Spontaneous cholecystocutaneous fistula (CCF) is defined as the communication of the gallbladder with the skin, without trauma or previous biliary surgery, and is a potential complication of gallstones.1–10 The current incidence is extremely low, and CCF associated with a cholecystocholedochal fistula (Mirizzi syndrome, type II) is even rarer. We present a case of CCF and cholecystocholedochal fistula and review the literature on this subject.
The patient was a 66-year-old woman with a history of morbid obesity, high blood pressure, hyperuricaemia, obstructive sleep apnoea syndrome, chronic obstructive pulmonary disease, partial thrombosis of the coeliac trunk and atrial fibrillation who came to the emergency department for abdominal pain that had commenced 24h previously, located in the umbilical region. A strangulated umbilical hernia was observed on examination. As an incidental finding, a punctate orifice was observed on the right flank that discharged a clear yellow, oily liquid, which the patient reported as having been present for 10 years (Fig. 1). Urgent surgery was performed with a periumbilical incision, resecting 15cm of ileum but not acting on the previously described fistula at the patient's request.
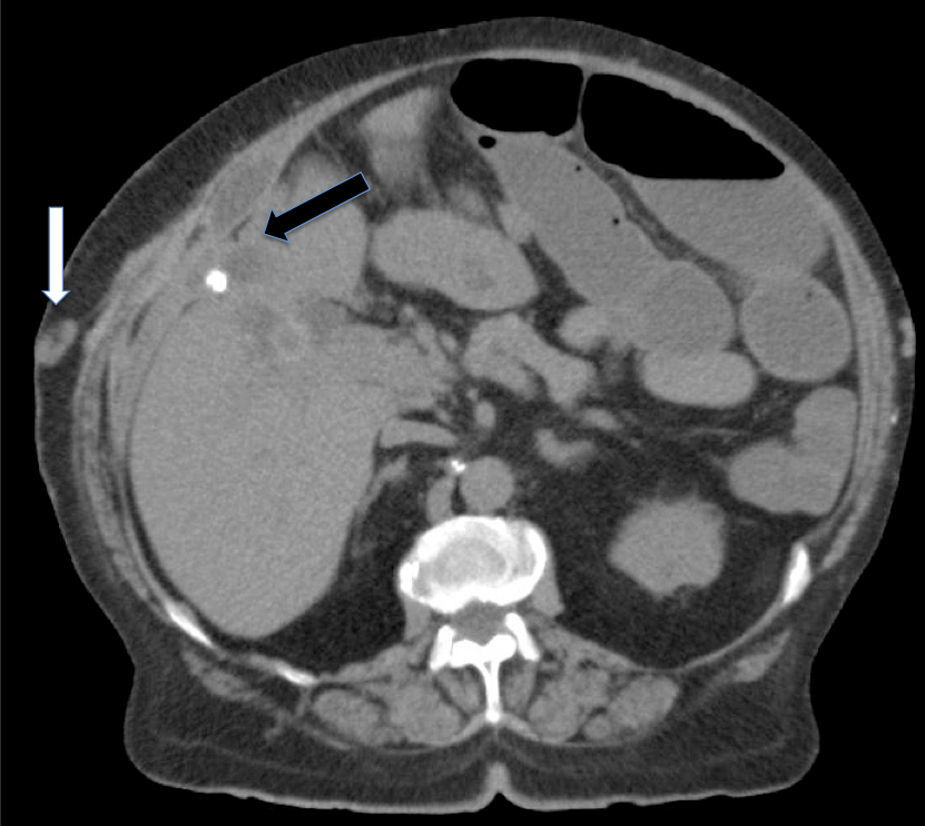
Ten days after the surgery, she began to have abdominal pain and leukocytosis (16320×106/L), with no alterations in the liver profile. Abdominal computed tomography (CT) (Fig. 2) revealed: calculi in the small bowel without causing gallstone ileus, dilated loops of small bowel related to stenosis of the anastomosis, cholelithiasis, slight dilatation of the bile duct and infected collection in the right hypochondrium. Urgent laparotomy was performed, observing: the gallbladder firmly attached to the bile duct and peritoneum of the right hypochondrium and retracting the latter, a cholecystocholedochal fistula (Mirizzi II [McSherry classification]) that affected more than 50% of the circumference and severe inflammation of the rest of the extrahepatic bile duct. The gallbladder was perforated to the subcutaneous tissue, where there was a purulent bile collection connected to the cutaneous orifice (CCF). The following were performed: cholecystectomy and resection of the extrahepatic bile duct, hepaticojejunostomy on common bile duct, drainage of the subcutaneous collection and excision of the cutaneous orifice. Inflammatory stenosis of the intestinal anastomosis was detected, so a new anastomosis was performed. During the immediate postoperative period the patient presented a low-output bile leak (<50cc/24h) through a subhepatic drain, which was resolved conservatively in 12 days. The histology report revealed chronic inflammatory signs in the gallbladder and bile duct. Culture of the subcutaneous collection grew Escherichia coli. The patient was hospitalised for 22 days. During the 24-month follow-up, she has not presented any clinical or laboratory abnormalities related with the intervention.
The first case of CCF was described by Thilesius in 1670 and Courvoisier described 169 cases in 1890, but between 1966 and 2014, only 55 cases of CCF have been published in the medical literature (search strategy in PubMed: “cholecystocutaneous fistula”, unlimited 1966–2015).1–10
CCF generally occurs as a complication of gallstone disease, although it can be caused by a tumour.3,6 Ingestion of steroids, polyarteritis nodosa, gliomatosis and vasculitis of the gallbladder, previous trauma or typhoid infection have been proposed as suspect predisposing factors of CCF.1,2,5 CCF usually occurs after an episode of acute cholecystitis.3 Cystic duct obstruction due to gallstones, or exceptionally a tumour, increases the intramural pressure causing mural necrosis and, in the course of time, perforation.3,5,9,10 On extremely rare occasions, the gallbladder attaches to the wall and ultimately perforates the subcutaneous tissue. It eventually connects to the skin, giving rise to a CCF.8,9
CFF can present in 2 forms: as a cutaneous orifice that discharges bile, pus or calculi, with no changes in the patient's general condition or few symptoms; or as a subcutaneous tumour in the right hypochondrium, with inflammatory signs, that can be accompanied by impairment of the general condition.6
A CCF accompanied by an internal fistula has been reported on only 3 occasions, 2 to the duodenum and 1 to the small intestine.6,9 We found no previous cases of cholecystocholedochal fistula (Mirizzi II) and concomitant CCF in our literature search.
The abscess and sometimes the fistula track can be seen on abdominal CT or magnetic resonance imaging.1,4,5,8 A fistulography may occasionally be necessary.1,2,8 Differential diagnosis should consider infected epidermal cyst, tuberculosis, gangrenous pyoderma and costal osteomyelitis.2,10
Treatment should be adapted to the form of onset and the patient's medical conditions. If the symptoms start as a wall abscess, surgical drainage should be performed and antibiotics administered.3,8 Although the CCF closes in around 20% of patients, recurrence is practically universal.1,9 Closure is only advisable in very elderly patients and those with severe comorbidities. Deferred treatment consists of cholecystectomy, drainage of the subcutaneous collection and excision of the fistula track.4–6,8 Percutaneous cholecystostomy has been used as a bridging treatment between the initial phase and the definitive surgery.6
The presence of an orifice or abscess in the right hypochondrium, or more rarely in another location, that drains bile or gallstones should raise the possibility of a CCF. If only pus is observed, the diagnosis is more difficult and fistulography may be useful. Immediate or deferred laparotomic cholecystectomy is usually the most effective treatment.
Please cite this article as: Ramia JM, de la Plaza R, López Marcano A, Ramiro C, Valenzuela Torres JC. Fístula colecistocutánea y fístula colecistocoledociana (Mirizzi II). Gastroenterol Hepatol. 2016;39:599–600.