To describe the perceptions of nurses in neonatal units on pain management, meet the educational profile and describe the use of pain assessment tools and non-pharmacological management for treatment.
MethodsCross-sectional descriptive multicentre study, developed during the months of February to September 2015, in the neonatology services of three hospitals at the Community of Madrid, Spain. Data collection was performed through an ad hoc questionnaire on paper or electronically using Survey Monkey platform.
ResultsThe sample consisted of 142 professionals, with a response rate of 55%: 47.9% (68) confirmed they had received specific training in pain management; 39.5% (56) stated that pain is regularly assessed in the unit; only 43.6% reported using validated scales, the most used being the Premature Infant Pain Profile (PIPP). As for the non-pharmacological management, swaddling and non-nutritive sucking it is the most used, followed by sucrose. Intravenous cannulation was identified as the most painful procedure.
ConclusionsPain management is in the process of improvement, because of training and because there is little pain assessment using validated scales. The improvement in the use of non-pharmacological management for the relief of pain in minor procedures is noteworthy.
Describir las percepciones del personal de enfermería de unidades neonatales sobre el manejo del dolor, conocer el perfil formativo y describir el uso de herramientas de valoración del dolor y de medidas no farmacológicas.
MétodoEstudio multicéntrico observacional descriptivo transversal desarrollado durante febrero-septiembre de 2015 en los Servicios de Neonatología de tres hospitales de la Comunidad de Madrid, España. La recogida de datos se realizó a través de cuestionario de elaboración propia enviado en formato papel o electrónico utilizando la plataforma Survey Monkey®.
ResultadosLa muestra consta de 142 profesionales (tasa de respuesta: 55%). El 47,9% (68) afirman que han recibido formación específica sobre el manejo del dolor. El 39,5% (56) refieren que el dolor se evalúa de forma habitual en su unidad. Tan solo el 43,6% refieren utilizar escalas validadas, siendo la PIPP la más usada. La contención y la succión no nutritiva son las medidas no farmacológicas más usadas, seguidas de la sacarosa. Se identifica la canalización intravenosa como el procedimiento más doloroso.
ConclusionesEl manejo del dolor está en vías de mejora, ya sea por la formación como por la escasa evaluación a través de escalas validadas. Destaca la mejora en el uso de medidas no farmacológicas.
The consequences of pain in the neonatal population are highly important, so that proper pain management has to be a core objective. Although a large amount of evidence supports the above statement, in clinical practice major deficiencies still exist in pain management. This is chiefly due to persistence of myths and beliefs among healthcare professionals, a lack of training and variations in clinical practice.
What is the contribution of this?This is the first study undertaken in Spain to describe the perceptions of nursing staff regarding pain management in Neonatal Departments. It covers three hospitals in the Community of Madrid and no findings differed from those published in international studies. It found that pain management is still improving.
Implications of the studyTo learn which areas of neonatal pain control could be improved, to design training strategies and strategies to improve the quality of care.
Hospitalised newborn babies undergo a very high incidence of painful and/or stressful procedures. This incidence stands at an average of 7.5–17.3 painful procedures per newborn baby/day, while premature infants are the most exposed to these.1 The consequences of continuous and repeated exposure to pain in the newborn goes beyond alterations to pain sensing systems, as it also affects growth, cognitive and motor functioning, behaviour and personality, and it also leads to changes in brain structure and functioning.2–4 Due to this incidence and magnitude, good management of pain must be a core objective in all neonatology.
Good pain management commences with evaluation of the same, continues with the establishment of measure to treat it and then subsequent evaluation. The first limitation in the management of neonatal pain is that there is no gold standard for measuring pain, and newly born infants are unable to express it in words. Nevertheless, many scales make it possible to monitor pain using physiological indicators, behaviour and other indicators based on facial expression.5 The most widely used scales are said to include: Premature Infant Pain Profile – Revised (PIPP-R),6 Crying, Requires oxygen to maintain saturation >95%, Increased vital signs, Expression, Sleepiness (CRIES)7 and the Neonatal Infant Pain Scale (NIPS).8 However, these scales may be complex and hard to use in a clinical context, while they also require specific education and training.9
It is recommended that non-pharmacological be used to relieve pain during minor procedures in newborn infants,10 such as heel puncture, the aspiration of secretions or canalising peripheral venous accesses, etc. These are defined as contextual, psychological and behavioural actions that do not use the effect of an active ingredient.11 The most widely used non-pharmacological methods in neonatal infants are identified as non-nutritious suckling, holding, breast feeding (BF) and/or extracted mother's milk (EMM) and a sling. Oral sucrose (and products containing sugar) have recently come to be considered pharmacological methods.12
The American Academy of Paediatrics (AAP)12 and the International Association for the Study of Pain (IASP), as well as institutions13 and studies,14,15 attribute neonatal pain management deficits to the persistence of myths and beliefs among healthcare professionals, together with lack of knowledge, lack of training and variations in clinical practice.
There are few clinical practice guides and/or protocols in Spain for managing neonatal pain. A study undertaken in more than 20 hospitals in different autonomous communities in Spain showed that the measures used to control pain during frequent minor procedures were still inappropriate and rarely implemented.16
There is little evidence in our field regarding the knowledge and attitudes of healthcare professionals in managing neonatal pain. Only the study by Ponsell17 was found. This uses a qualitative approach to analyse the perceptions of different healthcare professionals on the management of infant pain. It shows that beliefs in connection with pain persist, with a certain tendency to consider infant pain as something that forms part of hospital culture.
However, several international studies have been performed in Japan, the United States, the United Kingdom and Turkey, among others, on the perception of nurses and neonatologists in neonatal units regarding the management of neonatal pain.18–20
Due to all of the above considerations, the overall aim of this study is to describe the perceptions of nursing personnel regarding pain management in Neonatology Departments in three hospitals in the Autonomous Community of Madrid.
MethodThis multicentre observational descriptive transversal study was undertaken from February to September 2015 in the Neonatal Departments of three hospitals in the Autonomous Community of Madrid (Spain). Two hospitals are care level IIIC and one is IIIA. All three Departments have open door policies.
This study targeted the nursing staff (nurses and auxiliary nursing care technicians [ANCT]) who work in the said Neonatal Departments, including intermediate care neonatal units (ICNU) and/or the Neonatal Intensive Care Unit (NICU). The inclusion criteria were: nursing staff who had worked in the Neonatal Department for more than 3 months. Those participants who answered fewer than 80% of the items in the questionnaire were excluded.
The sample size was not predetermined, as there was access to all of the study population.
An ad hoc questionnaire was designed to achieve the study objective. It was prepared by expert neonatal care researchers after a review of the literature on this subject, and its content was validated by a previous pilot trial. This questionnaire covered the four dimensions studied: the socio-professional and educational profile of the nursing staff, evaluation of neonatal pain, the use of non-pharmacological measures and perception of pain.
The following indicators/variables were used for the dimension of the socio-professional and educational profile: the unit in which respondents work, their profession, sex, year of birth, length of working experience in neonatal units (years), type of shift and training received in the last 5 years on pain management, and the quality of their training in pain management. In the evaluation of neonatal pain dimension they described the availability of a protocol in their unit, frequency of evaluation and the tools they use to evaluate pain.
In the dimension of the use of non-pharmacological measures, the questions were on the frequency of use of sucrose or extracted mother's milk, non-nutritious suckling and holding, as well as a record of the amount of sucrose.
Lastly, the perception of neonatal pain was examined by using questions about the utility of the tools, the perception of painful procedures, perceived efficacy of sucrose and extracted mother's milk, and overall evaluation of pain management in their unit. A space was also left open for observations or remarks on the management of neonatal pain.
The questionnaire contained 15 questions; 11 of these used the Likert 5 point scale in which 1 corresponded to “never” and 5 to “always”. In the other questions 1 indicated “very inappropriate” and 5, “very appropriate”. Three of the questions in the questionnaire were dichotomies (yes/no). The perception of pain intensity during painful procedures was described on a 5-point Likert scale, in which 1 meant “no pain” and 5 meant “very intense pain”. Respecting pain evaluation, there were questions about the scale that was used to measure pain, whether it was evaluated using physiological and/or behavioural signs, or whether no scale of any type was used.
A 10-point scale was used to evaluate the overall management of pain in units, where 1 was the lowest score and 10 the highest.
Data were gathered using anonymous questionnaires in paper or electronic format using the Survey Monkey® platform, depending on whether or not the sample had access to the latter.
Descriptive analysis was carried out overall as well as stratified according to Unit, professional category and hospital. Frequencies and percentages were used to describe the quantitative variables, while the average and standard deviation (SD) were used for quantitative variables; the median and interquartile range (IQR) were used for continuous variables that did not follow a normal distribution.
To establish whether there was a significant statistical association between the variables studied the Chi-squared, Student t and Anova single factor tests were used, together with their non-parametric variants when this was necessary.
The data recorded were analysed using the IBM SPSS® program, version 21.0.
This study was approved by the Clinical Research Ethics Committee of one of the hospitals involved in the study. The questionnaire was accompanied by an information sheet that explained the study and requested voluntary and anonymous participation in it, including consent.
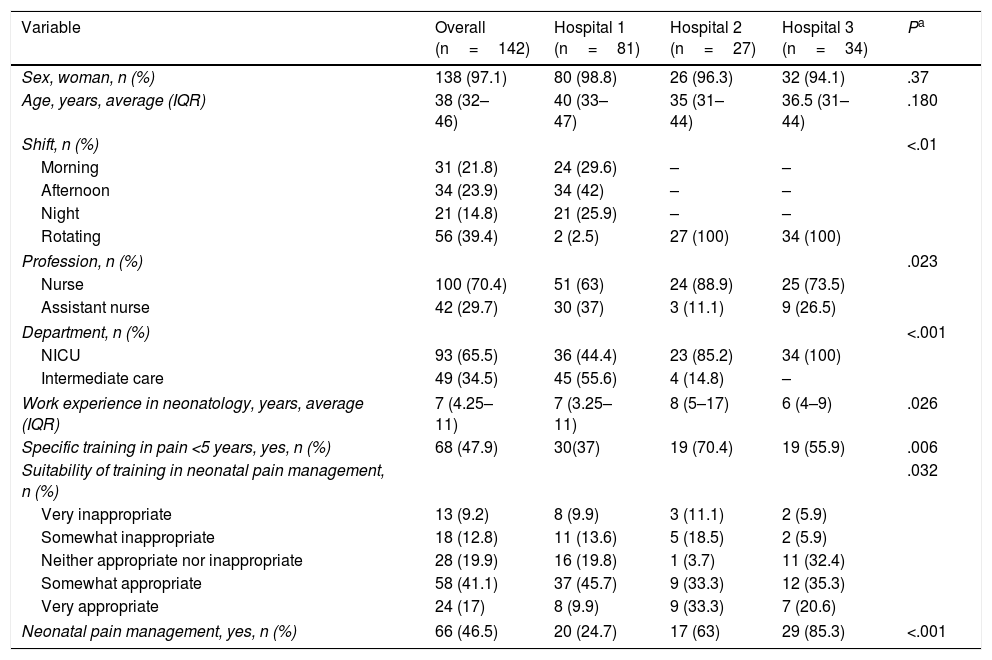
ResultsThe final sample was composed of 142 nursing professionals. The response rate was 55%, and none of the participants were excluded due to failure to answer at least 80% of questions. The socio-professional profile and educational characteristics of the sample are described in Table 1. Five neonatal units took parts, as in two hospitals the NICU and ICNU participated, while in one hospital only a NICU was identified, and the ICNU were included in the NICU.
Socio-professional and training profile (n=142).
| Variable | Overall (n=142) | Hospital 1 (n=81) | Hospital 2 (n=27) | Hospital 3 (n=34) | Pa |
|---|---|---|---|---|---|
| Sex, woman, n (%) | 138 (97.1) | 80 (98.8) | 26 (96.3) | 32 (94.1) | .37 |
| Age, years, average (IQR) | 38 (32–46) | 40 (33–47) | 35 (31–44) | 36.5 (31–44) | .180 |
| Shift, n (%) | <.01 | ||||
| Morning | 31 (21.8) | 24 (29.6) | – | – | |
| Afternoon | 34 (23.9) | 34 (42) | – | – | |
| Night | 21 (14.8) | 21 (25.9) | – | – | |
| Rotating | 56 (39.4) | 2 (2.5) | 27 (100) | 34 (100) | |
| Profession, n (%) | .023 | ||||
| Nurse | 100 (70.4) | 51 (63) | 24 (88.9) | 25 (73.5) | |
| Assistant nurse | 42 (29.7) | 30 (37) | 3 (11.1) | 9 (26.5) | |
| Department, n (%) | <.001 | ||||
| NICU | 93 (65.5) | 36 (44.4) | 23 (85.2) | 34 (100) | |
| Intermediate care | 49 (34.5) | 45 (55.6) | 4 (14.8) | – | |
| Work experience in neonatology, years, average (IQR) | 7 (4.25–11) | 7 (3.25–11) | 8 (5–17) | 6 (4–9) | .026 |
| Specific training in pain <5 years, yes, n (%) | 68 (47.9) | 30(37) | 19 (70.4) | 19 (55.9) | .006 |
| Suitability of training in neonatal pain management, n (%) | .032 | ||||
| Very inappropriate | 13 (9.2) | 8 (9.9) | 3 (11.1) | 2 (5.9) | |
| Somewhat inappropriate | 18 (12.8) | 11 (13.6) | 5 (18.5) | 2 (5.9) | |
| Neither appropriate nor inappropriate | 28 (19.9) | 16 (19.8) | 1 (3.7) | 11 (32.4) | |
| Somewhat appropriate | 58 (41.1) | 37 (45.7) | 9 (33.3) | 12 (35.3) | |
| Very appropriate | 24 (17) | 8 (9.9) | 9 (33.3) | 7 (20.6) | |
| Neonatal pain management, yes, n (%) | 66 (46.5) | 20 (24.7) | 17 (63) | 29 (85.3) | <.001 |
Those participants who had received specific training in the previous 5 years considered their pain-management training to be more appropriate than was the case for those who had received no such training in the previous 5 years (P=.001). The majority of the nursing professionals (79.4%) had received training in the previous 5 years, in comparison with only 20.6% of the ANCT (P=.024). In terms of the neonatal unit, there were no statistically significant differences between the percentage of intermediate care professionals who had received training in the previous 5 years (46.9%) and those in the NICU (48.4%) (P=.87).
A significant relationship was found between having received specific training in the previous 5 years and years of neonatal work experience, with a median duration of experience of 8 (IQR 6–14) years for professionals who had received training in the previous 5 years and 6 (IQR 3–9) years of experience for those who had not received it (P=.006).
Significant differences were also found between type of working shift and having received specific pain training in the previous 5 years (P<.001), as staff in rotating shifts (64.3%), followed by those in the morning shift (58.1%) are the most highly trained, as opposed to those on the night shift (only 14.3%).
Respecting the evaluation of neonatal pain, 39.5% (56) stated that pain was always or almost always evaluated in their unit, while 38.7% (55) said that it was evaluated sometimes, while the corresponding figure for never or almost never was 21.8% (31).
29% (41) of the sample did not answer the question about how pain is evaluated. Of those who did answer it, 43.6% (44) mentioned validated pain evaluation scales and 28.7% (29) cited behavioural and physiological signs, 16.8% (17) only mentioned physiological signs and 4% (4) only cited behavioural signs. 7% (7) said they did not use anything to measure neonatal pain.
Statistically significant differences were found in the stratified analysis of evaluation according to hospital. Evaluation takes places using validated scales in 13% of cases in Hospital 1, in 60% of cases in Hospital 2 and in 87.5% of cases in Hospital 3 (P<.001).
The PIPP scale was the most widely used, followed by the CRIES and the NIPS, in 58.6%, 19% and 10.3%, respectively.
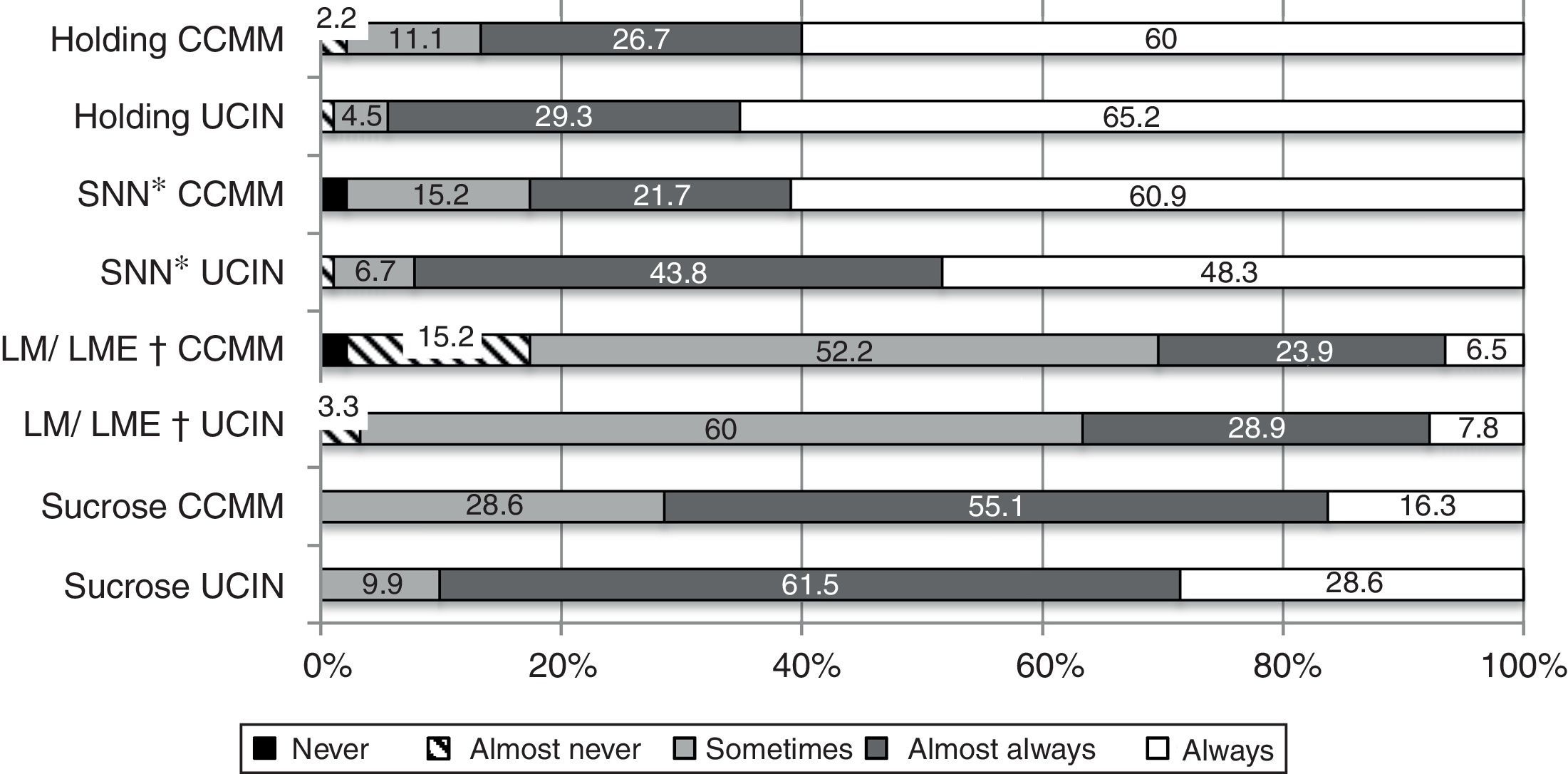
Non-pharmacological measures are shown in Fig. 1, stratified according to Unit.
The amount of sucrose administered was hardly recorded: only 9.3% (13) of the sample mentioned always or almost always recording this, compared to 83.6% (117) who said they never or almost never do so.
Statistically significant differences were found between hospitals in terms of frequency of use of sucrose. It is used regularly by 96% of the sample in Hospital 2, 94.1% in Hospital 3 and 75.3% in el Hospital 1 (P<.001). No statistically significant differences were found in the frequency of use of the other measures such as BF/EMM, non-nutritious suckling or holding.
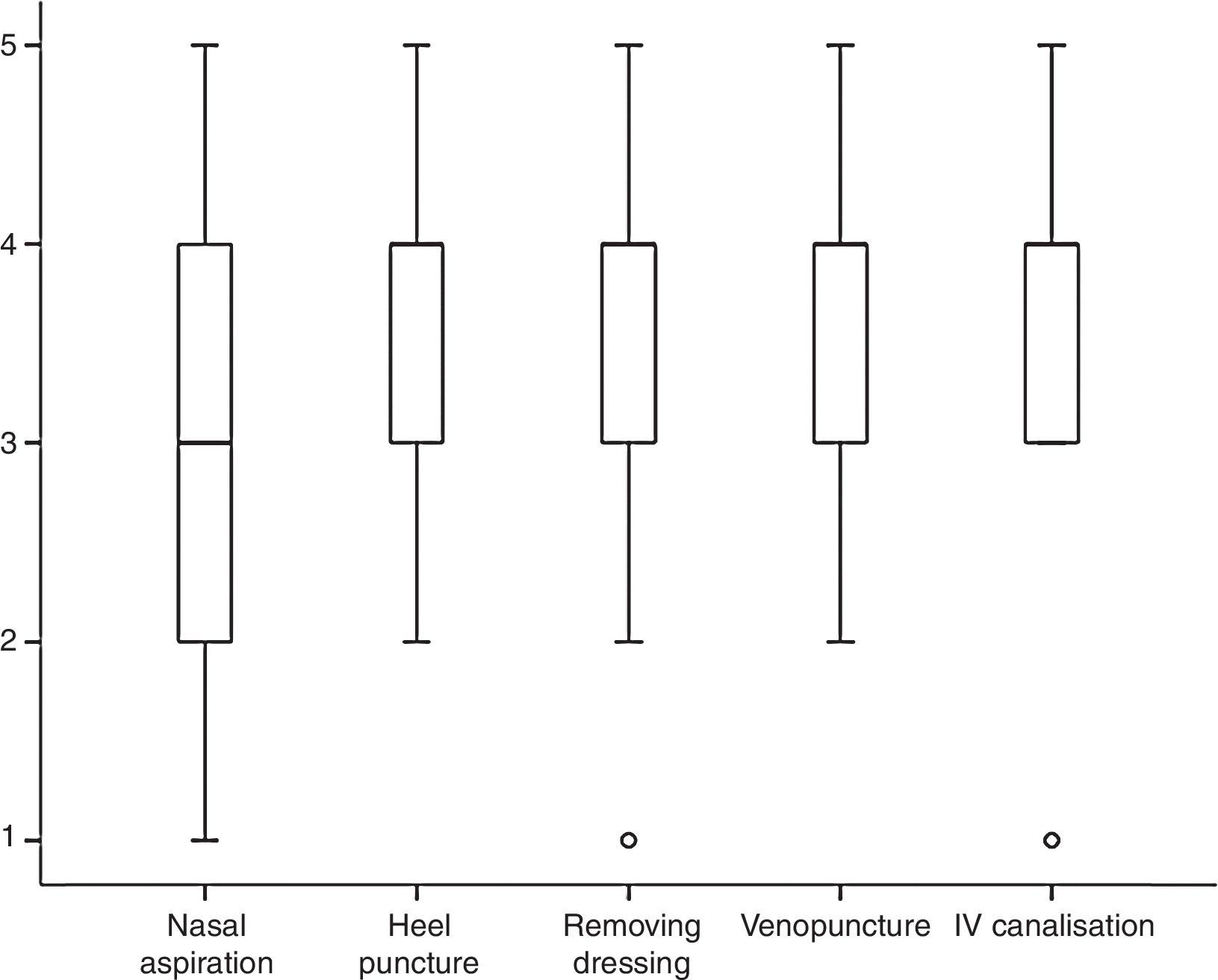
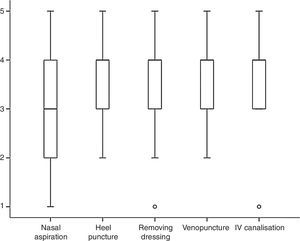
Fig. 2 shows the perception of the professionals surveyed about the intensity of the pain associated with five of the most common minor procedures in neonatal units.
The overall score awarded to pain management in their unit was 6.3±1.95 points. It was slightly higher in the ICNU (6.8±1.2 points) than it was in the NICU (6.08±2.18 points) (P=.04).
Staff qualification also differed between hospitals. The staff in Hospital 1 scored 5.85±1.97 points, while the staff in Hospital 2 scored 6.25±2.19 points; the highest score was obtained in Hospital 3, with 7.45±1.14 points (P<.001).
Significant differences were found in the overall qualification for pain management between those professionals who had received specific training in the previous 5 years (6.82±1.61 points) and those who had not received it (5.88±2.12 points) (P=.005). No significant differences were found between the overall score for pain management and years of experience or professional category.
DiscussionThis research study is the first one of nursing staff perceptions regarding neonatal pain management in Spain. It shows that pain management by nursing staff is still improving, due to the limited specific training in this field and the low implementation of validated pain evaluation scales. Nevertheless, it should be pointed out that the use of non-pharmacological means of pain relief during minor procedures has improved.
The percentage of nursing professionals trained specifically in the management of neonatal pain is low in our sample (47.9%), a percentage similar to the one found by Cong et al.20 Given this result, pain management may be considered to be a non-priority aspect in the on-going training plans for nursing personnel.
Differences are also found between hospitals in the same Autonomous Community; this also therefore depends on the strategies and aims of each neonatal department. However, pain management should be a universal strategy in all departments, given that a range of international institutions such as the American Academy of Paediatrics, the International Association for the Study of Pain, as well as national ones such as the Sociedad Española del Dolor consider pain relief to be an ethical obligation and a fundamental right of patients.13,21
It should be underlined that the professionals with the most experience are also the ones who have received the most specific training about pain in the previous 5 years. This relationship was not found in the study by Martín et al.22
In the case of premature infants—and more so in the case of very premature ones—manipulation should take place using two professionals. Due to unit organisation these will normally be a nurse and an ANCT.23 It is therefore important that both be trained in neonatal pain management, so that they will be able to supply optimum pain prevention, evaluation and management.
Approximately 44% of the sample said that they evaluate pain using a validated scale. This datum is similar to those obtained in the study by Cong et al.,20 where 49% of the Chinese sample used scales regularly in their unit. This percentage rises to 81.5% of the sample of nurses in the United States. The study by Ozawa and Yokoo18 in Japan found that 40% of nursing respondents used validated scales. Nevertheless, the study by Foster et al.19 in Australia found that only 11% of the units studied use scales, and it was in highly specialised neonatal and surgical units where they are most used.
However, when observational studies that audit clinical histories are reviewed, pain evaluation is even less frequent. The EUROPAIN24 study found that 31.8% of the neonatal infants studied had been evaluated for pain on a validated scale at least once in the month of the study; the data in Spain using the same methodology25 are lower than this, showing that only 16.7% of the children admitted to neonatal units had records of pain evaluation using a validated scale.
It should be pointed out that differences were found between the different hospitals studied in the use of validated scales. Hospital 3 stands out, as it has implemented complete electronic clinical histories and has the highest percentage of evaluations. The aforesaid tool gives frequent reminders for evaluation, and it also gives access to the said scales.
The scales used the most are the PIPP, CRIES and NIPS. This is a similar finding to those of Ozawa and Yokoo,18 where the PIPP was the most used, followed by the NIPS. However, the study by Avila-Alvarez et al.25 indicates that at a national level the most used are the NIPS (30%), the CRIES (25%) and the PIPP (10%). These differing results may be due to the nature of the neonatal units where the studies took place, as the PIPP scale is indicated for premature infants and CRIES is for infants after surgery. This therefore shows the gap between the number of validated scales and their infrequent use in clinical contexts.26
Respecting non-pharmacological measures, sucrose (77.9%) is used more frequently than EMM and/or breast feeding (76.9%). This is similar to the findings of other national publications, such as the one by López-Maestro et al.,16 which showed 75% regular use of sucrose compared to 15% EMM and/or breast feeding; the study by Foster et al.19 showed similar results for sucrose, although EMM and/or BF were used more often.
Significant differences were found in this study regarding the frequency with which sucrose is used, as was also the case for Losacco et al.27 They found that sucrose was often used in countries such as Sweden (83%) and Denmark (100%), in comparison with countries where it is used far more rarely, such as Belgium (5%), the Netherlands (10%), the United Kingdom (12%) or Spain (15%). These discrepancies may be explained by fact that sucrose is used less for minor procedures due to lack of knowledge about the effect of repeated doses in premature infants, disagreements about its mechanism of action and, definitively, the absence of sucrose administration procedures.28 It was also found that the volume of sucrose given is hardly ever recorded, giving rise to lack of knowledge about the total volume administered to patients. As the latest recommendations indicate, sucrose has to be identified as a medication, so that it must be prescribed and recorded.12
Respecting the perception of pain intensity during painful procedures in this study, intravenous canalisation was considered to be the most intense. This agrees with the studies by Jeong et al.29 and Andersen et al.30
The professionals consider heel puncture to be less painful than venepuncture, unlike the review by Cochrane.31
Finally, the general opinion of pain management in their units is considered to be appropriate. This is similar to findings in other studies,14,20 and the professionals who have received training award the highest scores here.
The limitations of this study are those which are intrinsic to its methodology. It has to be said that it is possible that the questionnaire was answered by the professionals who are the most interested in treating neonatal pain, and this may have distorted the results. Another limitation is that not all of the hospitals are equally represented in the sample.
ConclusionsThis is the first study of how nursing staff perceive neonatal pain management to be performed in Spain. It shows that pain management is still improving, with limited specific training and a low rate of validated pain scale implementation. Strong points are the improvement in the use of non-pharmacological measures for pain relief in minor procedures.
In the light of these results, training strategies should be designed together with improved care plans such as those using bundles. These would have the purpose of improving training in neonatal pain evaluation and management, including the whole multidisciplinary team in the said plans, with neonatal specialists and nursing staff.
Pain control has to be included as a universal objective for care in the strategic plans of neonatal departments. It is a complex problem, so that it has to be an essential value for the institution and not be subject to individual action by some professionals. Specific lines of pain control are also a priority concern for very premature infants, given that their responses to pain are less specific and they present more comorbidities and instability. In these patients the efficacy of pharmacological and non-pharmacological measures has been studied less.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank the nursing staff who took part in the study of neonatal departments in the Hospital Universitario Gregorio Marañón, Hospital Universitario Puerta de Hierro-Majadahonda and the Hospital Universitario 12 de Octubre. We would also like to thank the Nursing Research Support Unit of the Hospital Universitario Gregorio Marañón for their advice, and the Preventive Medicine and Quality Management Unit of the same hospital for supplying the data gathering tool.
Please cite this article as: Collados-Gómez L, Camacho-Vicente V, González-Villalba M, Sanz-Prades G, Bellón-Vaquerizo B. Percepción del personal de enfermería sobre el manejo del dolor en neonatos. Enferm Intensiva. 2018;29:41–47.