Este estudio investigó si una intervención de autorregulación por computadora incrementa el ejercicio físico en pacientes con o sin síntomas depresivos. Fueron reclutados en Alemania un total de 361 pacientes de rehabilitación ortopédica, 36 de los cuales tenían síntomas depresivos. En un estudio cuasi experimental los individuos fueron asignados a una intervención de autorregulación o a un cuestionario en línea. Se midió la cantidad de ejercicio al principio de la rehabilitación y seis semanas después de la misma. Los síntomas depresivos fueron valorados al final de la rehabilitación. Se llevó a cabo un análisis de covarianza, controlando el ejercicio en la línea base, el sexo y la fase de evaluación. Se encontro tanto un efecto principal para los síntomas depresivos (p = 0,005) y para la intervención grupal (p = 0,011) sí como una interacción marginal de intervención x síntomas depresivos (p = 0,076). Los resultados indican que la intervención de autorregulación en ejercicio físico dentro del contexto de rehabilitación fue efectiva solamente en individuos no deprimidos. Investigaciones futuras deberían examinar cómo pueden ser diseñados programas de cambio de conducta más efectivos para individuos con síntomas depresivos.
This study investigated whether a computer-based self-regulation intervention increases physical exercise in individuals with or without depressive symptoms. A total of 361 individuals in orthopedic rehabilitation, 36 of them with depressive symptoms, were recruited in Germany. In a quasi- experimental study, individuals were allocated to either a computer-based self-regulation intervention or an online questionnaire. Exercise was measured at the beginning of rehabilitation and six weeks after rehabilitation. Depressive symptoms were assessed at the end of rehabilitation. An analysis of covariance was conducted, controlling for exercise baseline, sex, and phase of assessment. A main effect for depressive symptoms (p = .005) and intervention group (p = .011), as well as a marginal interaction of intervention x depressive symptoms were found (p = .076). Results indicate that the self-regulation exercise intervention in an orthopedic rehabilitation setting seem to be only effective in non-depressed individuals. Future research should examine how health behavior change programs can be designed more effectively for individuals with depressive symptoms.
Regular exercise is required for a long-term recovery of the physical condition of orthopedic rehabilitation patients. Nevertheless, a high percentage of patients fail to maintain prescribed exercise levels after discharge from rehabilitation (e.g., Reuter, Ziegelmann, Lippke, & Schwarzer, 2009). Some interventions targeting self-regulation techniques (i.e., action planning) have been successful in promoting exercise among orthopedic patients after rehabilitation (e.g., Lippke, Ziegelmann, & Schwarzer, 2004b). However, some self-regulation interventions have failed too (e.g., Huisman et al., 2009). One reason for a lack of effectiveness of a self-regulation intervention might be that not everyone benefits from such interventions, e.g. individuals suffering from depressive symptoms.
Individuals dealing with medical health concerns often report depressive symptoms (e.g., Bardwell & Fiorentino, 2012) and have difficulties with adherence to physical exercise (Burgos-Garrido, Gurpegui, & Jurado, 2011). A large number of individuals with orthopedic health problems experience depressive symptoms (Nickision, Boards, & Kay, 2009; Riddle, Wade, & Jiranek, 2010). Suffering from depressive symptoms is associated with sadness and loss of joviality (Watson, Clark, & Stasik, 2011). Previous research has also shown that depressive symptoms interfere with self-regulation processes regarding the engagement in exercise (Pomp, Lippke, Fleig, & Schwarzer, 2010). Common self-regulation interventions to promote physical exercise do not consider these difficulties of individuals experiencing depressive symptoms. As a consequence, these individuals might not benefit from such an intervention in the same way as individuals without depressive symptoms do. Therefore, this study investigates whether an exercise self-regulation intervention is as effective in individuals who report depressive symptoms in those reporting no symptoms.
Self-regulation interventions promote post-rehabilitation exercise
Self-regulation is defined as any effort an organism undertakes to alter its own response (Carver & Scheier, 1998) and refers to a process in which individuals try to exert control over their own thoughts, feelings, impulses, and performances. Self-regulatory strategies that foster exercise are goal setting, action planning and action control (Michie et al., 2011). Observational studies (Conner, Sandberg, & Norman, 2010; Sniehotta, Scholz, & Schwarzer, 2005; Ziegelmann, Luszczynska, Lippke, & Schwarzer; 2007) and intervention studies (Knittle, Maes, & De Gucht, 2010; Latimer, Ginis, & Arbour, 2006; Lippke et al., 2004b; Sniehotta et al., 2005) have proven the beneficial effects of these strategies to uphold regular exercise. However, some interventions targeting self-regulatory strategies failed to enhance exercise behavior (Huisman et al., 2009; Sniehotta, Gorski, & Araujo-Soares, 2010). This raises the question for potential moderators. Studying moderators reveals whether intervention effects are associated with third variables, e.g., with characteristics of participants.
A conflict of resources? Why depressive symptoms may interfere with exercise-related self-regulation
A theoretical framework that might explain an interference of depressive symptoms with self-regulation processes is the strength and energy model (Baumeister, Muraven, & Tice, 2000; Hagger, Wood, Stiff, & Chatzisarantis, 2010). Within this paradigm, self-regulation is assumed to be a global energy that is utilized on self-regulated tasks across different domains of actions. Self-regulation is conceptualized as a limited source. If the energy is used up a person reaches a state of ego-depletion. Strong usage of self-regulation in one action domain can cause self-regulation failure in other domains. The regulation of negative affect (i.e., regulation of depressive symptoms) as well as symptoms of stress and fatigue demand lots of self-regulation energy and thus facilitate ego-depletion (Hagger et al., 2010; Tice & Bratslavsky, 2000). If individuals with depressive symptoms have depleted resources then they might struggle to adopt self-regulation strategies regarding exercise behavior. Common self-regulation interventions do not consider the parallel management of depressive symptoms and health behavior (Detweiler-Bedell, Friedman, Leventhal, Miller, & Leventhal, 2008) and are therefore not tailored to the particular situation of individuals dealing with depressive symptoms. Differential effects of such self-regulation interventions in individuals with and without depressive symptoms might therefore be likely.
Aims
The objective of this study was to investigate whether a computer-based self-regulation intervention during rehabilitation is effective in promoting post-rehabilitation exercise in patients with and without depressive symptoms. We expected that the effectiveness of the intervention is moderated by depressive symptoms, i.e., that individuals without depressive symptoms respond better to the intervention (i.e., have a higher increase in behavior after rehabilitation) in comparison to those screened positive on depressive symptoms.
Method
Participants and procedure
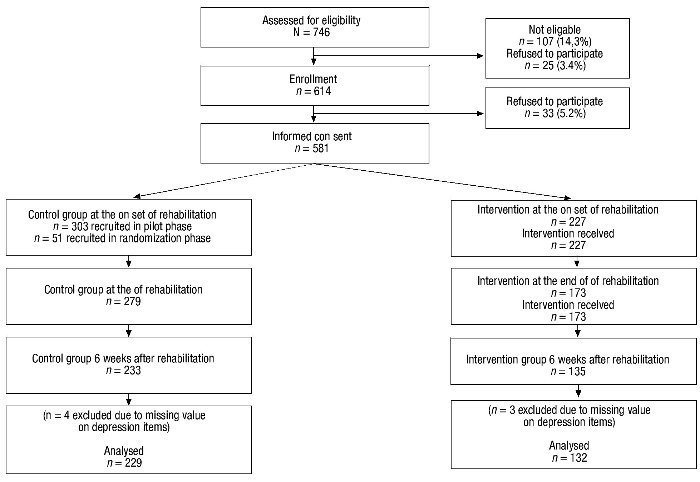
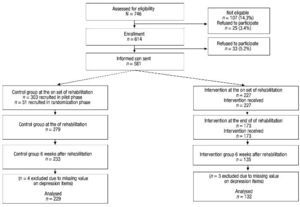
Study participants were recruited at the onset of their rehabilitation in two orthopedic rehabilitation clinics in Germany. The regular clinic program comprised a complex regimen of medical and physiotherapeutic therapies. A self-regulatory online intervention was provided to prepare rehabilitation patients to perform exercise on a regular basis after discharge. Trained project workers informed the patient about the study and patients were asked to sign an informed consent. Participants were assigned to an intervention or control group and received either an online questionnaire followed by a computer-based exercise intervention or an online questionnaire only (see Fig. 1). The uneven sample size of the control and the intervention group is due to a two-phase recruitment of the control-group. In a first phase, a pilot sample was recruited. All participants of the pilot sample filled out the online questionnaire only. In the second phase, individuals were randomly assigned to the intervention or control group by a computer algorithm. Participants of the pilot sample were compared to participants who were randomized to the control group during the main trial by using analyses of variance (ANOVAs) for continuous measures, and χ2-tests for categorical measures. Differences between the groups were found on physical exercise T1 and educational background. Individuals of the randomized control group sample reported higher levels of physical exercise at T1 (Mrandomized control group = 235.90, Mpilot sample control group = 93.60; t (54) = -3.8; p ≤ .001) and were less likely to have a high school degree (nrandomized control group = 28, npilot sample control group = 210; χ2(1) = 4.60; p ≤ .05) than individuals in the pilot sample control group. The groups did not differ with regard to sex, age, depressive symptoms, occupational status, and partner status. To increase power, the pilot sample and the randomized control group were merged into one control group in the present study. Thereby, a quasi-experimental design was applied. However, to consider differences between the two groups phase of assessment was included as a covariate in the main analysis.
Figure 1 Flowchart of participants progress through the study phases. Note. aExcluded as inclusion criteria were not met (i.e., being capable of exercising on their own, able to fill out a computer-based questionnaire, being not too handicapped to write and having sufficient literacy); brefused to participate and did not show up at the appointment; crefused to participate due to time constraints, concerns regarding protection of data privacy, and other reasons not communicated to study assistant.
The questionnaire or/and the intervention were provided at the beginning (Time 1; T1) and at the end of their rehabilitation stay (Time 2; T2). About six weeks after rehabilitation (Time 3; T3), individuals were contacted a third time and assessments were conducted via Computer-Assisted Telephone Interviews (CATI). Ethical approval was granted by the Ethics Commission of the German Psychological Association.
At T1, 581 patients participated in the study. At the end of the rehabilitation (T2), 440 patients (75.70% of T1) took part, and a total of 63.30% of the baseline sample participated in the assessment at T3. A total of 7 individuals were excluded due to missing values on the depression items. The longitudinal sample (T1, T2, T3) consisted of 361 individuals (see Fig. 1).
Mean age of the longitudinal sample was 48.40 years (SD = 10; age range: 21-76 years), and the sample consisted of more women (64.80%) than men. Of all participants, 73.40% were living with a partner, and 66.80% reported to have a high school degree.
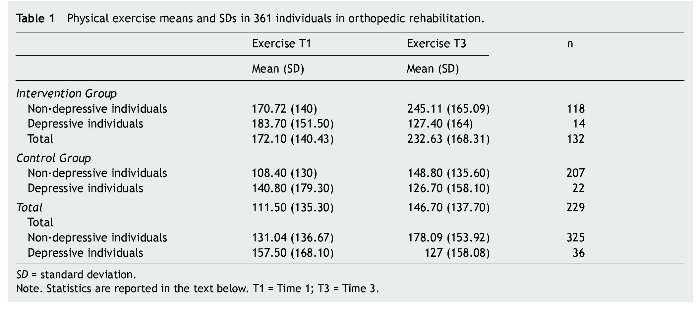
Out of the final sample, n = 325 (90%) scored negative and n = 36 (10%) scored positive on depressive symptoms. The control group comprised 207 individuals without depressive symptoms and 22 (10.60% of the control group) with depressive symptoms. In the intervention group, 118 were screened negative on depressive symptoms and 14 were screened positive (11.90% of the intervention group).
The self-regulation intervention
The online intervention consisted of two units that were delivered at the beginning and end of the rehabilitation stay. Within both units, individuals were prompted to generate up to five post-rehabilitation exercise ideas (e.g., swimming, running), as well as to form up to five post-rehabilitation action plans (e.g., Prestwich, Lawton, & Conner, 2003). Additionally, the second intervention addressed the volitional strategy of action control. A diary to self-monitor one's home-based physical exercise was handed out to participants (e.g., Sniehotta et al., 2005). On average, participants in the intervention group spent 36.10 minutes (SD = 10.10) on the questionnaire and the intervention at T1 and 20.30 minutes (SD = 19.50) with the program and the questionnaire at T2.
Measures
Depressive symptoms were measured at the end of rehabilitation (T2) by the 2-item version of the Patient Health Questionnaire (PHQ-2; Kroenke, Spitzer, & Williams, 2003). The PHQ-2 assesses the frequency of depressed mood and anhedonia over the past two weeks. The two items were "Have you often been bothered by feeling down, depressed, or hopeless?" and "Have you oft≤en been bothered by little interest or pleasure in doing things?". Responses ranged from "not at all" (0), "on some days" (1), "more than half of the days" (2), and "nearly every day" (3). Responses were aggregated, and, according to Kroenke et al. (2003), those who had a score of three and higher were categorized as patients with depressive symptoms. Löwe, Kroenke, and Gräfe (2005) found the PHQ-2 to have a sensitivity of 79% and a specificity of 86% for any depressive disorder.
Physical exercise considering the effort of exercise was measured at the beginning of the rehabilitation stay and six weeks after rehabilitation with a modified version of the Godin Leisure-Time Exercise Questionnaire (GLTEQ; Godin & Shephard, 1985; Plotnikoff et al., 2007). At T1 rehabilitation patients were asked how much exercise they had performed prior to rehabilitation. Six weeks after rehabilitation (T3), exercise in the last four weeks was assessed. Each time, participants indicated how often per week and how long per session they performed moderate and strenuous physical exercise. Total physical exercise was the number of sessions per week multiplied by minutes per session. The scale has been used in a rehabilitation setting before (Lippke, Ziegelmann, and Schwarzer, 2004a).
Analytic procedure
To test the effect of the intervention and depressive symptoms, as well as the interaction of intervention and depressive symptoms on physical exercise T3, an analysis of covariance (ANCOVA) with the covariates exercise T1, sex, and phase of assessment was conducted.
Results
Randomization check
Participants in the intervention group reported significantly higher levels of physical exercise prior to rehabilitation than participants in the control group (Mcontrol group = 111.50; M intervention group = 173.20; t(359) = -4.10; p ≤ .001). The groups did not differ with regard to age, gender, occupational status, high school degree, partner status, and depressive symptoms (p's > .05).
Attrition analysis
The original sample at T1 (N = 581) differed from the longitudinal sample at T3 (N = 361) with regard to age (M T1 sample = 48.30; Mlongitudinal sample = 45.90; t (399) = -2.80; p = .01). Thus, individuals who continued the participation in the study were younger than those who dropped out. No differences were found with regard to gender, occupational status, high school degree, and partner status (p's > .05) between the T1 and the T3 sample. Samples did not differ with regard to depressive symptoms at T2 or physical exercise prior to rehabilitation (p's > .05).
Preliminary results
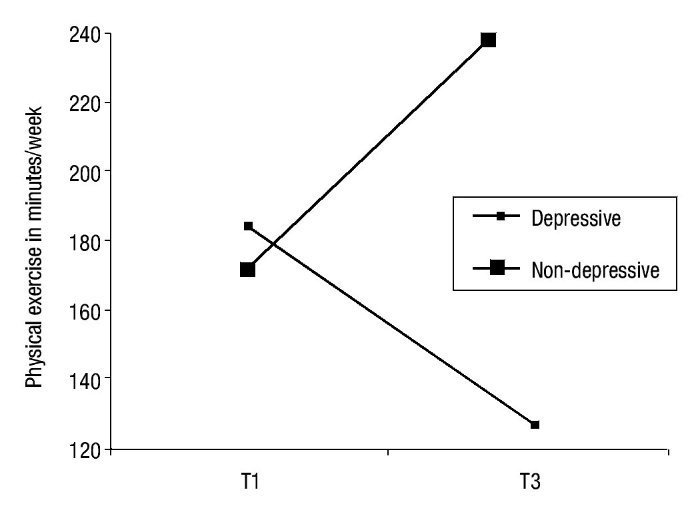
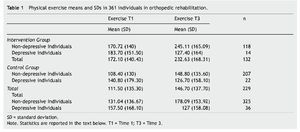
Means of exercise T1 and exercise T3 are depicted in Table 1. Overall, individuals without depressive symptoms increased their levels of exercise, in particular individuals in the intervention group. Individuals with depressive symptoms rather decreased their level of exercise within the control and intervention group.
Main effects and interaction effect
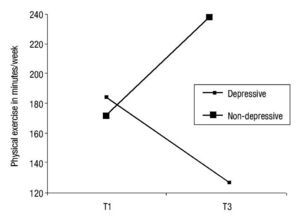
The ANCOVA (covariates: exercise prior to rehabilitation, sex, phase of assessment) revealed two significant main effect and a marginal significant interaction effect: Depressive symptoms (F (1, 354) = 8.10; p = .005; partial η2= .02) and the intervention condition (F (1, 354) = 6.50; p = .011; partial η2= .02) predicted exercise T3 significantly. However, results also revealed a marginal significant interaction of intervention x depressive symptoms (F (1, 354) = 3.20; p = .076; η2= .01). Figure 2 illustrates that individuals without depressive symptoms in the intervention group reported higher levels of exercise compared to individuals with depressive symptoms in the intervention group. Additionally to the main effects and the interaction effect, the covariates exercise prior to rehabilitation (F (1, 354) = 20.30; p ≤ .001; η2= .05) and phase of assessments (F(1, 354) = 5.30; p = .021; η2= .02) predicted exercise after rehabilitation.
Figure 2 Means of physical exercise T1 and T3 are depicted for individuals with and without depressive symptoms in the intervention group. Note. Individuals without depressive symptoms in the intervention group increased their levels of exercise 6 weeks after rehabilitation, whereas individuals with depressive symptoms did not.
Discussion
This study aimed to investigate whether a common computer-based self-regulation intervention during orthopedic rehabilitation is effective in promoting exercise after rehabilitation in individuals with or without depressive symptoms. We hypothesized that depressive symptoms moderate the effectiveness of the self-regulation intervention, i.e., that a common self-regulation intervention is more effective in increasing exercise in individuals without depressive symptoms than in individuals with depressive symptoms.
Depressive symptoms moderate the effectiveness of an exercise self-regulation intervention
The overall (in the intervention and control group) negative effect of depressive symptoms on exercise is in line with previous meta-analytic findings (Roshanaei-Moghaddam, Katon, & Russo, 2009). Our study adds to these findings by replicating this negative link with regard to post-rehabilitation exercise in a sample of orthopedic patients. As regular exercise training is essential for the physical rehabilitation of individuals with orthopedic health problems and depressive symptoms are highly prevalent in this target group, it is important to consider that depressive symptoms might interfere with the engagement in exercise after rehabilitation.
Findings of our study indicate that a self-regulation intervention is effective to enhanced post-rehabilitation exercise. Targeted self-regulatory strategies in the present intervention were to generate exercise ideas (i.e., exercise goals), make detailed action plans (when, where, and how will I exercise), and to monitor one's own behavior with the help of an exercise diary. The main effect of the treatment is in line with previous studies demonstrating the benefit of self-regulation interventions to increase exercise (Latimer et al. 2006; Lippke et al., 2004b; Sniehotta et al., 2005). However, individuals with depressive symptoms in the intervention group did not increase their exercise levels six weeks after rehabilitation. They exercised less than individuals without depressive symptoms in the intervention group. This is in line with the assumption that individuals with depressive symptoms might have fewer capabilities to implement health behavior due to depleted self-regulatory resources (Hagger et al., 2010; Tice & Bratslavsky, 2000). One might assume that individuals with depressive symptoms planned less, had difficulties setting realistic plans, or did not adhere to their plans. Individuals dealing with depressive symptoms might have also not self-monitored their exercise behavior with the help of a diary. Further, our intervention asked individuals to set up to five exercise ideas and make up to five exercise plans. The intervention might have been overwhelming for individuals with depressive symptoms. Less ambitious goals might avoid frustration and thus produce more positive feelings in individuals with depressive symptoms (Conn, 2010). Goal achievement was found to have a positive effect on depressive symptoms (Scholz, Knoll, Sniehotta, & Schwarzer, 2006). A decrease of depressive symptoms and the positive experiences of goal attainment might later enhance the likelihood to engage in exercise. Thus, interventions that prompt the generation of fewer goals or plans might be more appropriate for individuals with depressive symptoms. Further, one could presume that external strategies (e.g., social support, social control) are more beneficial for individuals with depressive symptoms to increase their exercise. Such strategies might require less self-regulatory effort and thus consider depleted resources. However, studies on these questions are missing. One might also question whether the mode of our intervention was suitable to support participants suffering from depressive symptoms. Although, there is some evidence for the effectiveness of computer-based intervention in the field of psychotherapy (Proudfoot, 2004), most computer-delivered treatments fail to address non-specific treatment factors (e.g., empathy). Such non-specific factors contribute to the effects of face-to-face psychotherapy to a valuable degree (Proudfoot, 2004). Exercise interventions for individuals with depressive symptoms might also benefit from such non-specific factors. Additionally, individuals with depressive symptoms may benefit from more regular contact. Our intervention was delivered only twice during rehabilitation. Interventions with frequent contacts were found to be more effective at fostering exercise maintenance in individuals than interventions with fewer contacts (Fjeldsoe, Neuhaus, Winkler, & Eakin, 2011). Particularly individuals suffering from depressive symptoms might benefit from weekly reminders and booster sessions (Hampel, Graef, Krohn-Grimberghe, & Tlach, 2009). Finally, individuals experiencing depressive symptoms might benefit from additional psychotherapeutic support, e.g., cognitive behavior therapy (Hollon, Stewart & Strunk, 2006). Integrated approaches that address the management of depressive symptoms and health behaviors, rather than an exercise intervention alone, might be advantageous for individuals with depressive symptoms. By considering depression management when promoting health behavior and vice versa, treatments might become synergistic (Detweiler-Bedell et al., 2008). However, research on integrated approaches for the promotion of exercise in individuals with comorbid depressive symptoms is required.
Outlook
Advantages of exercise are twofold in particular for individuals experiencing depressive symptoms: exercise fosters physical health and also alleviates depressive symptoms (Conn, 2010). Therefore, these individuals should not be neglected when designing exercise promotion programs for rehabilitation patients. Future research needs to focus on the development and evaluation of appropriate exercise programs for rehabilitation patients with depressive symptoms. One focus might be set on integrated approaches that address exercise behavior and depressive symptoms. Moreover, exercise programs could be more tailored to the particular situation of individuals experiencing depressive symptoms (e.g., by considering fewer self-regulatory resources in these individuals). Further, studies need to test whether some health behavior change strategies are superior to others in increasing exercise in individuals with depressive symptoms (self-regulatory strategies vs. more external strategies). Future research might also evaluate effects regarding different modes (computer vs. face-to-face) and intensities (frequency of contacts) of exercise programs for individuals with depressive symptoms. By addressing these questions, more appropriate interventions to support individuals suffering from depressive symptoms to engage in exercise may be developed.
Limitations
Some limitations need to be addressed. First, the interaction effect was only marginal significant. Replications of the findings in similar samples are required. Second, participation rates of individuals with depressive symptoms were low in our study compared to actual prevalence of depressive symptoms in orthopedic rehabilitation. The relatively low rate of participants with depressive symptoms in this study might have resulted from two aspects. A screening instrument rather than a clinical diagnosis was used to identify individuals with depressive symptoms. Moreover, the study participation was optional for medical rehabilitation patients and individuals with depressive symptoms might have been less likely to participate. An increase of the participation rate of individuals dealing with depressive symptoms in future studies is desirable. Third, the assessment of self-regulation energy (i.e., ego depletion) would be helpful to strengthen theoretical assumptions. Thus, future studies need to replicate the findings and include measures of ego-depletion.
Conclusion
The self-regulation intervention seemed effective in increasing post-rehabilitation exercise among individuals without depressive symptoms, but not among participants with depressive symptoms. Thus, a self-regulation exercise intervention which is not tailored to the needs of individuals suffering from depressive symptoms might not be effective in increasing post-rehabilitation exercise in this target group.
If we want to support individuals with depressive symptoms to engage in regular exercise, research is required to clarify how exercise programs for individuals with depressive symptoms can be designed effectively. Future research might compare the effectiveness of different health behavior change techniques that are most beneficial for individuals with depressive symptoms. Moreover, integrated approaches that address the management of health behavior and depressive symptoms in concert, i.e., by integrating exercise programs and cognitive behavior therapy, might be considered in the future.
*Corresponding author at:
Health Psychology, Freie University Berlin, Habelschwerdter Allee 45 (PF 10), 14195 Berlin, Germany. E-mail address: sarah.pomp@fu-berlin.de (S. Pomp).
Received May 2, 2012;
accepted October 30, 2012
References
Bardwell, W. A., & Fiorentino, L. (2012). Risk factors for depression in breast cancer survivors: An update. International Journal of Clinical and Health Psychology, 12, 311-331.
Baumeister, R. F., Muraven, M., & Tice, D. M. (2000). Ego depletion: A resource model of volition, self-regulation, and controlled processing. Psychological Bulletin, 18, 130-150.
Burgos-Garrido, E., Gurpegui, M., & Jurado, D. (2011). Personality traits and adherence to physical activity in patients attending a primary health centre. International Journal of Clinical and Health Psychology, 11, 539-547.
Carver, C. S., & Scheier, M. F. (1998). On the self-regulation of behavior. New York: Cambridge University Press.
Conn, V. S. (2010). Depressive symptom outcome of physical activity interventions: Meta-analysis findings. Annals of Behavioral Medicine, 39, 128-138.
Conner, M., Sandberg, T., & Norman, P. (2010). Using action planning to promote exercise behavior. Annals of Behavioral Medicine, 40, 65-76.
Detweiler-Bedell, J. B., Friedman, M. A., Leventhal, H., Miller, I. W., & Leventhal, E. A. (2008). Integrating co-morbid depression and chronic physical disease management: identifying and resolving failures in self-regulation. Clinical Psychological Review, 28, 1426-1446.
Fjeldsoe, B., Neuhaus, M., Winkler, E., & Eakin, E. (2011). Systematic review of maintenance of behavior change following physical activity and dietary interventions. Health Psychology, 30, 99-109.
Godin, G., & Shephard, R.J. (1985). A simple method to assess exercise behavior in the community. Canadian Journal of Applied Sport Science, 10, 141-146.
Hagger, M. S., Wood, C., Stiff, C., & Chatzisarantis, N. L. (2010). Ego depletion and the strength model of self-control: A meta-analysis. Psychological Bulletin, 136, 495-525.
Hampel, P., Graef, T., Krohn-Grimberghe, B., & Tlach, L. (2009). Effects of gender and cognitive-behavioral management of depressive symptoms on rehabilitation outcome among inpatient orthopedic patients with chronic low back pain: A 1 year longitudinal study. European Spine Journal, 18, 1867-1880.
Hollon, S. T., Stewart, M. O., & Strunk, D. (2006). Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annual Review of Psychology, 57, 285-315.
Huisman, S., De Gucht, V., Maes, S., Schroevers, M., Chatrou, M., & Haak, H. (2009). Self-regulation and weight reduction in patients with type 2 diabetes: A pilot intervention study. Patient Education Counseling, 75, 84-90.
Knittle, K., Maes, S., & De Gucht, V. (2010). Psychological interventions for rheumatoid arthritis: Examining the role of self-regulation with a systematic review and meta-analysis of randomized controlled trials. Arthritis Care and Research, 62, 1460-1472.
Kroenke, K., Spitzer, R. L., & Williams, J.B. (2003). The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care, 41, 1284-1294.
Latimer, A. E., Ginis, K. A., & Arbour, K. P. (2006). The efficacy of an implementation intention intervention for promoting physical activity among individuals with spinal cord injury: A randomized controlled trial. Rehabilitation Psychology, 51, 273-280.
Lippke, S., Ziegelmann, J. P., & Schwarzer, R. (2004a). Behavioral intentions and action plans promote physical exercise: A longitudinal study with orthopedic rehabilitation patients. Journal of Sport and Exercise Psychology, 26, 470-483.
Lippke, S., Ziegelmann, J. P., & Schwarzer, R. (2004b). Initiation and maintenance of physical exercise: Stage-specific effects of a planning intervention. Research in Sports Medicine, 12, 221-240.
Löwe, B., Kroenke, K., & Gräfe, K. (2005). Detecting and monitoring depression with a 2-item questionnaire (PHQ 2). Journal of Psychosomatic Research, 58, 163-171.
Michie, S., Ashford, S., Sniehotta, F. F., Dombrowski, S. U., Bishop, A., & French, D. P. (2011). A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: The CALO-RE taxonomy. Psychology and Health, 26, 1479-1498.
Nickision, R. S., Boards, T. N., & Kay, P. R. (2009). Post-operative anxiety and depression level in orthopoedic surgery: A study of 56 patients undergoing hip or knee arthoplastry, Journal of Evaluation in Clinical Practice, 15, 307-310.
Plotnikoff, R. C., Lippke, S., Reinbold-Matthews, M., Courneya, K. S., Karunamuni, N., Sigal, R. J., & Birkett, N. (2007). Assessing the validity of a stage measure on physical activity in a population-based sample of individuals with type 1 or type 2 diabetes. Measurement in Physical Education and Exercise Science, 11, 73-91.
Pomp, S., Lippke, S., Fleig, L., & Schwarzer, R. (2010). Synergistic effects of intention and depression on action control: Longitudinal predictors of exercise after rehabilitation. Mental Health and Physical Activity, 2, 78-84.
Prestwich, A., Lawton, R., & Conner, M. (2003). The use of implementation intentions and decisional balance sheet in promoting exercise behavior. Psychology and Health, 18, 707-721.
Proudfoot, J. G. (2004). Computer-based treatment for anxiety and depression: Is it feasible? Is it effective? Neuroscience and Biobehavioral Reviews, 28, 353-363.
Reuter, T., Ziegelmann, J. P., Lippke, S., & Schwarzer, R. (2009). Long-term relations between intentions, planning, and exercise: A 3-year longitudinal study after orthopedic rehabilitation. Rehabilitation Psychology, 54, 363-371.
Riddle, D. L., Wade, J. B., & Jiranek, W. A. (2010). Major depression, generalized anxiety disorder, and panic disorder in patients scheduled for knee arthroplasty. The Journal of Arthroplasty, 25, 581-588.
Roshanaei-Moghaddam, B., Katon, W. J., & Russo, J. (2009). The longitudinal effects of depression on physical activity. General Hospital Psychiatry, 31, 306-315.
Scholz, U., Knoll, N., Sniehotta, F. F., & Schwarzer, R. (2006). Physical activity and depressive symptoms in cardiac rehabilitation: Long-term effects of a self-management intervention. Social Science and Medicine, 62, 3109-3120.
Sniehotta, F. F., Gorski, C., & Araujo-Soares, V. (2010). Adoption of community-based cardiac rehabilitation programs and physical activity following phase III cardiac rehabilitation in Scotland: A prospective and predictive study. Psychology and Health, 25, 839-854.
Sniehotta, F. F., Scholz, U., & Schwarzer, R. (2005). Bridging the intention-behavior gap: Planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychology and Health, 20, 143-160.
Sniehotta, F. F., Scholz, U., Schwarzer, R., Fuhrmann, B., Kiwus, U., & Völler, H. (2005). Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. International Journal of Behavioral Medicine, 12, 244-255.
Tice, D. M., & Bratslavsky E. (2000). Giving in to feel good: The place of emotion regulation in the context of general self-control. Psychological Inquiry, 11, 149-159.
Watson, D., Clark, A. C., & Stasik, S. M. (2011). Emotions and the emotional disorders: A quantitative hierarchical perspective. International Journal of Clinical and Health Psychology, 11, 429-442.
Ziegelmann, J. P., Luszczynska, A., Lippke, S., & Schwarzer, R. (2007). Are goal intentions or implementation intentions better predictors of health behavior? A longitudinal study in orthopedic rehabilitation. Rehabilitation Psychology, 52, 97-102.