Predictors of PTSD.
| Preschool criteria | Adult criteria | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Step 1: Demographics | ||||
| Girls/Boys | 1.06 | .63-1.79 | .90 | .46-1.75 |
| Hispanic/White | 2.84** | 1.31-6.16 | 2.88* | 1.02-8.12 |
| Black/White | 3.69** | 1.58-8.62 | 3.34* | 1.08-10.39 |
| Other/White | 3.22** | 1.35-7.70 | 2.68 | .83-8.63 |
| Step 2: Life Threat | ||||
| Perceived Life Threat | 2.18** | 1.23-3.85 | 1.86 | .89-3.91 |
| Actual Life Threat | 1.52** | 1.16-1.99 | 1.78*** | 1.29-2.46 |
| Step 3: Stressors | ||||
| Loss & Disruption | 1.22* | 1.05-1.43 | 1.30* | 1.05-1.60 |
| Life Events | 1.19* | 1.01-1.42 | 1.11 | .91-1.36 |
Note. *p<.05,**p<.01,***p<.001
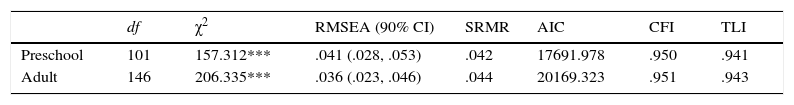
Finally, we used confirmatory factor analyses to evaluate model fit for the preschool criteria (see Table 3). We previously reported the model fit for the DSM-5 adult criteria (La Greca et al., 2017) and included those results in Table 3 as well. Models based on the preschool and adult criteria exhibited fairly similar fit. Specifically, four of the six fit indices showed evidence of good fit: the SRMR was less than .08 for both models; the CFI and TLI were greater than .90 for both models; and the RMSEA was less than .05 for both models. However, the RMSEA 90% confidence intervals generated an upper limit that was above .05 for the preschool criteria. Two additional criteria suggested a poor fit: the chi-square values were large and significant for both models, although lower for the preschool model; and the AIC values were high for both models, although lower for preschool model.
Model fit comparisons.
| df | χ2 | RMSEA (90% CI) | SRMR | AIC | CFI | TLI | |
|---|---|---|---|---|---|---|---|
| Preschool | 101 | 157.312*** | .041 (.028, .053) | .042 | 17691.978 | .950 | .941 |
| Adult | 146 | 206.335*** | .036 (.023, .046) | .044 | 20169.323 | .951 | .943 |
Note. ***p<.001; RMSEA= Root mean square error of approximation; SRMR= standardized root mean square residual; AIC= Akaike Information Criterion; CFI= Comparative Fit Index; TLI= Tucker-Lewis Index.
This study evaluated the use of the DSM-5 preschool criteria for PTSD, compared to the DSM-5 adult criteria, in a sample of trauma-exposed school-age children. We examined how the different criteria would affect rates of PTSD, the degree to which children reported functional impairment, and relationships with established PTSD risk factors; we also evaluated model fit. Overall, findings indicated that both the adult and preschool criteria identified impaired children who were likely to be at risk for PTSD, and their conceptual models had acceptable fit to the children's responses. However, the preschool criteria were more inclusive than the adult criteria.
Specifically, the preschool criteria identified over twice as many children (30.6%) as the adult criteria (14.1%). Children who met criteria for both the adult and the preschool criteria reported the most functional impairment, although children identified only by the preschool criteria also reported significantly greater impairment than those who did not meet any PTSD criteria. Further, even when functional impairment was included in the diagnostic criteria, the number of children identified using the preschool criteria still almost doubled those identified by the adult criteria. These findings suggest that the DSM-5 adult criteria may miss a substantial number of children with considerable symptoms of PTSD and functional impairment.
Our findings are consistent with the concern that traumatized children may be under-diagnosed with PTSD because their symptoms do not fit traditional conceptualizations of the disorder (Scheeringa et al., 2011; van der Kolk, 2005). Other research on PTSD prevalence supports the argument that children may be under-diagnosed. The adult lifetime prevalence rate for PTSD is 8.7% (APA, 2013). In adolescents, the lifetime prevalence is 7% in females and 5% overall (McLaughlin et al., 2013). Yet, research on school-age children (based on DSM-IV PTSD criteria) has found the lifetime prevalence to be only 0.1% (Copeland, Keeler, Angold, & Costello, 2007). The extremely low prevalence of PTSD in children seems unlikely to be due solely to lower rates of trauma exposure. The Adverse Childhood Experiences Study, which assessed childhood trauma retrospectively, found that 52.1% of their sample reported exposure to at least one form of abuse (e.g., physical, sexual) or household dysfunction (e.g., domestic violence, criminal behavior) during childhood (Felitti et al., 1998). Given the relatively high rates of childhood trauma exposure, and the discrepancy in PTSD prevalence between children and adolescents/adults, it is possible that the stringent clinical thresholds used in adult-orientated diagnostic criteria for PTSD are under-identifying PTSD in school-aged children.
Our results also indicated that the DSM-5 preschool criteria may provide an inclusive method for identifying PTSD in school-age children. This is important because DSM-IV and DSM-5 (adult criteria) have been shown to have low overlap in identifying PTSD (Danzi & La Greca, 2016; Stein et al., 2014). In this sample, there was only 71% agreement between DSM-IV and DSM-5 (adult criteria). However, we found that the preschool criteria captured all the children identified by the DSM-5 adult criteria and almost all the children (except for one) identified by DSM-IV. Thus, the preschool criteria might be used to resolve the problematic discrepancies between DSM-IV and DSM-5 by encompassing children identified by both.
Mental health providers and researchers might consider using the preschool criteria to cast a wide net for screening purposes when assessing trauma-exposed child populations. The use of clinical thresholds consistent with the preschool model of PTSD during screening might ensure that no children get “missed”, and follow-up assessments could then determine which children are exhibiting clinically significant levels of distress. It is important not to under-diagnose because PTSD is associated with numerous negative outcomes, including serious health concerns (Britvić et al., 2015). Notably, most children (70%) identified only by the preschool criteria also reported significant levels of functional impairment; thus, it may be the case that a substantial number of children who do not meet the adult criteria for PTSD would still benefit from treatment.
In addition to comparing rates of PTSD, we investigated the validity of the adult and preschool criteria, finding that the preschool criteria were associated with more risk factors (seven variables) for PTSD than the adult criteria (four variables). Importantly, perceived life threat was associated with preschool-defined PTSD, but not adult-defined PTSD. Perceived life threat is theorized to be a critical precursor to developing PTSD (Heir, Blix, & Knatten, 2016). Additionally, membership in certain racial minority groups (e.g. those from Asian, Native American, and biracial backgrounds) and stressful life events were associated with the preschool (but not the adult) criteria. These findings support our hypothesis that the preschool criteria would capture the PTSD construct well and be associated with as many or more risk factors for PTSD as the adult criteria.
Interestingly, model fit was reasonably good for both the preschool and adult criteria. Four of the six indices showed evidence of good fit for both models. However, a limitation is that the RMSEA confidence intervals were broad and the upper limit exceeded the cutoff for good fit for the preschool model. Although our findings did not yield a clearly superior set of criteria in terms of model fit, it will be important for future research to investigate the validity of the preschool and adult criteria in school-age children by comparing them to other indicators of PTSD, such as clinician diagnosis.
Although this study provided an important investigation of the potential effects of extending the preschool criteria for PTSD to school-age children, several limitations should be noted. One limitation was that the study relied on children's self-reports of their PTSD symptoms. Although clinical interviews or parent-reported data may have yielded different findings, it is noteworthy that child-report has been found to correlate with PTSD diagnosis whereas parent-report does not (Shemesh et al., 2005). Another limitation is that three symptoms (negative beliefs, negative emotional state, and socially withdrawn behavior) were approximated using items from the CDI and RCMAS and one symptom (reckless/self-destructive behavior) was unable to be assessed. However, this latter symptom was designed to capture behaviors such as reckless driving and risky sexual behaviors observed in older populations (Friedman et al., 2011), which likely do not occur or have extremely low prevalence in preadolescent child samples (Riesch et al., 2013). Still, it will be important for future research to use measures developed and validated to assess the preschool and adult criteria, as they become available for future disaster-exposed samples. Finally, this study focused on children exposed to a natural disaster and thus the findings may not generalize to other types of child trauma exposure. Future research should evaluate these issues.
In conclusion, this study evaluated the effects of using lenient clinical thresholds for assessing PTSD, based on the DSM-5 preschool model, with trauma-exposed school-age children. It appears that using the preschool criteria may result in many more children being identified with PTSD than the adult criteria, and yet many of the children identified by the preschool criteria report substantial impairment. Importantly, findings highlight the need for future research to investigate school-age children as a group distinct from adolescents and adults, and to take their developmental stage into consideration when establishing clinical thresholds for diagnosing PTSD (Brewin, 2016; Scheeringa et al., 2011). In the meantime, mental health providers and researchers might consider using the preschool criteria with school-age children, at least for screening purposes, as our findings indicate that cases identified by the preschool criteria would likely encompass those identified by DSM-IV and DSM-5 (adult criteria). However, additional research is needed to establish whether it is appropriate to use the preschool criteria as the primary model for identifying PTSD in school-age children.
FundingThis research was supported by Flipse Funds, a Cooper Fellowship, and a Provost's Research Award at the University of Miami to the second author. Data collection was partially funded by general funds from the University of Miami and the University of Texas Medical Branch.
We wish to thank the Galveston Independent School District for their help and cooperation, as well as the many research team members who worked on the project. We acknowledge Dr. Beth Auslander and Dr. Mary Short for their participation in study implementation and data collection. We also thank María Jiménez Muñoz, Ashley Marchante, and Estefany Saez-Flores for their assistance with the Spanish translation.