Through the use of an experimental design with a baseline and post intervention, the aim of this study was to investigate the effectiveness of a psychological intervention in increasing public health and communication skills for caregivers.
MethodsThis randomized controlled trial was designed in Razi Hospital in Tehran, Iran. A sample size of 90 participants was evenly divided into intervention and control groups. The intervention group was given routine treatments and also participated in planned educational sessions. The planned educational program was implemented in 10 group sessions over a period of 5 weeks. Each session lasted 45–60min. The outcome measures were: (1) improvement in the caregiver's general health as measured by the changes in their General Health Questionnaire (GHQ) scores taken at baseline and post intervention and (2) changes in the caregiver's communication skills, measured by the communication skills questionnaire taken at baseline and after 3 months.
ResultsAn independent samples t-test revealed that there was a significant difference between the two groups in the mean scores of communication skill at baseline (P<0.001). To adjust for the effects of pre-intervention scores on the post-intervention results, a covariance analysis was used. Consequently, differences between the mean scores of post-intervention GHQ total, GHQ subcategories, and communication skills in the intervention group and the control group were statistically significant (P<0.001).
ConclusionResults of our study confirm that providing education on effective communication skills can be an effective, cost-efficient, and convenient strategy to reduce the psychological complications for caregivers and improve the care of patients living with schizophrenia.
Schizophrenia is one of the most severe mental disorders in the world and seriously impairs cognition, affection, and perception.1 According to the World Health Organization's2 report, about 21 million people around the world are struggling with schizophrenia.2 Besides the immediate mental and physical health effects of schizophrenia on the individual, their caregivers and family members face significant added distress.3–5 Families who live with an individual with schizophrenia deal with a multitude of challenges in their work and social communications, especially after the patient's discharge from a hospital.6–8 The amount of time spent living with an individual with schizophrenia and the age of the caregiver are associated with higher rates of distress.9 Caregivers can undergo considerable stress due to the long-lasting nature of nursing someone with schizophrenia.
It has been reported that 60% of chronic schizophrenia patients live with at least one other family member. According to the General Health Questionnaire (GHQ), approximately 25% of caregivers for those living with schizophrenia met the criteria of having their own mental disorder.10 High levels of depression was seen among the caregivers of schizophrenic patients11–13 despite having no history of earlier mood disorders.14,15 The most common variables associated with depression among schizophrenia caregivers included gender, socioeconomic status, marital status, number of family members, educational level, relationship to the patient, and nursing distress.16,17 Caregivers and the family members of patients with schizophrenia could benefit from family health interventions and psychoeducational plans.9 Patients with schizophrenia require an integrative and extensive care plan that provides for their physical and psychological needs, helps to reduce the caregiver's distress, and encourages family members to be part of the intervention.18
Information regarding schizophrenia, the treatment plan, and coping strategies could be provided in psychoeducational programs. The meta-analyses found a positive association between psychoeducation plans and improved expressed emotion, less acute episodes of the disorder, and a decrease in multiple inpatient treatments.19,20 Psychoeducation involves explaining the main aspects of schizophrenia to the caregiver and emphasizing the necessity of pharmacotherapy, seeking rehabilitation, and reinforcing the patient's social communication and support system.21 Behavioral family management, psychoeducational family interventions, and family therapy are among the various family intervention methods that aim to decrease both patient and family distress. A recent study concluded that psychoeducation was the most effective method in decreasing the distress of mothers who act as the main caregiver for a child with schizophrenia.22,23
Considering the aforementioned points, the aim of this experimental study is to investigate the effectiveness of a psychological intervention (specifying treatments and the symptoms of schizophrenia) in increasing general health (GH) and communication skills (CS) through a baseline and post-intervention. It was hypothesized that: (1) the planning intervention will have a significant effect on the GH outcome (e.g., physical, social, and psychological outcomes) compared to the baseline condition; and (2) the implementation intervention will have a significant effect on CS compared with the baseline condition.
Material and methodsSettingAt present, centers do not provide support services to meet the specific needs of families with a schizophrenic member. Instead, families can only get support systems at psychiatric or general healthcare centers. Other challenges faced by this population are a lack of nonmedical services, like family interventions, the general societal stigma attached to psychotic disorders, and the general lack of knowledge regarding psychiatric disorders. Cumulatively, these issues and barriers may cause significant distress among families with psychiatric patients. Lastly, there is a dearth of trained experts who could offer psychoeducational programs in Iran.23
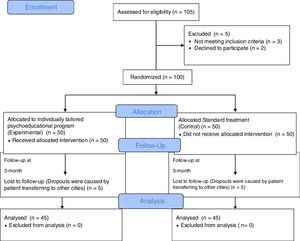
Ethical approvalApproval for the study was obtained from the Ethics Committee at the University of Social Welfare and Rehabilitation Sciences and was conducted in accordance with the Consolidated Standards of Reporting Trials (CONSORT)24 (Fig. 1) (Ethic Approval/Registration Number: IR.USWR.REC.1395.170). Written consent was obtained from the patients and their families. All participants were informed about the purpose of the study and their right to withdraw at any time, and they were assured that all personal information would remain confidential.
Participants and samplingThe target population were caregivers referred to psychoeducational programs. Families were also invited to take part in the study when visiting the hospital. This two-armed blind randomized controlled trial was designed in Razi Hospital in Tehran, Iran, where recruited caregivers were referred for psychoeducational programs with their families. The sample of 90 participants was evenly divided into intervention and control groups. We used a blocked randomization method. In this method, subjects were assigned to blocks. Then, within each block, subjects were randomly assigned to treatments. Each group had four participants. The intervention group was given routine treatments and also participated in the planned educational sessions. Sampling was available and continuous, but the division of people into two groups was randomly assigned through EPI INFO software.
Fig. 1 depicts the sample design. The inclusion criteria included: (1) identifying as the primary caregiver of the patients in treatment sessions and (2) no history of psychological illness among the caregivers. The exclusion criteria included: (1) having more than one family member as a patient in the hospital and (2) participating in a psychoeducational mental health intervention program in the past.
Sample sizeThe sample size for this study was calculated using a formula by Lemeshow et al.25:
In the intervention group, a power of 90%, a confidence interval of 95%, a pooled standard deviation of 17.21, and a baseline and post-test mean score of 55.42 and 46.57, respectively, were used. An estimated sample size of 40 participants was calculated. Taking into consideration a 10% dropout rate, a sample size of 45 participants was calculated for each group.
ProcedureBefore starting the sessions, a trained researcher stated the goals of the study. The researcher also explained the symptoms and behaviors of schizophrenia and their effects on caregivers during a meeting to the families of schizophrenic patients that were participating in the research. Finally, the researchers completed the general evaluation and the brief criterion form for psychiatry for each group. Afterwards, the planned educational program was implemented in 10 group sessions during the timespan of 5 weeks. Each session lasted 45–60min, and the main topic of each session was as follows:
- 1.
The first session was held as an introduction and assessment of requirements and as a mechanism to develop trust between families and instructors.
- 2.
At the second meeting, schizophrenia, its treatments, the symptoms, and its effects were explained to the attendees.
- 3.
At this meeting and all subsequent sessions, a review of previous sessions was presented and then, the positive and negative effects of antipsychotic drugs and the problems related to antipsychotic drugs were discussed.
- 4.
This topic discussed schizophrenic relapse and its symptoms. The signs and effects for the patients and their families were explained.
- 5.
The importance of family CS and the improvement of this effective skill set was discussed.
- 6.
This session covered effective CS with patients when they are presenting symptoms, skills for coping with some of the patients’ symptoms, and a question-answer group discussion.
- 7.
This session discussed expressing emotion and the emotional environment for families and coping with the patient's negative emotions.
- 8.
This topic included stress management and the ways to reduce stress for the family members of the patients.
Sessions 9 and 10 were a review of the previous sessions and an explanation of relaxation methods and ways to practice relaxation.
MeasurementsThree questionnaires were used to gather data. Initially, the caregivers completed a personal information questionnaire (age, sex, level of education, marital status, and their relationship to the patient). The GHQ was used to assess physical and mental health and social performance.26 The GHQ has 28 questions and 4 subcategories, including: (1) physical symptoms, (2) anxiety symptoms and sleep disorder symptoms, (3) social performance symptoms, and (4) depression symptoms. The scoring system was from 0 to 3 for each question, and any criteria from 6 to the total score of 22 indicated the existence of psychiatric disease symptoms. Further, we used the CS questionnaire that has 19 questions. Every question had varied responses (very low to very good).
Outcome measuresThe outcome measures were: (1) improvement in the caregiver's GH measured by the change in GHQ score taken at baseline and at post-intervention and (2) change in the caregiver's CS as measured by the CS questionnaire taken at baseline and after 3 months.
Data analysisData analysis was performed with Stata (version 12), using descriptive and inferential methods. We conducted an independent samples t-test to compare the GH and CS dimensions for the control and intervention groups. Because only two measurements were utilized, differences in scores in both GH and CS from baseline through post-measurement were evaluated between the two groups by using analysis of covariance (ANCOVA) with baseline values of GH or CS, respectively, as covariates.
ResultsA total of 90 caregivers completed the study. Seven participants (three from the experimental group and four from the control group) dropped out before completion of the study. Table 1 presents the relationship between categorical demographic characteristics and GHQ scores. The caregivers with higher levels of education and who were retired had significantly higher mean scores. Compared to other relatives, spouses had a higher GHQ score. No significant differences were observed for GHQ scores among gender or age categories. Table 2 shows pre-intervention scores in the control and intervention groups. An independent samples t-test revealed that there were no statistically significant differences between the intervention and control groups at baseline in the mean score of GHQ total and GHQ subcategories. However, there was a significant difference between the two groups in the mean score of CS at baseline.
Relationship between categorical demographic characteristics and GHQ scores.
| Covariate | GHQ (N=90) Mean±SD | P-value | |
|---|---|---|---|
| Age (year) | <50 years | 36.84±1.61 | 0.4 |
| >50 years | 39.24±1.91 | ||
| Sex | Male | 38.68±2.66 | 0.87 |
| Female | 38.22±1.53 | ||
| Educational history | Yes | 42.22±1.78 | 0.06 |
| No | 36.74±1.57 | ||
| Education | 35.49±1.88 | 0.002 | |
| >Diploma | 43.9±1.19 | ||
| Employment status | Employ | 55±4.00 | 0.000 |
| Free | 24.6±5.23 | ||
| Unemployed | 37.66±8.83 | ||
| Housewife | 36.2±1.30 | ||
| Retired | 53.8±4.60 | ||
| Caregivers relationship | Father | 50.2±3.06 | 0.0004 |
| Mother | 33.47±2.03 | ||
| Sister | 40±2.26 | ||
| Brother | 34±4.56 | ||
| Father and mother | 36.09±4.32 | ||
| Husband and wife | 43.33±1.48 | ||
Mean scores of the control and intervention groups before psychoeducational program.
| Variable | Group | P-value | |
|---|---|---|---|
| Control (N=45) Mean±SD | Intervention (N=45) Mean±SD | ||
| Physical | 9.02±4.68 | 8.02±3.94 | 0.17 |
| Sleep problem | 7.97±5.06 | 7.75±3.48 | 0.1 |
| Social | 11.95±4.8 | 9.08±3.31 | 0.17 |
| Depression | 12.86±4.66 | 9.08±3.31 | 0.1 |
| GHQ total | 41.82±14.47 | 34.95±10.21 | 0.12 |
| CS | 39.88±10.17 | 37.44±7.05 | 0.002 |
To adjust for the effects of pre-intervention scores on the post-intervention results, a covariance analysis was used. Consequently, differences between mean scores of post-intervention GHQ total, GHQ subcategories, and CS scores in the intervention and control groups were statistically significant (P<0.001) (see Table 3).
Covariance analysis of the effect of psychoeducational program on caregiver's GH and CS.
| Variable | df | Mean square | F | P value |
|---|---|---|---|---|
| Physical | ||||
| Pre-intervention | 1 | 501.747 | 78.163 | <0.001 |
| Post-intervention | 1 | 410.948 | 64.018 | <0.001 |
| Sleep problem | ||||
| Pre-intervention | 1 | 1010.200 | 164.988 | <0.001 |
| Post-intervention | 1 | 317.891 | 51.919 | <0.001 |
| Social | ||||
| Pre-intervention | 1 | 869.154 | 132.950 | <0.001 |
| Post-intervention | 1 | 1225.464 | 187.453 | <0.001 |
| Depression | ||||
| Pre-intervention | 1 | 803.354 | 147.402 | <0.001 |
| Post-intervention | 1 | 537.323 | 98.590 | <0.001 |
| GHQ total | ||||
| Pre-intervention | 1 | 8585.792 | 352.049 | <0.001 |
| Post-intervention | 1 | 8722.722 | 357.663 | <0.001 |
| CS | ||||
| Pre-intervention | 1 | 279.817 | 6.068 | 0.016 |
| Post-intervention | 1 | 47,149.914 | 1022.476 | <0.001 |
Obtaining knowledge and practical skills to cope with schizophrenia is one of the greatest needs of caregivers for individuals with schizophrenia. Knowledgeable caregivers usually have greater coping strategies to manage the pressure and problems of supporting those living with schizophreniar.27 This study aimed to understand the effectiveness of a psychoeducational intervention program on caregivers of patients with schizophrenia. Our results show a significant correlation between GHQ scores and education, employment status, and caregiver relationship. The findings of the present study also indicate that participants with a higher educational level reported the highest GHQ scores. Caqueo-Urízar et al. found that caregivers with a positive attitude reported higher education levels28 – similar to the findings of the current study.
Employed and retired participants reported the highest GHQ scores. This finding could be well explained by the likely financial independence and time autonomy of employed and retired caregivers, which allows for the caregivers to plan a more appropriate schedule for their caregiving routines. Data from the current study found that fathers had the highest GHQ scores in caring for patients with schizophrenia, compared to other family members. Such scores may illustrate the cultural role of fatherhood in Iranian families and their supportive role in economic, social, and emotional aspects.
Our findings found a significantly higher mean GHQ score and CS score after completing the educational program in the intervention group. In other words, the educational intervention improved the GH of caregivers by providing them with useful and applicable information. This is consistent with the results of Sharif et al. in a study that illustrated the effectiveness of a psychoeducational intervention in increasing GHQ scores among family members of schizophrenic patients.23 Compared to the control group, results of the present study found a significant increase in the mean score of a caregiver's social function in the intervention group, and, as a result, caregivers improved their interpersonal relationships after gaining an accurate perception of schizophrenia. Magliano et al. also reported that psychoeducational interventions could dramatically improve caregivers’ social relationships.29
Caregiving for schizophrenic patients can bring forth various health complications, both physically and mentally. Depression is known to be among the greatest psychological side effect of caring for psychiatric patients.16 Our findings illustrated a significant decrease in the total mean score of depression in the intervention group, i.e., completion of the psychoeducational program, compared to the control group. This was consistent with Dyck et al.’s study that showed the effectiveness of psycho-social interventions in reducing depression among caregivers of patients with schizophrenia.30 Physical illnesses and sleep disorders are also among the most common issues faced by the families of psychiatric patients.31,32 Previous studies have found that the psychological distress of schizophrenic patients may increase a family member's physical disorders 3 times that of an average person.33
Given the effectiveness of psychoeducational interventions on reducing physical issues and sleep disorders, it is imperative to acknowledge the physical and psychological needs of caregivers for schizophrenic patients when designing intervention and treatment plans for schizophrenia. This may not only improve a family member's quality of caregiving, but also enhance the individual's physical and psychological health. Prior investigations have outlined the importance and effectiveness of psychoeducational interventions for caregivers of psychiatric patients in healthcare settings.34,35 Families are known to be the most important form of social support for schizophrenic patients and the best at noting signs and symptoms of reoccurrence. However, it is imperative for the caregiver to be knowledgeable about this disorder and aware of different coping strategies to relieve stress given that a lack of sufficient information and skills to manage the patient's behavior could exacerbate the disease.31,36 Furthermore, several studies have reported that teaching problem-solving skills, improving CS, and providing information about the disease and its treatment to families can encourage them to engage in social activities and reduce psychological stress.37 Green et al. also documented that increasing the use of CS techniques could significantly raise the efficiency of care.38 A study conducted by Michel et al. sought to understand the impact of CS on nursing and found that training caregivers significantly increased the quality of their caregiving behaviors.39 In their study on caregiver burdens and psychiatric symptoms in patients with schizophrenia, Sharif et al. found that teaching skills, such as CS, to the family could significantly improve the patient's disease and reduce its burden.23 Effective communication is a key nursing skill and impacts the quality of care. The aforementioned research illustrates the effectiveness of providing CS in improving patient care, but Włoszczak-Szubzda et al. and Nørgaard et al. have called the abovementioned findings into question and did not find a caregiver's CS to be of any importance.40,41
This study focused on the training of CS for caregivers, covered a caregiver's lack of information about the treatment and symptoms of schizophrenia, and provided new skills through psychological interventions. However, the present study falls short of illustrating practical (rather than theoretical) education, where better results may be found. Another limitation of our study was limiting the sampling to only one hospital. Considering the duration of the study and only one follow-up after completion of the intervention, it is recommended that subsequent studies should be carried out for a longer time frame to evaluate CS and GH at different intervals.
ConclusionThe results of our study confirm that psychoeducational programs can be an effective, cost-efficient and convenient strategy to reduce the psychological complications for caregivers. Strengthening CS can increase a caregiver's capability to provide care by improving verbal and nonverbal communication. Most Iranian health and hygiene service plans focus only on the patients, thus neglecting their families. Therefore, holding workshops to teach CS to caregivers for patients with schizophrenia can provide caregivers with training in problem-solving approaches and gradually increase their quality of care. Such an approach may be effective in other settings for patients with other psychological disease. We suggest that this intervention might be effective in teaching CS to caregivers of patients with disorders such as Alzheimer's and dementia. It is also recommended for future studies to design and implement interventions and evaluate their effectiveness for psychological issues, such as social support and depression. In addition, it would be appropriate to conduct various interventions for caregivers by utilizing scheduling patterns the precede-proceed model.
Ethical approvalAll procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consentWas obtained for all participants.
Authors contributionsStudy design: BA and MN. Data synthesis: OR, YM and MSN. Drafting the manuscript: FF, NA, YS, ME, EA, DAGH, JH and ML. Critical revision of the manuscript: DA, BD, and SN. Revision of manuscript: KW and MGh.
FundingThis research was funded by Psychosis Research Center, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Conflict of interestThe authors declare that they have no competing interests.
The authors would like to acknowledge the contributions of Heidar Mohammadi to the work of this review of the evidence.