There is a recognized increase of lifelong surgery risk in Crohn disease (CD). Outcome data concerning surgery in children, particularly in the biological era, are limited.
AimTo characterize the clinical profile and the clinical outcome in children and adolescents with CD who underwent surgical intervention, in a single tertiary referral center.
MethodsRetrospective, cross-sectional study, including pediatric patients with CD undergoing intra-abdominal surgery in the last 11 years.
ResultsIncluded eight of 50 CD total patients (16%); six female; median age at CD diagnosis of 12.0 years; Paris classification: (a) location: ileocolonic (5), colonic (1), upper disease (1), ileocolonic/upper disease (1); (b) behavior: stricturing (4), nonstricturing nonpenetrating (2), penetrating (1), both penetrating and stricturing disease (1); growth delay (2). Six children received thiopurines, five mesalazine, three corticosteroids and four anti-TNF therapy, preoperatively. Surgery followed diagnosis by a median of 2.9 years. Median PCDAI at the time of surgery was 35.0. Elective surgery was performed in six patients and emergency surgery in two, without major complications. Five children received anti-TNF and three thiopurines post-operatively. Within the follow-up period (median 1.7 years), relapse occurred in one child (3.2 years after intervention); the remaining seven patients persist in clinical remission. Median PCDAI in the last evaluation was 6.3. Weight and height recovery was observed in seven patients, at last follow-up.
ConclusionSurgical treatment of CD is a valid alternative in selected cases, contributing to the resolution of acute complications and maintenance of remission, allowing disease-free interval and nutritional recovery.
É reconhecido o risco aumentado de cirurgia ao longo da vida na população com doença de Crohn (DC). Contudo os estudos publicados em idade pediátrica são ainda escassos, particularmente na era dos biológicos.
ObjetivosCaraterizar o perfil evolutivo da população pediátrica com DC submetida a cirurgia num centro de referência.
MétodosEstudo retrospetivo, transversal, doentes pediátricos com DC submetidos a cirurgia intra-abdominal no período de 11 anos.
Resultados8/50 doentes com DC (16%); seis raparigas; idade mediana ao diagnóstico 12,0 anos; Classificação de Paris: a) localização: ileocólica (5), cólica (1), proximal (1); ileocólica e proximal (1); b) comportamento: estenosante (4), não estenosante não penetrante (2), penetrante (1), estenosante e penetrante (1); atraso de crescimento (2); terapêutica pré-cirurgia: tiopurinas (6), mesalazina (5), corticóides (3) e agentes biológicos (4). Mediana do PCDAI à data da cirurgia 35,0. O timing cirúrgico mediano foi 2,9 anos após o diagnóstico. Foram efetuadas cirurgias eletivas em seis doentes e de emergência em dois, sem complicações. No período após cirurgia, a terapêutica de manutenção incluiu: biológicos (5) e tiopurinas (3). No período de seguimento (mediana 1,7 anos), ocorreu recidiva numa criança (3,2 anos após a intervenção); as restantes persistiram em remissão clínica; PCDAI mediano na última avaliação 6,3. Observou-se recuperação ponderal e estatural em sete doentes, na última avaliação.
ConclusãoO tratamento cirúrgico da DC representa uma alternativa válida em casos selecionados, contribuindo para a resolução de complicações agudas e manutenção da remissão, permitindo um intervalo livre de doença e recuperação nutricional.
Crohn disease (CD) at pediatric age is recognizably associated with significant morbidity, with growth and nutritional impairment. New epidemiological data indicate that the incidence of CD in this specific age group is continually rising, with up to 25% of patients with inflammatory bowel disease being diagnosed before age 20.1–3 In Portugal, a recent pharmaco-epidemiological study, based on regional intestinal anti-inflammatory drugs consumption, estimated an incidence of CD pediatric patients of 6.7/100,000 children/year.4
This chronic relapsing disease may have devastating effects on patient's quality of life with need for long-term therapy, frequent hospitalizations and consultations.5
The medical therapy of CD has dramatically changed over the past decade, with the increasing use of early anti-TNF, both in children and adulthood. However, it remains to be elucidated the true impact of this therapy in disease natural course and the need of surgery.
It has been estimated that the total life time risk of surgery in CD adult patients is between 50% and 70%.6 Gupta et al reported that the cumulative incidence of surgery in a pediatric population was 17% at 5 years and 28% at 10 years after diagnosis. In this study, the main risk factors for the first surgery were the presence of abscess, fistula or stricture and poor growth at presentation.7 Furthermore, Nod2/CARD15 gene variants which play an important role in the susceptibility to CD, may also be associated with the development of intestinal strictures and increased risk for surgery.8
The results of surgery in children with CD are largely dated from the 1980s and early 1990s, a period in which immunomodulators were not widely used and biological therapy had not yet begun.
Elective surgery is generally advocated in children with growth failure not responding to medical therapy and/or stricturing disease. Despite the relative frequency of surgery in children with CD, there is a paucity of publications reporting outcomes and describing the results of minimal access techniques.9–11 Recent pediatric studies have reported a wide range of postoperative recurrence rate, between 18% and 94%, possibly reflecting different clinical settings, treatment protocols and surveillance after surgery.10,12–14
The aim of the present study was to characterize the clinical profile and the clinical outcome of children and adolescents with CD, who underwent surgical intervention within the last 11 years period in a tertiary referral center.
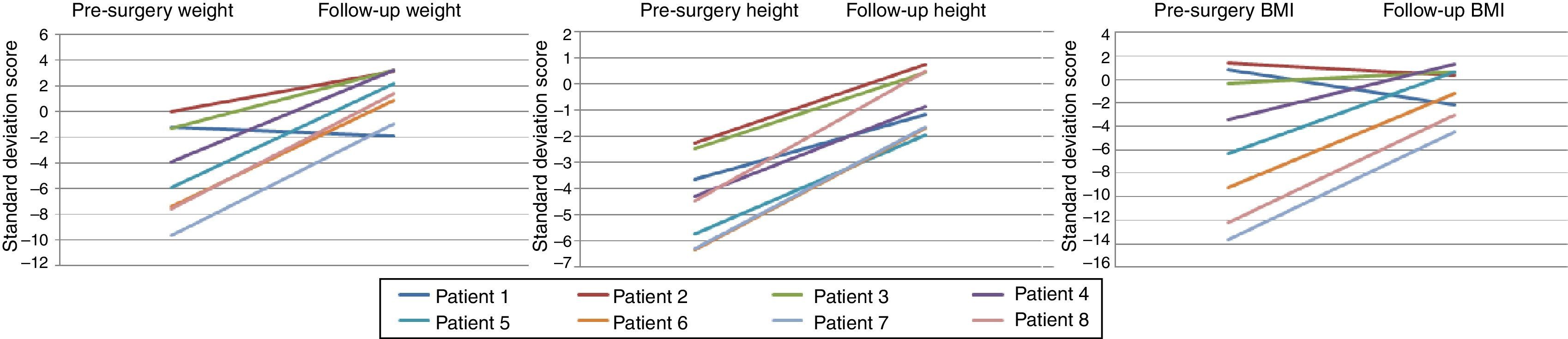
2Materials and methodsThis was a retrospective, cross-sectional study, including pediatric patients less than 18 years with the diagnosis of CD established according to Porto Criteria,15 undergoing intra-abdominal surgery in our unit between January 2004 and December 2014. All patients were identified from a department database and clinical data were collected from patient records. A standardized protocol has been used before and after surgery. Date of diagnosis was taken as the date of the first endoscopy with histological confirmation of the disease. Height, weight and body mass index (BMI) were converted to SD scores (SDS) using the National Center for Health Statistics international growth reference. Growth data before surgery and at last follow-up were compared using a T test, with significance considered at p<0.05. Paris phenotypic classification immediately before surgery, pre and postoperative medical therapy and type of surgery were recorded. Clinical response was assessed by Pediatric Crohn's Disease Activity Index (PCDAI) at baseline and at last follow-up and classified into 3 categories: clinical remission (PCDAI <10), relapse (disease-free time with subsequent rise in PCDAI >10) and persistence of active disease (unabated PCDAI >12.5). All patients undergoing elective intra-abdominal surgery underwent preoperative MRI scans. Endoscopic evaluation and MRI scans were done approximately one year after surgery. The surgical techniques used were selected according to surgical team experience. Two emergency surgeries were performed in district hospitals, by general surgery teams. Major surgery-related complications were defined as potentially life-threatening, with the need of re-intervention or hospital stay longer than twice the median hospitalization for the same procedure.
3Results3.1Preoperative evaluationThe database included 50 patients diagnosed with CD during the study period; eight patients underwent surgery (16%). Table 1 summarizes the results. Median age at CD diagnosis was 12.0 years (mean 12.4±2.8 years; range 7.9–17.1 years). Paris classification: CD diagnosis was established below 10 years in one patient, between 10 and 16 years in six patients and at 17 years in one patient. Concerning the location of the disease: ileocolonic (5), colonic (1), upper disease (1), ileocolonic/upper disease (1). Regarding the disease behavior, classification was as follows: stricturing (4), nonstricturing nonpenetrating (2), penetrating (1), both penetrating and stricturing disease (1). Six patients had no evidence of growth delay. Three patients had pubertal delay at the time of surgery. Median CD index activity (PCDAI) was 35.0 (mean 35±13.2; range 15–55) indicating a moderate activity disease. All patients started partial/exclusive enteral nutrition at CD diagnosis. Mesalazine was used in five patients preoperatively, thiopurines in six and steroids in three patients. Monoclonal anti-TNF therapy (infliximab or adalimumab) was used in four patients.
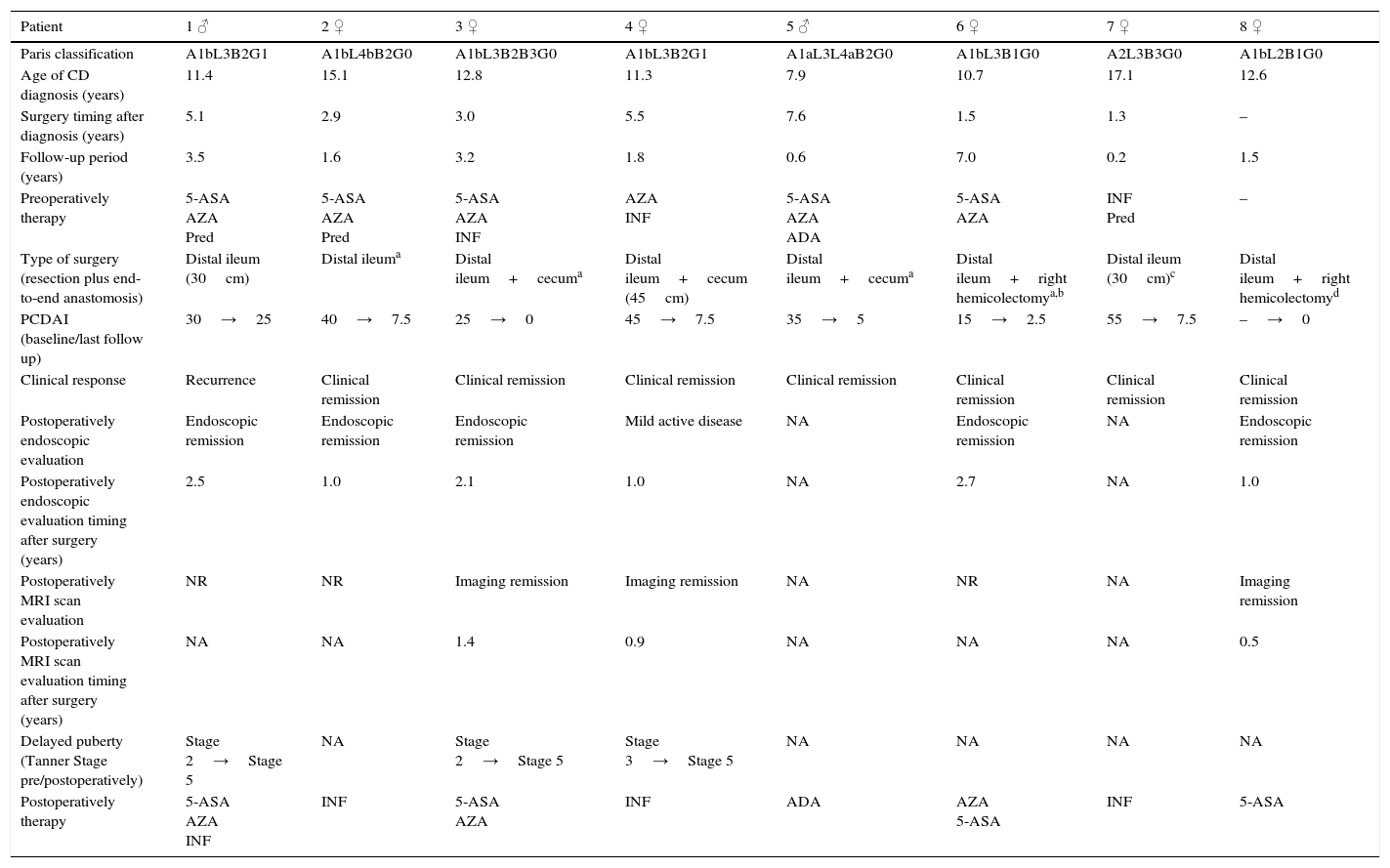
Table summarizing the results.
| Patient | 1 ♂ | 2 ♀ | 3 ♀ | 4 ♀ | 5 ♂ | 6 ♀ | 7 ♀ | 8 ♀ |
|---|---|---|---|---|---|---|---|---|
| Paris classification | A1bL3B2G1 | A1bL4bB2G0 | A1bL3B2B3G0 | A1bL3B2G1 | A1aL3L4aB2G0 | A1bL3B1G0 | A2L3B3G0 | A1bL2B1G0 |
| Age of CD diagnosis (years) | 11.4 | 15.1 | 12.8 | 11.3 | 7.9 | 10.7 | 17.1 | 12.6 |
| Surgery timing after diagnosis (years) | 5.1 | 2.9 | 3.0 | 5.5 | 7.6 | 1.5 | 1.3 | – |
| Follow-up period (years) | 3.5 | 1.6 | 3.2 | 1.8 | 0.6 | 7.0 | 0.2 | 1.5 |
| Preoperatively therapy | 5-ASA AZA Pred | 5-ASA AZA Pred | 5-ASA AZA INF | AZA INF | 5-ASA AZA ADA | 5-ASA AZA | INF Pred | – |
| Type of surgery (resection plus end-to-end anastomosis) | Distal ileum (30cm) | Distal ileuma | Distal ileum+cecuma | Distal ileum+cecum (45cm) | Distal ileum+cecuma | Distal ileum+right hemicolectomya,b | Distal ileum (30cm)c | Distal ileum+right hemicolectomyd |
| PCDAI (baseline/last follow up) | 30→25 | 40→7.5 | 25→0 | 45→7.5 | 35→5 | 15→2.5 | 55→7.5 | –→0 |
| Clinical response | Recurrence | Clinical remission | Clinical remission | Clinical remission | Clinical remission | Clinical remission | Clinical remission | Clinical remission |
| Postoperatively endoscopic evaluation | Endoscopic remission | Endoscopic remission | Endoscopic remission | Mild active disease | NA | Endoscopic remission | NA | Endoscopic remission |
| Postoperatively endoscopic evaluation timing after surgery (years) | 2.5 | 1.0 | 2.1 | 1.0 | NA | 2.7 | NA | 1.0 |
| Postoperatively MRI scan evaluation | NR | NR | Imaging remission | Imaging remission | NA | NR | NA | Imaging remission |
| Postoperatively MRI scan evaluation timing after surgery (years) | NA | NA | 1.4 | 0.9 | NA | NA | NA | 0.5 |
| Delayed puberty (Tanner Stage pre/postoperatively) | Stage 2→Stage 5 | NA | Stage 2→Stage 5 | Stage 3→Stage 5 | NA | NA | NA | NA |
| Postoperatively therapy | 5-ASA AZA INF | INF | 5-ASA AZA | INF | ADA | AZA 5-ASA | INF | 5-ASA |
ADA: adalimumab; Aza: azathioprine; BMI: body mass index; INF: infliximab; NA: not applicable; NR: no realized; Pred: prednisolone; 5-ASA: mesalazine.
Median surgical timing was 2.9 years after CD diagnosis (mean 3.4±2.5 years; range 1.3–7.6 years). Six children had elective surgery based on clinical, endoscopic, imagiological findings and unresponsiveness to medical therapy. The most common indication for elective surgery was stricturing or penetrating disease (n=6); one child had additionally intestinal suboclusion. Two patients developed an acute abdomen and required emergency surgery for life-threatening conditions. Emergency surgery was due to: ileocecal abscess with ileal perforation and peritonitis (n=1) and acute appendicitis/peritonitis (n=1). In this last patient, the diagnosis of CD was made on the day of surgery. Surgical procedures performed are summarized in Table 1 and included: partial ileal resection (n=3), ileocecal resection (n=3), ileal plus right hemicolectomy (n=2). The extension of resected ileum ranged between 30 and 45cm in the 3/8 patients with available data. All surgeries took place without major complications. No laparoscopic/stricturoplasty procedures were performed in this series.
3.3Postoperative courseMedian follow-up time was 1.7 years (mean 2.4±2.2 years; range 0.2 months to 7.0 years). Five children received anti-TNF therapy and three children received thiopurines as maintenance therapy postoperatively (one patient was treated simultaneously with anti-TNF plus thiopurine). During the follow-up period, all patients performed postoperatively endoscopic evaluation at a median period of 1.5 years (mean 1.7 years±0.8 years; range 1.0 months to 2.7 years), except the two patients in which follow-up period was less than 6 months; five patients presented endoscopic remission and the remained patient presented mild endoscopic activity. Postoperatively MRI was performed in three patients, within a median period of one year, and no disease activity was observed.
One patient (Patient 1) had clinical and endoscopic relapse, 3.2 years following surgery. In this patient, evidence of disease at the resection margin had not been observed.
Median PCDAI at the last evaluation was 6.3 (mean 6.9±8.0; range 0–25). Height and weight SDS significantly increased between surgery and the latest follow-up (p<0.05), although no significant increase in BMI SDS has been observed (p=0.07) (Fig. 1). The three children who had prepubertal stages evolved in their puberty status after surgery.
4DiscussionThe present study reflects the experience of a single tertiary center over a 10-year period, representing a national case series concerning specifically surgery in pediatric CD patients.
The natural history of pediatric CD often includes bowel surgery even in the biological therapy era. However, there is a wide range of surgery rate in the literature, depending on the studied population. Two recent pediatric studies from tertiary referral centers, reported a median interval from diagnosis to first surgery of 9 months and 1.9 years, respectively.9,11 In our series the whole surgery rate of 16% was relatively low, as compared to other pediatric series. In fact, intra-abdominal surgery in our cohort might have been performed relatively late in the course of disease, with a median interval from diagnosis to intervention of 2.9 years, which may reflect the recent impact of biological therapy use. However, the age of presentation (12.0 years) and disease location at diagnosis were both similar to other reported series.16,17
Preoperative therapy most commonly involved thiopurines and mesalazine. Monoclonal anti-TNF therapy before surgery was used in half of the patients. When looking at our cohort of patients, therefore, the question of whether surgery might have been delayed or prevented by increased use of biologic agents should also be raised. Considering that around 25% of pediatric patients with CD will present with stricturing disease,18 it is likely that a subset of our patients will develop fibrotic strictures which are unlikely to resolve with medical treatment. In fact, despites the use of more intensive medical therapy (including biological agents) this may only delay, rather than avoid surgery.19
However, most available studies do not report the impact of biological agents in the surgery timing and clinical outcome.9,13 Although in our series, four in eight patients were under biologic therapy, surgery was ultimately required, reflecting the unavoidable progressive disease behavior. Biologic therapy was not used in remaining four patients, concerning the earlier study period, where biologic agents were not yet available. In fact, this feature is common to the rare pediatric surgery series, mostly including a low rate of biological therapy use (7–10%).9,13
An additional issue concerning the use of biological agents in young patients with CD is the development of antibodies, and subsequent treatment resistance or dependence.20 An argument exists, therefore, that one advantage of surgical therapy is the maintenance of treatment naivety, retaining a useful therapeutic option in the future.
Limitations of the present series are the unavailability of data concerning the extension of ileal resection in five of eight patients and the fact that no laparoscopic stricturoplasty was performed. Although this minimally invasive surgery/stricturoplasty has not been performed, it is currently considered as the standard technical option when feasible, particularly in limited ileal disease.
Surprisingly, the two patients submitted to emergency surgery had a disease previously evaluated as nonpenetrating nonstricturing.
Although no major complications have occurred in our series, the small number of patients should be taken into account. In a large study from a regional center including 69 patients, a 29% complication rate was reported.9
According to ECCO/ESPGHAN guidelines21 endoscopic investigation should be done six months to one year after surgery to evaluate the effectiveness of the surgery and redefine therapeutic strategy. In this small cohort the postoperative endoscopic evaluation was performed a little later than the recommended period, and only three patients underwent MRI scan reflecting organizational limitations. The clinical relapse rate of 12.5% (one in eight patients) at a median follow-up of 1.7 years in our series is also consistent with that reported in the literature,13 concerning short/medium follow-up, although it is scarcely documented in surgical series. Expectedly, the recurrence rate increases with duration of follow-up, attaining rates as high as 94% at 10 years follow-up.10 Both clinical behavior (predominantly ileal restricted disease) and relatively low activity index in some patients might have contributed to the low recurrence rate in this series. Davies et al. reported that outcome after surgery for CD in children is mainly related to disease location, but is also influenced by the type of primary operation performed. In this study, concerning pre-biological agents era, anatomical location of disease, indication for surgery, and preoperative duration of symptomatic disease, were the only factors that significantly influenced the duration of the recurrence-free interval.22
The timing of surgery is crucial, because surgery can offer a disease-free interval to ensure normal growth and development when performed before late puberty.11,23 Growth delay leading to delayed puberty is recognized as a common complication of CD in the pediatric population. Our data are consistent with these observations, showing an improvement of weight and catch-up-growth. However, in a recent study involving a large number of patients no increase in height was observed.9 Interestingly, epidemiological data suggests a growth advantage of early surgery, with a recently published cohort of patients demonstrating better catch-up-growth in patients operated within 3 years of diagnosis.11 Thus this issue deserves further elucidation.
5ConclusionDespite the small size of the present cohort (single center study) and the relatively short follow-up period, data from the present study are consistent with the evidence that surgical treatment of CD is a valid alternative in selected cases, contributing to the resolution of acute complications and to the maintenance of clinical remission, allowing a disease-free interval and nutritional recovery. It should emphasized that surgical decisions should be taken by a multidisciplinary team, at an early stage of disease and ideally involving surgical teams from reference centers, with experience in minimally invasive/laparoscopic surgery techniques.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
To the Pathology Department and to the Pediatric and Adult Surgical Teams involved in the patients surgery.