To estimate how many of the trauma patients admitted to ICU would be candidates for a secondary prevention program for trauma related to alcohol or drug use by brief motivational intervention and to define what factors prevent that intervention being performed.
MethodsAll 16–70year old trauma patients (n=242) admitted to ICU in 32 non-consecutive months (November 2011–March 2015) were included in the study, coinciding with the implementation of a screening and brief motivational intervention program for trauma patients related to substance consumption. The program includes screening for exposure to substances at admission. Sociodemographic and clinical variables were collected prospectively.
ResultsThe screening for substances was not performed in 38 (15.7%) of all admitted patients. Of the patients screened, 101 (49.5%) were negative. The variables that in greater proportion impeded intervention between screening positive patients were neurological damage due to the trauma with 23 patients (37.1%) and prior psychiatric disorder with 18 (29%). Both variables were associated with substance consumption: negatives 9.9% vs positive 22.3% (p=.001) and negatives 3% vs positive 17.5% (p=.016) respectively. The number of candidates for motivational intervention was 41, 16.9% of all admitted patients.
ConclusionsAlmost 2 out of 10 patients were potential candidates. The factors that in a greater proportion precluded the intervention were the same as those associated with consumption. Mortality in ICU was associated with non-compliance with the screening protocol.
Estimar cuántos de los pacientes ingresados en la UCI por un traumatismo serían candidatos a un programa de prevención secundaria por traumatismos relacionados con el consumo de alcohol y drogas mediante intervención motivacional breve y establecer qué factores impiden la realización de esta intervención.
MétodosSe incluyeron en el estudio todos los pacientes de entre 16 a 70años (n=242) ingresados en la UCI por lesiones traumáticas en 32meses no consecutivos (de noviembre de 2011 a marzo de 2015), coincidiendo con la implantación de un programa de cribado e intervención motivacional breve para traumatizados relacionados con el consumo de sustancias. El programa incluye el cribado de exposición a sustancias en el ingreso. Se recogieron prospectivamente variables sociodemográficas y clínicas.
ResultadosDel total de pacientes ingresados, a 38 (15,7%) no se les realizó la determinación a sustancias. Dieron resultado negativo 101 (49,5%) de los pacientes analizados. Las variables que en mayor proporción impedían la intervención entre los positivos fueron las secuelas neurológicas debidas al traumatismo (23 pacientes; 37,1%) y el trastorno psiquiátrico previo (18 pacientes; 29%). Ambas variables aparecieron asociadas al consumo: 9,9% negativos vs 22,3% positivos (p=0,001) y 3% negativos vs 17,5% positivos (p=0,016), respectivamente. El número de pacientes candidatos a intervención motivacional fue de 41, el 16,9% del total de ingresados.
ConclusionesCasi 2 de cada 10 pacientes fueron potenciales candidatos a la intervención. Los factores que en mayor proporción la impedían entre los positivos fueron los que aparecieron asociados al consumo. La mortalidad en la UCI se asoció con el incumplimiento del protocolo de cribado.
Choosing “an appropriate time for teaching”, or “teachable moment”, to take measures for health prevention and promotion, has proven to be an effective strategy. To this end, programs aimed at detecting alcohol and drugs in patients hospitalized for trauma, and the subsequent conduct of a brief motivational intervention during their hospital stay, are initiatives based on evidence that these actions result in a reduction or complete cessation of the consumption of such substances. However, there are doubts regarding the fact that this type of measures can be implemented successfully in intensive care settings, given the characteristics of the patients admitted to said units.
This paper analyzes situations that prevent the conduct of brief motivational interventions in trauma patients admitted to an intensive care unit in order to estimate how many of such patients would benefit from this technique, describing which are the factors that prevent the conduct of the intervention.
Implications of the studyThe conduct of secondary prevention nursing interventions in trauma patients entails an opportunity for professional development based on available evidence and within our competence framework. A greater understanding of the amount and characteristics of intensive care unit patients who could benefit from a screening program and brief motivational intervention should encourage the development of initiatives aimed at implementing this sort of programs, in collaboration with other healthcare professionals and hospital units, as well as the promotion of new research deepening the knowledge of the impact of these initiatives.
At times, an English term can be difficult to translate into Spanish, and this is the case with the expression “teachable moment”. This expression can be translated as “an appropriate time for teaching”, and is defined, in health sciences, as a situation or set of circumstances that leads an individual to modify their health behavior in a positive way.1 Taking advantage of the special receptivity to make behavioral changes that results from experiencing certain situations, has intuitively been accepted as an important focus for clinicians and researchers interested in healthcare promotion and education, therefore, the effectiveness of choosing an adequate moment to promote such changes hast been studied in multiple contexts and situations.2–13
The situation leading to such behavioral change can be a positive one used to adopt healthy behaviors, such as pregnancy.4,10 However, on other occasions, it is the individual's experiencing of adverse events related to their harmful health habits which gives us an opportunity to help our patients adopt effective measures to change their behavior in terms of their own healthcare. A clear example of this can be seen in patients who are hospitalized for respiratory diseases related to tobacco consumption,2 in those who have suffered a cardiac episode6,8 or those who have suffered trauma secondary to alcohol and/or drug abuse.14,15 In this sense, there is evidence that a patient's hospitalization implies a temporary interruption of harmful habits, which consequently generates “a window of opportunity”16 to adopt initiatives aimed at initiating change.
Along these lines, the Screening, Brief Intervention, and Referral to Treatment (SBIRT)17 program for the systematic screening of alcohol, drugs and psychotropic drugs in trauma patients, the brief (motivational) intervention and the referral to specific treatment in patients with more severe problems, have been recommended as part of an integrated approach based on public health evidence to address the issue of alcohol and drug abuse.18
A brief motivational intervention (BMI)19 consists of a semi-structured interview lasting approximately 30min, aimed at changing patients’ behaviors to promote healthier lifestyles. A BMI has proved to be effective and, therefore, its implementation is currently being studied for several conditions such as diabetes,20 obesity21 and tobacco consumption.22 However, its most widespread scope of application is in drug addictions.23
The combination of the use of a BMI added to the benefits of choosing the most appropriate moment during the patients’ hospital stay, could determine the success of SBIRT programs. However, there are still doubts regarding which type of hospitalizations should be considered as a teachable moment (admissions to the Emergency Department, to the Intensive Care Unit [ICU], or to a conventional hospital ward).
In our country, a pilot study for the implementation of an alcohol screening and intervention program in patients with traffic-related injuries carried out in an Emergency Department concluded that the difficulties to apply such type of programs in Emergency Departments were obvious.24 Furthermore, it seems obvious that the likelihood of success increases when these initiatives are implemented in normal hospitalization wards,25 where a greater number of “windows of opportunity” may be available. However, higher quality opportunities are more likely to be found in the ICU.12 In the ICU, the severity of the situation experienced by the patient puts the individual in an ideal position to start adopting the relevant measures for change, with the necessary help. Nevertheless, this severity and the sequelae related to such experience could prevent a sufficient number of patients from benefiting from a screening and motivational intervention program.
Based on the above, this study was approached with the following objectives in mind:
- -
To determine the percentage of patients admitted to an ICU due to trauma who are eligible for a systematic screening protocol for substance abuse and a BMI.
- -
To estimate the most prevalent factors of non-compliance of the screening protocol+BMI in trauma patients.
- -
To analyze differences between the sociodemographic and clinical characteristics of patients in which the protocol was not followed and those in which it was.
A prospective, analytical, observational study was carried out in the ICU of the University Hospital Complex of Granada.
SubjectsSubjects were selected thanks to a project aimed at implementing a program for the secondary prevention of traumas potentially associated with the consumption of alcohol, drugs and psychotropic drugs. The purpose of this protocol, which was approved by the hospital's Ethics Committee, is to systematically screen for the presence of such substances in patients aged 16–70years old who are hospitalized for trauma, so that patients with a positive result may receive a BMI and/or be referred for specialized care18 after obtaining their informed consent.
Patients admitted to the ICU were candidates, in the first place, for the screening protocol and, thereafter, for the BMI, whenever they met the following selection criteria:
Inclusion criteria of the screening program- -
Hospitalization due to trauma.
- -
Age 16–70years old.
- -
Death.
- -
Immediate transfer to another clinic.
- -
Neurological sequelae.
- -
Spinal cord injury.
- -
Previous psychiatric disorder.
Throughout the study period, the program remained active for a total of 32 non-consecutive months (due to discontinuities in funding sources): from November 2011 to October 2012, from June 2013 to November 2013 and from June 2014 to March 2015. Therefore, the eligible population for this study consisted of all patients admitted to the ICU for traumatic injuries during the periods in which the program was active.
Collection of data and variablesFactors preventing the implementation of the BMIFor the purpose of this study, we defined the factors preventing the implementation of the motivational intervention among all patients admitted to the unit:
- -
Non-compliance of the substance screening protocol.
- -
Negative result for substance consumption.
- -
BMI exclusion criteria among patients positive for substance abuse.
All samples were collected upon the patients’ admission to the ICU; our hospital's protocol specifies that care for severe trauma must be administered in the intensive care unit after stabilizing the patient in the Emergency Department, if necessary. Exposure to alcohol was determined by gas chromatography, considering blood alcohol levels equal to or greater than 0.3g/l as a positive result. The use of illicit drugs (cannabis, cocaine, amphetamines, methamphetamines, heroin) and psychoactive drugs (benzodiazepines, prescription opiates, barbiturates and tricyclic antidepressants) was detected with a urine fluorescence immunoassay (LifeSign StatusFirst®)26. In order to differentiate patients with positive results for benzodiazepines and opiates due to the administration of drugs by pre-hospital emergency services or in the emergency department from those who had consumed such substances prior to suffering the trauma, we reviewed the medical histories (hospital and pre-hospital) of all patients admitted, and we carried out interviews with the patients or their family members.
Other sociodemographic and clinical variables includedIn order to define the study population and the analysis of factors, the following data was collected prospectively during the patient's stay at the ICU: age, sex, injury mechanism (traffic accident, sports accident, assault, fall from the same level, falls from a height, blows-cuts and other mechanisms), severity of the trauma measured by the Injury Severity Score (ISS),27 length of stay at the ICU and mortality at the ICU.
Data analysisTo analyze those factors preventing the conduct of the BMI, we first compared the main demographic and clinical characteristics of patients who had undergone screening with those in which the substance screening protocol had been breached. To calculate the total number of patients candidate for a BMI, the number of patients who had not undergone screening, who were negative for substance abuse and who were positive for substance abuse and met BMI exclusion criteria, was subtracted from the total of patients admitted to the unit.
To determine which characteristics seemed to be related to the detection of the substance abuse and the existence of differences in the distribution of the exclusion criteria according to the negative or positive result to substance consumption, these variables were compared according to the exposure. Finally, demographic and clinical characteristics were compared among patients grouped according to whether or not they were candidates for BMI, in order to be able to determine variables associated with their availability for the intervention which could difficult it.
For the statistical analyses, after verifying the lack of normality in the distribution of quantitative variables with Shapiro–Wilk's test, the median and interquartile range [IQR] were used as measures of the central tendency and dispersion, using Mann–Whitney's tests to compare such variables. Pearson's chi-square test was used to examine the association between categorical variables. All analyses were carried out in the SPSS 20.0 software for Windows (SPSS, Chicago, IL), considering p-values <0.05 as significant.
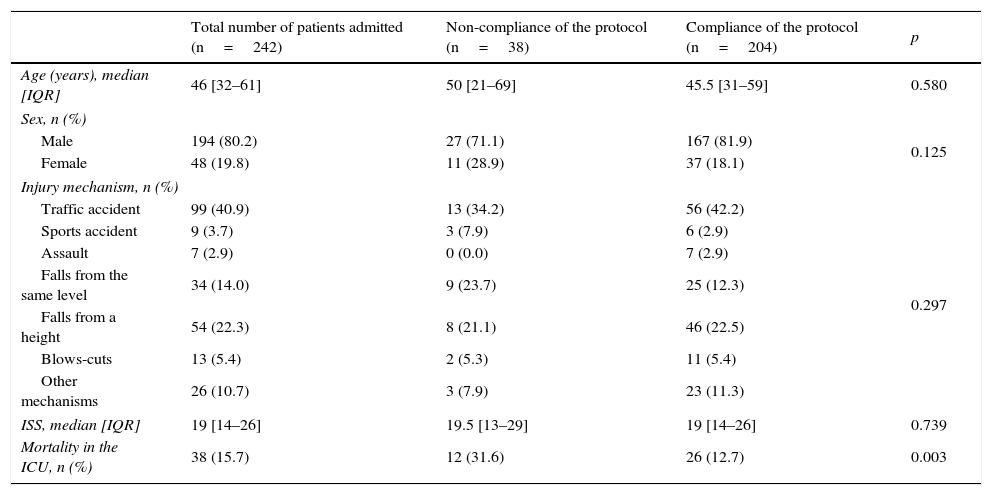
ResultsOf the total number of patients admitted to the ICU (n=242), 38 (15.7%) did not undergo screening tests for alcohol, drugs or psychotropic drugs upon admission due to the non-compliance of the protocol on behalf of the on-call team, hence, the final total number of patients analyzed for substance abuse was 204 (84.3%). In the comparison of distribution variables between non-analyzed and analyzed patients (Table 1), the mortality rate was found to be significantly lower in the second group (31.6% vs 12.7%; p<0.003).
Comparison of the main characteristics of patients admitted to the unit according to the compliance of the substance screening protocol.
| Total number of patients admitted (n=242) | Non-compliance of the protocol (n=38) | Compliance of the protocol (n=204) | p | |
|---|---|---|---|---|
| Age (years), median [IQR] | 46 [32–61] | 50 [21–69] | 45.5 [31–59] | 0.580 |
| Sex, n (%) | ||||
| Male | 194 (80.2) | 27 (71.1) | 167 (81.9) | 0.125 |
| Female | 48 (19.8) | 11 (28.9) | 37 (18.1) | |
| Injury mechanism, n (%) | ||||
| Traffic accident | 99 (40.9) | 13 (34.2) | 56 (42.2) | 0.297 |
| Sports accident | 9 (3.7) | 3 (7.9) | 6 (2.9) | |
| Assault | 7 (2.9) | 0 (0.0) | 7 (2.9) | |
| Falls from the same level | 34 (14.0) | 9 (23.7) | 25 (12.3) | |
| Falls from a height | 54 (22.3) | 8 (21.1) | 46 (22.5) | |
| Blows-cuts | 13 (5.4) | 2 (5.3) | 11 (5.4) | |
| Other mechanisms | 26 (10.7) | 3 (7.9) | 23 (11.3) | |
| ISS, median [IQR] | 19 [14–26] | 19.5 [13–29] | 19 [14–26] | 0.739 |
| Mortality in the ICU, n (%) | 38 (15.7) | 12 (31.6) | 26 (12.7) | 0.003 |
IQR: interquartile range; ISS: Injury Severity Score.
Out of all patients analyzed, 101 (49.5%) had a negative result for substance consumption. Among those with a positive result, the most frequently detected substance was alcohol in 76 patients (37.3% out of the analyzed total), followed by benzodiazepines in 31 (15.7%), cannabis in 25 (12.3%), cocaine in 12 (5.9%), tricyclic depressants in 6 (2.9%), opiates not administered at the hospital or by pre-hospital emergency services in 6 (2.9%), methadone in 4 (2%), barbiturates in 3 (1.5%) and amphetamines in 2 (1.0%).
Among those patients with a positive result for substance consumption, 62 met BMI exclusion criteria: 14 (22.6% of the total of positives excluded) passed away at the ICU, 3 (4.8%) were transferred to another clinic, 23 (37.1%) suffered neurological sequelae due to traumatic brain injury (TBI), 4 (6.4%) had spinal cord injury and 18 (29%) experienced some sort of diagnosed psychiatric disorder. Therefore, the final number of patients who were eligible for the BMI was 41, 16.9% of the total of patients aged 16–70years old who were admitted to the unit.
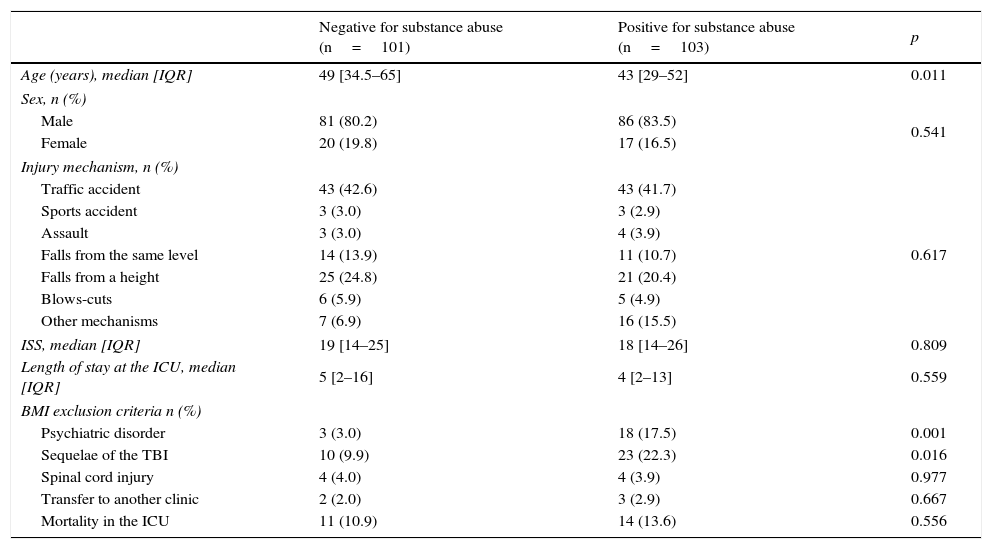
When comparing the demographic and clinical characteristics of the negative vs positive groups for substance consumption (Table 2), we found that the median age was 6years lower among patients who were positive for any of the analyzed drugs (p<0.011). Psychiatric disorders and neurological sequelae due to TBI were variables that appeared to be significantly associated with substance abuse, this also being the reason why a greater number of BMI candidates were excluded from the group of patients who were positive for substance consumption.
Comparison of the main patient characteristics according to the results of the substance screening protocol.
| Negative for substance abuse (n=101) | Positive for substance abuse (n=103) | p | |
|---|---|---|---|
| Age (years), median [IQR] | 49 [34.5–65] | 43 [29–52] | 0.011 |
| Sex, n (%) | |||
| Male | 81 (80.2) | 86 (83.5) | 0.541 |
| Female | 20 (19.8) | 17 (16.5) | |
| Injury mechanism, n (%) | |||
| Traffic accident | 43 (42.6) | 43 (41.7) | 0.617 |
| Sports accident | 3 (3.0) | 3 (2.9) | |
| Assault | 3 (3.0) | 4 (3.9) | |
| Falls from the same level | 14 (13.9) | 11 (10.7) | |
| Falls from a height | 25 (24.8) | 21 (20.4) | |
| Blows-cuts | 6 (5.9) | 5 (4.9) | |
| Other mechanisms | 7 (6.9) | 16 (15.5) | |
| ISS, median [IQR] | 19 [14–25] | 18 [14–26] | 0.809 |
| Length of stay at the ICU, median [IQR] | 5 [2–16] | 4 [2–13] | 0.559 |
| BMI exclusion criteria n (%) | |||
| Psychiatric disorder | 3 (3.0) | 18 (17.5) | 0.001 |
| Sequelae of the TBI | 10 (9.9) | 23 (22.3) | 0.016 |
| Spinal cord injury | 4 (4.0) | 4 (3.9) | 0.977 |
| Transfer to another clinic | 2 (2.0) | 3 (2.9) | 0.667 |
| Mortality in the ICU | 11 (10.9) | 14 (13.6) | 0.556 |
BMI: brief motivational intervention; ISS: Injury Severity Score; IQR: interquartile range; TBI: traumatic brain injury. Negatives: no substance detected; Positives: positive to any substance.
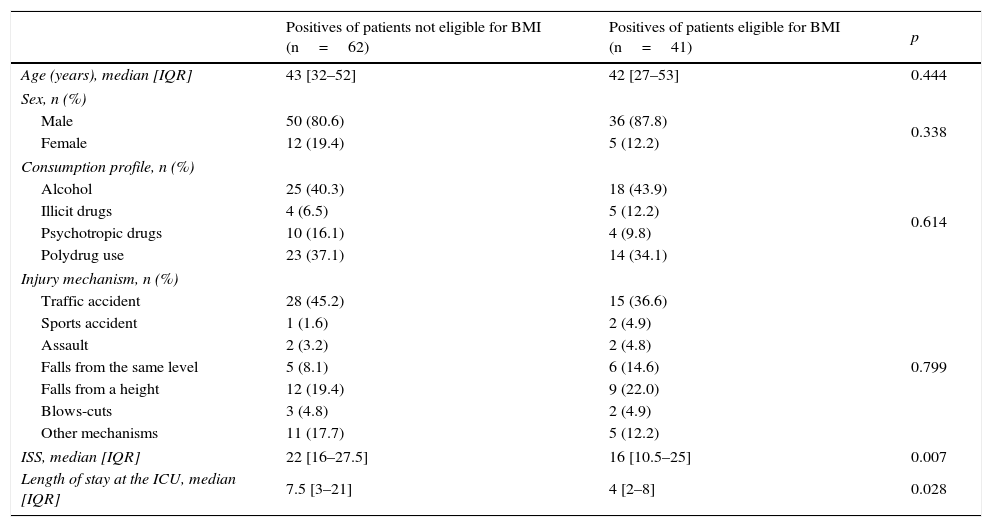
As for the comparison between the characteristics of eligible and non-eligible patients for BMI (Table 3), we detected a trauma severity 6 points lower in the ISS scale in eligible patients (p<0.007) and a median length of stay at the ICU 3.5days shorter than in the case of non-eligible patients (p<0.028). No differences were observed in the distribution of the injury mechanism, with traffic accidents being the most frequent type of injury in all groups. The substance abuse profile was mainly alcohol consumption (43.9%), followed by polydrug use (34.1%).
Comparison of the main patient characteristics according to whether they were eligible or not for the brief motivational intervention.
| Positives of patients not eligible for BMI (n=62) | Positives of patients eligible for BMI (n=41) | p | |
|---|---|---|---|
| Age (years), median [IQR] | 43 [32–52] | 42 [27–53] | 0.444 |
| Sex, n (%) | |||
| Male | 50 (80.6) | 36 (87.8) | 0.338 |
| Female | 12 (19.4) | 5 (12.2) | |
| Consumption profile, n (%) | |||
| Alcohol | 25 (40.3) | 18 (43.9) | 0.614 |
| Illicit drugs | 4 (6.5) | 5 (12.2) | |
| Psychotropic drugs | 10 (16.1) | 4 (9.8) | |
| Polydrug use | 23 (37.1) | 14 (34.1) | |
| Injury mechanism, n (%) | |||
| Traffic accident | 28 (45.2) | 15 (36.6) | 0.799 |
| Sports accident | 1 (1.6) | 2 (4.9) | |
| Assault | 2 (3.2) | 2 (4.8) | |
| Falls from the same level | 5 (8.1) | 6 (14.6) | |
| Falls from a height | 12 (19.4) | 9 (22.0) | |
| Blows-cuts | 3 (4.8) | 2 (4.9) | |
| Other mechanisms | 11 (17.7) | 5 (12.2) | |
| ISS, median [IQR] | 22 [16–27.5] | 16 [10.5–25] | 0.007 |
| Length of stay at the ICU, median [IQR] | 7.5 [3–21] | 4 [2–8] | 0.028 |
ISS: Injury Severity Score; IQR: interquartile range.
Alcohol: positives for alcohol alone; illicit drugs: positives for cannabis, cocaine, amphetamines, methamphetamines and/or heroin; polydrug use: positives for a combination of 2 or more substances of several of the above groups; psychotropic drugs: positives for benzodiazepines, prescribed opiates, barbiturates and/or tricyclic antidepressants.
The results of our study prove that 16.9% out of the total number of patients aged 16–70years old admitted to the ICU due to a trauma would be eligible for a systematic screening program for alcohol, drug and psychotropic drug consumption for the implementation of a BMI, taking advantage of the teachable moment that is the patients’ admission to such unit. The factors that most prevented this intervention among patients with a positive result for substance abuse coincided with those that were seen to be significantly linked to the consumption: neurological sequelae resulting from traumas and previous psychiatric disorders. Mortality in the ICU was also strongly linked to the non-compliance of the screening protocol.
The role of alcohol as one of the major risk factors for trauma is well-known,28 as well as that of drugs other than alcohol, such as cannabis, cocaine, amphetamines and other stimulants,29–33 and even of prescription or non-prescription psychotropic drugs, such as benzodiazepines or opioid derivatives.34,35 These investigations conclude that exposure to alcohol and/or other drugs is associated with a greater risk of trauma, regardless of the injury mechanism (traffic accident, falls, etc.). Moreover, the consumption of such substances and the recurrence of traumas is strongly associated.28,36
There is evidence that the BMI is a useful tool to combat this problem. A BMI could not only reduce substance consumption,23 but there is also data suggesting that it may reduce the recurrence of trauma by up to 50%,37 hence, the implementation of SBIRT programs in trauma clinics has proven to be a cost-effective measure,38 which has led countries such as the United States to adopt these programs as a mandatory requirement to accredit traumatology clinics as Level I centers.39
Although the usefulness of SBIRT-based programs in trauma patients seems obvious, their implementation in ICUs is questioned by some authors.12 These authors state that, given that the measures must be adopted based on evidence,40 the amount of evidence supporting the use of SBIRT-based programs in ICU patients is insufficient, including cost-effectiveness criteria, hence, efforts must be focused on identifying obstacles that difficult their implementation. In our study, we detected that variables associated with a positive result to substance consumption (psychiatric disorder and neurological sequelae) are, precisely, those which greatly prevent the implementation of BMI among patients with positive results for substance abuse (29 and 37.1%, respectively). The knowledge of these factors could facilitate the design of resource optimization strategies which, in turn, could tip the balance in favor of the implementation of screening programs and BMIs in ICUs.
Furthermore, the characteristics of patients eligible for the intervention draw the profile of a middle-aged male (42years old), consumer of alcohol or cocktails, who suffered a traffic accident and stayed at the intensive care unit for a median of 4days. The severity of the trauma is, logically, lower in comparison with that of the group of non-eligible patients, as the mortality is entirely concentrated in this second group. A lower severity may explain the fact that the median length of stay at the ICU is lower (4 vs 7.5 days) in the group of eligible patients, which reduces the “window of opportunity” for the BMI.
This study has the advantage of having been sponsored by a pioneering program in our country, in which a multidisciplinary research team, comprised by nurses, doctors and psychologists, has been working for more than 5years to implement a SBIRT-based program for patients with traumas related to substance abuse admitted to the ICU or to a conventional ward, with age (16–70 years old) being the only selection criteria, for the screening of alcohol, drugs and psychotropic drugs. This has enabled the conduct of these determinations in 84.3% of patients admitted to the ICU. However, the greater number of deaths among non-analyzed patients (31.6% vs 12.7%) indicates that patients who pass away are underrepresented in this estimate. This may be due to a greater non-compliance of the screening protocol of traumas more frequently associated with death, on behalf of the on-call team, especially in the case of those whose severity at admission could have delayed the compliance until, due to the patients’ death, the compliance no longer made sense.
Another important strong point of our study is the fact that, by reviewing the patients’ medical history (hospital and pre-hospital) and conducting interviews with the patients or their family members, we were able to differentiate patients whose positive results to benzodiazepines and opiates were a result of the medical care administered to treat the injury, from those who had consumed such substances prior to suffering the injury. This allowed us not to have to exclude all patients with a positive result for these groups of drugs, which are used so frequently in the management of trauma patients.
Despite the difficulties of the intervention in ICU patients, we believe that the available evidence supports the need to implement SBIRT-based programs that take advantage of the proven effectiveness of a BMI applied at the right time, through the sum of efforts at different levels (emergency services, ICU, hospitalization) and the coordination of the different healthcare professionals involved, with nurses playing a particularly important role in the implementation of BMIs, also endorsed by evidence.41–43
It is important to point out that, as in the case of previous experiences,24 the barriers that difficult the implementation of the SBIRT-based programs are not only the poor choice of the proper moment, information gaps or the training of the professionals involved, but also the lack of resources, either in the form of external collaboration or of the availability of time on the part of the nursing staff, which is decisive. The involvement of institutions, both governmental through the provision of resources, and scientific through the diffusion and recommendation of these programs, would entail a very valuable support mechanism that could increase the probability of success of initiatives based on scientific evidence.
Our study limitations included the fact that it was not possible to calculate an estimate of patients older than 70years and younger than 16years, as the hospital's screening protocol did not contemplate it and had a limited detection spectrum. The decision to study this age range in the screening program and the BMI implementation project was determined by the following factors:
- -
Trauma pathologies in age groups over 70years old differ greatly from the rest (predominantly falls related with frequently spontaneous hip fractures).44
- -
The prevalence of the consumption of alcohol and illicit drugs tends to be much lower in these extreme age ranges, and would consequently make screening programs implemented out of the established age range inefficient.17
- -
There is evidence that cognitive characteristics out of such age range can constitute an important limitation when implementing a motivational intervention of this type.45,46
Given the design of this study, it is not possible to determine how many candidates would have finally rejected the intervention, which constitutes a limitation for accurately estimating the number of patients who would have actually benefited from it, therefore, this data must be interpreted with caution.
ConclusionsAlmost 2 out of 10 patients admitted to the ICU due to trauma could benefit from a screening program and BMI, with the variables that most frequently prevent the conduct of the intervention among patients with positive results for substance consumption being neurological sequelae secondary to traumas and previous psychiatric disorders. Mortality in the ICU was seen to be associated with non-compliance of the screening protocol, with the percentage of deaths being significantly higher among patients in which the protocol was not implemented compared to those in which it was.
Knowledge of the barriers that prevent the conduct of the motivational intervention at the ICU can aid in adopting more optimized strategies to implement health promotion programs through BMIs in patients admitted to these units for trauma, aimed at encouraging the cessation or reduction of the consumption of harmful substances and/or the discontinuation of trauma risk behaviors.
Ethical disclosuresProtection of human and animal subjectsThe authors of this study declare that no human or animal experiments were carried out for this research.
Confidentiality of dataThe authors of this study declare that they followed the protocols established by their work center regarding the publication of patient data.
Right to privacy and informed consentThe authors of this study declare that no patient data was included in this paper.
FundingThis study was partially funded by the Directorate General of Traffic (Project: Technical assistance for the implementation of Motivational Interventions in accidents related to alcohol and drug use, Ref. 0100DGT22389) and by the Ministry of Health of the Junta de Andalucía (Project: Efficacy of Brief Motivational Interventions in the treatment of patients hospitalized due to traffic accidents related to alcohol and drug use, Ref. PI-0691-2013).
Conflict of interestThe authors of this study declare no conflict of interest.
We would like to thank the entire multidisciplinary team working at the intensive care unit of the former Traumatology Hospital of Granada, for their involvement and participation in the implementation of the screening protocol and brief motivational intervention.
Please cite this article as: Cordovilla-Guardia S, Vilar-López R, Lardelli-Claret P, Navas JF, Guerrero-López F, Fernández-Mondéjar E. Ingreso en cuidados intensivos por un traumatismo relacionado con el consumo de alcohol o drogas, un «momento propicio de enseñanza» para el inicio del cambio. Enferm Intensiva. 2017;28:4–12.
Second prize for the best oral communication presented at the XLII National Congress of the Spanish Society of Intensive Nursing and Coronary Units (SEEIUC), June 19–22, 2016, Valencia.