Nosocomial spontaneous bacterial peritonitis (SBP) accounts for one third of all SBP episodes and is caused by microorganisms resistant to third generation cephalosporins (3rdGC) up to 40% of cases, mainly due to extended-spectrum β-lactamases (ESBL) Escherichia coli and Klebsiella pneumoniae producing strains, other Enterobacteriaceae spp. and some gram positive bacteria.1 In this setting, 3rdGC must not be used as empirical antibiotic therapy in nosocomial SBP. Carbapenems have been recommended based in bacteriological data reported in these cases.2,3 Ertapenem, a parenteral broad-spectrum 1-beta-methyl carbapenem was approved by FDA in US and in Europe for complicated intra-abdominal infections. We are treating nosocomial SBP with ertapenem provided that 93% of isolated bacteria in nosocomial SBP of our center were sensible in vitro to this carbapenem. We report three cases of nosocomial SBP caused by ertapenem-susceptible, ESBL-producing E. coli and K. pneumoniae with a microbiological and clinical failure to recommended standard doses of 1g/24h.
Case 1A 62-year-old male cirrhotic patient was admitted because of refractory ascites and hepato-renal syndrome (HRS). He presented with anasarca and a MELD score of 24. After HRS recovery, he developed hepatic encephalopathy and fever with a creatinine of 66μmol/L, albumin of 22g/L and bilirubin of 121μkat/L. He was receiving prophylaxis with norfloxacin. Ertapenem 1g every 24h was initiated. An ESBL-producing K. pneumoniae was isolated in ascitic fluid culture with a MIC<0.5mg/L for ertapenem, however after 48h ascitic fluid (AF) PMN count was higher and culture was still positive. After changing therapy to meropenem 500mg/8h, the AF culture become negative and PMN count normalized.
Case 2A 41-year-old female patient was admitted for fever and ascites 9 months after orthotopic liver transplantation. Creatinine was 110μmol/L, albumin 36g/L and bilirubin 12μkat/L. She was immunosuppressed with tacrolimus. Ertapenem 1g/24h was begun. AF culture yielded an ESBL-producing K. pneumonia with a MIC <0.5mg/L. During the following days, PMN count decreased but ascitic fluid culture remained positive. After 6 days, although the patient improved clinically, we changed antibiotic therapy to imipenem 500mg/6h and AF culture became negative after 24h of therapy.
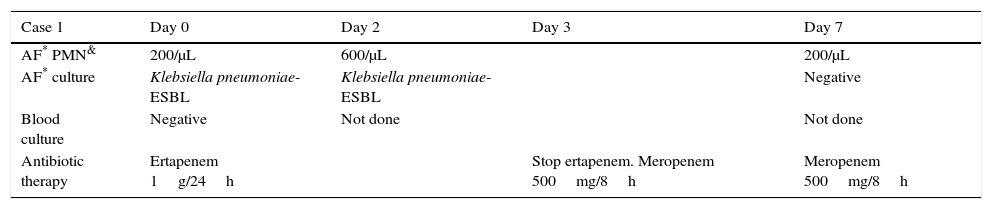
Case 3A 65-year-old male was admitted due to acute variceal bleeding. Patient was treated following our standard protocol. He developed a hepato-renal syndrome and was treated with terlypressin and albumin. Creatinine was 152μmol/L, albumin 29g/L and bilirubin 121μkat/L. AF analysis was diagnostic of SBP and ascitic and blood culture grew ESBL-E. coli with a MIC<0.5mg/L for ertapenem. In the following days, patient improved and the PMN count in ascitic fluid decreased; however AF culture remained positive until day 6 of therapy. We stopped antibiotic therapy at day 13 with normal PMN count and ascitic fluid culture finally negative. A summary of all AF analysis and cultures are shown in Table 1.
Asctic fluid, blood culture and polymorphonuclear count and antibiotic therapy in the three cases.
| Case 1 | Day 0 | Day 2 | Day 3 | Day 7 |
|---|---|---|---|---|
| AF* PMN& | 200/μL | 600/μL | 200/μL | |
| AF* culture | Klebsiella pneumoniae-ESBL | Klebsiella pneumoniae-ESBL | Negative | |
| Blood culture | Negative | Not done | Not done | |
| Antibiotic therapy | Ertapenem 1g/24h | Stop ertapenem. Meropenem 500mg/8h | Meropenem 500mg/8h |
| Case 2 | Day 0 | Day 2 | Day 6 | Day 7 |
|---|---|---|---|---|
| AF* PMN& | 5478/μL | 1496/μL | 525/μL | 200/μL |
| AF culture | Klebsiella pneumoniae-ESBL | Klebsiella pneumoniae-ESBL | Klebsiella pneumoniae-ESBL | Negative |
| Blood culture | Negative | Not done | Not done | Not done |
| Antibiotic therapy | Ertapenem 1g/24h | Stop ertapenem. Imipenem 500mg/6h | Imipenem 500mg/6h |
| Case 3 | Day 0 | Day 2 | Day 4 | Day 6 | Day 9 | Day 13 |
|---|---|---|---|---|---|---|
| AF* PMN& | 7221/μL | 4590/μL | 2960/μL | 560/μL | 330/μL | <100/μL |
| AF* culture | Escherichia coli-ESBL | Escherichia coli-ESBL | Escherichia coli-ESBL | Escherichia coli-ESBL | Negative | Negative |
| Blood culture | Escherichia coli-ESBL | Not done | Not done | Not done | Not done | Not done |
| Antibiotic therapy | Ertapenem 1g/24h | Stop ertapenem |
Carbapenems are considered the drugs of choice for serious infections due to ESBL-producing bacteria.4 Ertapenem is a good option when coverage against Pseudomonas aeruginosa or Acinetobacter baumannii is not needed,5 and it is recommended for the treatment of complicated intra-abdominal infections.6 It is noteworthy that despite a good sensibility in vitro measured by a MIC of <0.5mg/L, treatment failed to resolve infection in patient 1 and 2 and delayed SBP resolution in case 3. Verdier et al.7 studied ertapenem concentration in plasma and peritoneal fluid from patients with severe intra-abdominal infections. The study showed that ertapenem at 1 gr/day achieved highly variable plasma and peritoneal antibiotic concentrations. Ertapenem had a good peritoneal diffusion, but concentrations were frequently below the susceptibility breakpoint for ESLB-Enterobacteriaceae. Data in cirrhotic patients with ascites are not available. Host factors as hypoalbuminaemia may have a profound effect on ertapenem pharmacokinetics producing a decreased concentration in plasma and tissues.8 This may be relevant in cirrhotic patients. As others β-lactams, time above MIC is a key point to achieve good clinical and microbiological results and prevent resistance.
Resistance to ertapenem in ESBL-producing isolates during therapy may occur due to concurrent loss of porins and has been described in both K. penumoniae9 and E. coli.10 Nevertheless, in our three cases, MIC for ertapenem did not change during therapy in AF isolated bacteria.
Appropriate antibiotic empirical therapy in nosocomial SBP is unknown. Other carbapenem, imipenem and meropenem, and piperacillin–tazobactam alone or associated with glycopeptides have been suggested although randomized clinical trials are scanty.11 Knowing prevalence and susceptibility of bacteria involved in nosocomial SBP in each center is mandatory to choose the best option. Pharmacokinetic studies of new therapies are needed. In critically-ill cirrhotic patients, ertapenem at 1g/day may be insufficient due to hypoalbuminaemia and a low AF antibiotic concentration and 1 gr twice day may be more suitable for nosocomial SBP treatment.