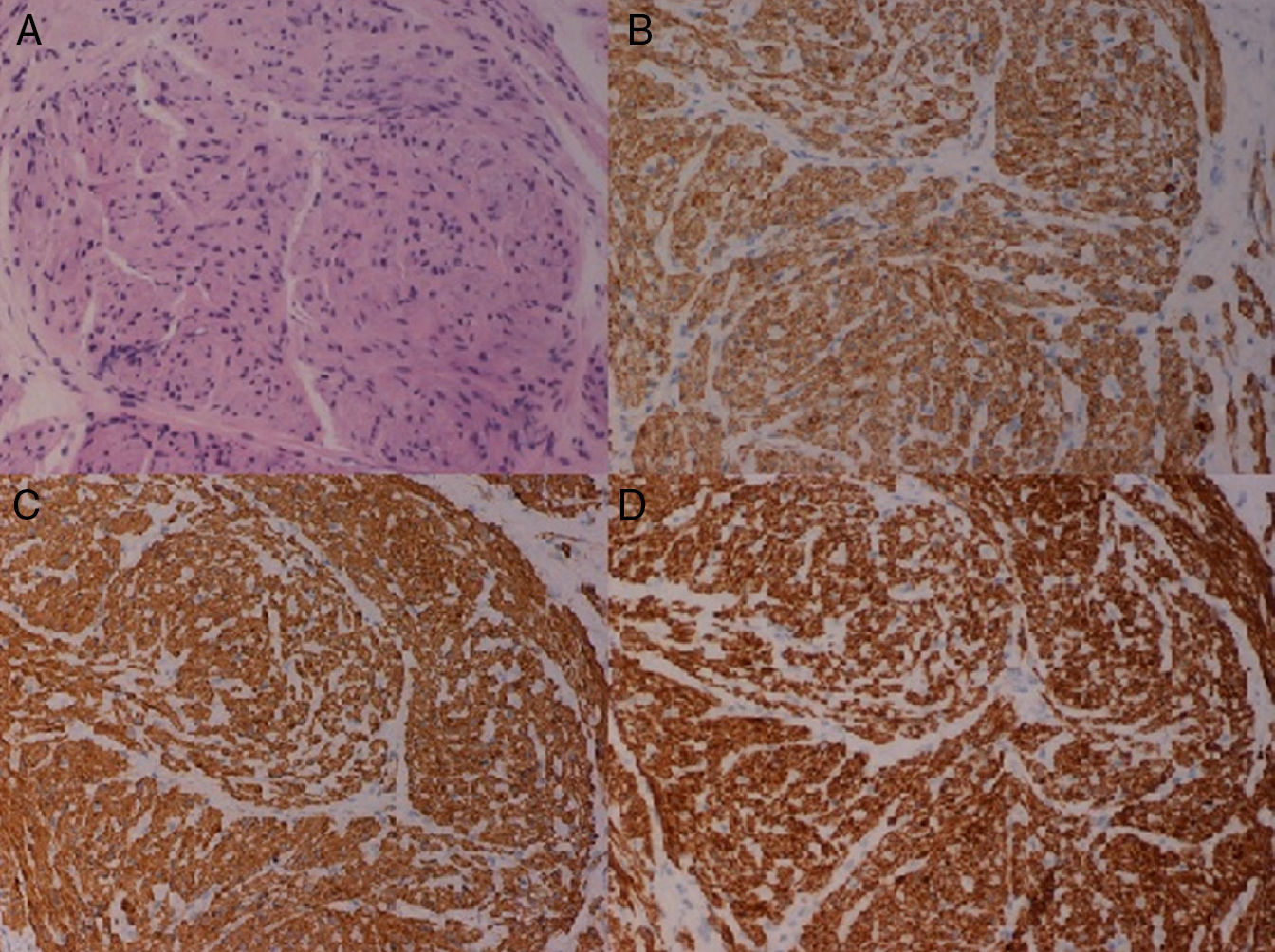
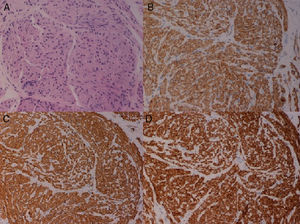
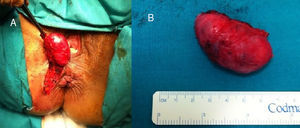
Leiomyoma is a tumor strain that derives from the smooth muscle fibers and develops in the regions where these fibers are present. In the digestive tract, the anorectal location is uncommon and is usually diagnosed late due to intraluminal growth in over 50% of the cases. Given the exceptional location, we present the case of a 49-year-old woman who sought medical attention for a tumor of 7-month progression in the perineal region that had progressively increased in size. She was asymptomatic during this period and did not present with tenesmus, rectorrhagia, or proctalgia. Physical examination revealed a right perianal tumor of 3cm in diameter that was mobile and had an elastic consistency to the touch (fig. 1). Nuclear magnetic resonance imaging showed a well-defined, nodular, oval-shaped lesion that measured about 5cm in diameter, with heterogeneous contrast medium uptake. Its location was intersphincteric and adjacent to the intergluteal fold. An ultrasound image identified a hypoechogenic ovoid nodule with abundant vascular flow. A thick needle biopsy was performed and the preoperative anatomopathologic diagnosis was leiomyoma (fig. 2). The patient was operated on and an oval intersphincteric tumor with a smooth external surface and a conglomeratic aspect was removed; there was no solution of continuity with the superficial fascicule of the external anal sphincter and minimum continuity with residual fibers of the internal anal sphincter (fig. 3). Patient progression was favorable and she is presently asymptomatic, with no tumor recurrence and with complete sphincteric continence.
Leiomyoma was first described by Virchow in 1854, defining it as a benign tumor of mesenchymal origin dependent on smooth muscle fibers. It represents approximately 3.8% of all the benign, soft tissue tumors and its pathogeny continues to be debated today.1–3It is classified into 2 variants: superficial and deep. One of the better known examples of the superficial variant is angioleiomyoma of the female genital tract. Leiomyoma of the deep variant, described by Kilpatrick and Billings, is in turn classified as somatic and as retroperitoneal. Unlike the somatic leiomyomas, 20% of the retroperitoneal type show low levels of mitotic activity. Leiomyomas of the superficial variant tend to more often affect the extremities and they affect both sexes, whereas the retroperitoneal variant involves the pelvic area in postmenopausal women.
The organ most commonly affected in the gastrointestinal tract is the stomach, followed by the small bowel. The esophagus, colon, and rectum are less frequent locations.4,5 The anorectal location presents in under 0.1% and is considered an extraordinary entity with an overall rectal tumor incidence of 1:2000. Tumor growth is intraluminal in 50% of the cases, extrarectal in 30%, intra and extraluminal in 10%, and intramural in the remaining 10%.6
The clinical course of these tumors varies widely, and it is the location and vascularization that determine patient symptomatology.7 Due to their submucosal origin, they are often asymptomatic in their initial stages. Later, when they reach significant sizes, anal and perineal pain, bowel transit alterations, pruritus, rectorrhagia, or tenesmus are some of the most frequent symptoms for which the patient seeks medical attention. Our patient was asymptomatic during the progression of tumor growth, probably being in the initial stage of the disease.
Tumors of the deep soft tissues tend to grow larger than the superficial variant due to the fact that they go by undetected and are diagnosed in the late stages.
The clinical symptoms of the patient, together with a complete physical examination including endoscopy with biopsy are usually essential for diagnosis. Imaging techniques are useful for preoperative staging because they enable the relation with the sphincters and urogenital tract to be defined.8 In the case of our patient, the preoperative studies performed allowed us to make the diagnosis and plan the surgical intervention.
In relation to management, complete surgical resection of the tumor is the treatment of choice. Easily accessible intrarectal leiomyomas can be transanally resected. Low anterior resection or abdominoperineal amputation should be reserved for those cases in which local resection cannot be performed due to tumor size or wall involvement. Another approach should be contemplated, which could be transperineal, pararectal, or transvaginal, when the tumor is extrarectal.9 Our patient developed a progressive increase in tumor size with no other accompanying symptoms, and so the decision was made to extirpate the tumor.
These tumors recur in up to 40% of the cases and up to 10% recur as leiomyosarcomas; this appears to be related to incomplete resection or a size greater than 5cm. The fact that there is the possibility of recurrence, even in low-grade tumors, makes follow-up essential.9,10
In conclusion, leiomyoma of the anal sphincter is a rare entity in the gastrointestinal tract, and because of its location it is important to make the correct differential diagnosis with other entities that develop at the same site. When there is suspicion, biopsy is recommended, as well as an imaging study to determine the relation with the sphincteric complex and adjacent organs. In this manner, the adequate surgical approach can be planned.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: García-Santos EP, Ruescas-García FJ, Estaire-Gómez M, Martín-Fernández J, González-López L. Leiomioma anorrectal. Presentación de un caso y revisión de la literatura. Revista de Gastroenterología de México. 2014;79:58–60.