To determine the effectiveness of the ‘Creating Opportunities for Parent Empowerment’ (COPE) programme in reducing stress levels in mothers of preterm infants in the neonatal intensive care unit (NICU).
MethodsClinical trial performed in Colombia, including mothers of infants younger than 34 weeks of gestation, hospitalized, without a history of premature delivery. The mothers with psychiatric illnesses, language disorders, history of use of psychoactive substances and whose newborns had a congenital malformation were excluded. A group intervened with the COPE programme and a control group with the usual institutional management were formed. Block randomisation and masking was used for mothers and evaluators. The parental stress scale was applied: NICU; Shapiro–Wilk normality test, Wilcoxon test and covariance analysis (ANCOVA) with a significance level of p<.05, 95% CI.
Results66 mothers were enrolled. The two groups were similar in their demographic characteristics and in the initial stress level score. The control group increased the final stress score in two categories and the intervention group decreased final values in all categories. The initial and final scores of the overall general stress level showed a significant decrease (p<.01), but when comparing with the ANCOVA analysis there was no significant difference (p=.4).
ConclusionsThe COPE programme reduces the level of maternal stress, strengthening aspects during hospitalisation, such as: emotional support, strengthening their role as caregivers and interaction with their babies and the development of a friendly environment in the NICU.
Determinar la eficacia del programa «Creating Opportunities for Parent Empowerment» (COPE) en la disminución del nivel de estrés en madres de prematuros en la unidad de cuidado intensivo neonatal (UCIN).
MétodosEnsayo clínico realizado en Colombia en el cual se incluyeron las madres de recién nacidos menores de 34 semanas de gestación, hospitalizados, sin antecedentes de hijos prematuros. Se excluyeron las madres con enfermedades psiquiátricas, trastornos del lenguaje, antecedentes de consumo de sustancias psicoactivas y cuyo recién nacido tuviera malformación congénita. Grupo intervención con el programa COPE y grupo control con el manejo usual institucional. Asignación aleatoria por bloques y enmascaramiento para madres y evaluadores. Se aplicó la Escala de Estrés Parental: UCIN. Se realizó la prueba de normalidad Shapiro Wilk, el test de Wilcoxon y análisis de covarianza (ANCOVA), con un nivel de significación de p<0,05 e IC del 95%.
ResultadosParticiparon 66 madres. Los dos grupos fueron similares en sus características demográficas y en la puntuación del nivel de estrés inicial. El grupo control aumentó la puntuación final de estrés en dos categorías y el grupo intervención disminuyó valores finales en todas las categorías. La puntuación inicial y final del nivel de estrés general total mostró disminución estadísticamente significativa (p<0,01), pero al realizar la comparación mediante el análisis ANCOVA no hubo diferencia significativa (p=0,4).
ConclusionesEl programa COPE disminuye el nivel de estrés materno, fortaleciendo aspectos durante la hospitalización como son: el apoyo emocional, el fortalecimiento de su rol como cuidadoras, la interacción con sus bebés y el desarrollo de un ambiente amigable en la UCIN.
We know from several studies that mothers of hospitalised preterm infants suffer high levels of stress, and that if this stress is not appropriately managed it can lead to mental disorders, principally anxiety and maternal depression, which affects the development of their children.
What does the paper contribute?This study offers results on the efficacy of an educational programme to reduce stress levels in premature mothers, bearing in mind emotional support, strengthening their carer role and their interaction with their babies.
Implications of the studyFor clinical practice, it is essential that healthcare personnel in neonatal intensive care units intervene in reducing the stress levels caused by hospitalisation, which has a negative effect on the mother's mental health, and consequently on the wellbeing of the preterm infant.
Through teaching, as part of their academic programmes, student nurses need to learn about these types of interventions to reduce stress levels, and should be able to use them during their training.
Through management, programmes that reduce the parental stress of preterm infants in Spanish-speaking countries should be implemented. These have been shown to reduce days of hospital stay, and consequently reduce costs.
In research, studies must continue to be undertaken that demonstrate the efficacy of interventions in situations of high levels of stress, for mothers of twin births, and of infants with congenital malformations, for example.
We know more about the causes of premature births, and great advances have been made in prenatal care, but this has not been sufficient to reduce the number of premature births. On a global level, the incidence of premature births is 11%,1,2 and 20.12%3 in Colombia. This impacts the health of the baby as well as the family and social dynamics, and the newborn infant usually needs to be hospitalised.
This is a traumatic experience for mothers, who often experience feelings of guilt, failure, and loss of a longed for healthy baby. They also have to cope with the physical and emotional separation from their baby after delivery, which can affect the creation of a secure attachment bond.4
Feelings of powerlessness, loss of control, isolation and vulnerability aggravate the emotional trauma of mothers who are fearful and uncertain about the hospitalisation of their newborn baby.5 Added to this is the frustration of not being able to care for their baby, knowing that he/she is unwell, and that he/she must undergo various medical procedures.6
Furthermore, studies show that mothers with high levels of stress are more likely to suffer symptoms of depression. However, a sense of receiving support from healthcare professionals is a protective factor.7
Therefore, mothers of a hospitalised preterm newborn infant (PTNI) offer a good opportunity to perform interventions to reduce the stress associated with this experience, strengthen their parenting skills, increase their confidence in their own resources, and to change perceptions of themselves and their baby that might interfere with appropriate bonding. This, in turn can foster a safe environment for the newborn infant.8
The literature describes interventions to improve these outcomes seeking to reduce parental stress levels, hospital stay and costs.9 COPE (Creating Opportunities for Parent Empowerment)10–12is one of these interventions, and has had a major positive impact on the mental health of both parents and their children and on the development of the PTNI.
The aim of this study was to determine the efficacy of the COPE programme in reducing stress levels in premature mothers in the neonatal intensive care unit (NICU).
MethodsA randomised clinical trial (RCT), parallel and single-blind, performed in Bucaramanga (Colombia), comprising a sample of 66 mothers of PTNI hospitalised in three of the city's health institutions. The sample size was calculated to compare the means of the two groups, with a p value of 5% (p=.05), considering a power of 80%, an estimated loss of 10% of participants, and a delta of .6.
Preterm infants of a gestational age of 34 weeks or less can be hospitalised for longer than a week, and therefore mothers of PTNI of 34 weeks’ gestation or less, mothers for whom this was the first experience of having a hospitalised preterm infant, and mothers with a single foetus were included in the study. Mothers with psychiatric diseases, language disorders, a history of psychoactive substance consumption, and mothers whose newborn had a congenital malformation were excluded from the study. No changes were made to the eligibility criteria after the study had started.
A block randomisation was performed. A separate randomisation was undertaken for each institution. The block allocation was performed creating a sequence of random numbers in STATCALC, Epi Info™ 6.02.
A trained nurse in each institution monitored the admission of the preterm infants to the NICU, checked the inclusion–exclusion criteria, and gave the informed consent and/or assent form. Once the mother had agreed to take part, she signed the form, the nurse applied the parental stress scale (initial measurement), and then took an identification code from a sealed envelope, and immediately called the general study coordinator who made the allocation to either the control or intervened group, according to the block randomisation.
Twenty-two randomisations were made in each of the three institutions. The mothers were not told which group they had been allocated.
In the intervention group, the trained nurse in each institution applied the first two phases of the COPE programme. This programme comprises four phases that are implemented from the first days after delivery until 2 weeks after discharge from the NICU, with recommendations for the baby's corrected age of 9 months.
The phases of the COPE programme are as follows: the first phase is from the second to the fourth day after admission to the NICU, and contains information on the NICU and the features of the PTNI. The second phase is from the fourth to the eighth day, during which time the mother is encouraged to become involved in the care of the PTNI. The third phase is one week before discharge from the NICU, in which the mother is prepared to go home with her baby, and finally the fourth phase comprises follow-up at home at 2 weeks after discharge from the NICU, where the mother is offered support for the baby to adapt to life at home.
The COPE programme has an audio CD with educational information for each of the phases and a book with activities to help the mothers to apply this information. This material has been translated from English to Spanish, and this is the first time it has been used in Colombia.
The control group was managed as usual, with information on the services of the institution, the features of the neonatal unit and general information on newborns.
For both the control group and the intervention group, the activity was undertaken in a different place to the NICU, and at a time agreed with the mother that did not interfere with her visiting times to her hospitalised child.
On the sixth admission day (which in the intervention group was the day following the second COPE phase), another trained nurse applied the same parental stress scale to the study participant (final measurement), unaware of which group the participant belonged to.
The Parental Stressor Scale (Neonatal Intensive Care Unit [PSS:NICU]) was used to measure the stress levels. This tool measures and assesses the stress associated with parents’ stay in NICU and comprises two parts. The first part assesses four categories: light and sounds, behaviour of the newborn infant, staff behaviours and relationship with the newborn infant. The second part assesses the general level of stress of parents of a child in the NICU. The scores are measured with a Likert-type scale from 1 to 5, 5 being the maximum level of stress experienced. The reliability coefficient of this instrument obtained a Cronbach's alpha of .89.13 The data was entered in Epidata 3.1 independently by two research assistants who recorded the data using codes and generated two databases; they did not know who belonged to the control or the intervention groups. These two databases were appropriately validated and adjusted.
Statistical analysisStata: Release 12 (StataCorp) was used for the statistical analysis. Normal distribution of the variables related to the stress scale dimensions was checked using the Shapiro–Wilk test. The initial and final scores of the stress scale were compared using the non-parametric test (Wilcoxon test). Finally, covariance analysis (ANCOVA) was performed for the final score of the stress test.
Ethical considerationsThe directives of Resolution 8430, 1993 of the Colombian Ministry of Health were followed, which set the standards for health research. The international ethical guidelines were followed for research on human beings of the Declaration of Helsinki and The Council for International Organizations of Medical Sciences (CIOMS). Informed consent was requested, and in the case of underage mothers, informed assent was signed, and the verbal and written consent of their legal representative obtained. The researchers were certified in best practice for research on human beings. This research study was approved by the Scientific Research Ethics Committee in accordance with protocol number 03, 2013, of 26 July, 2013.
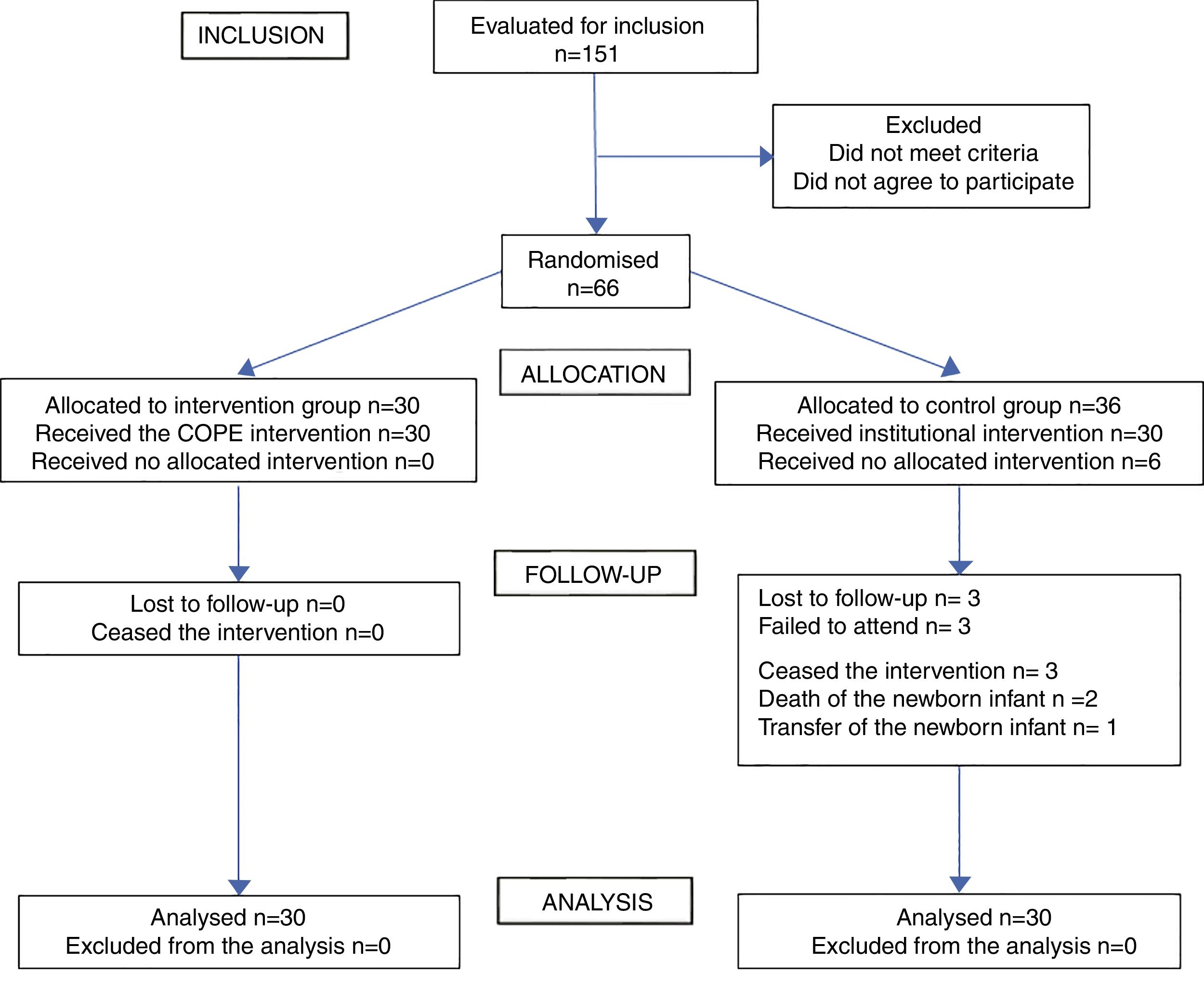
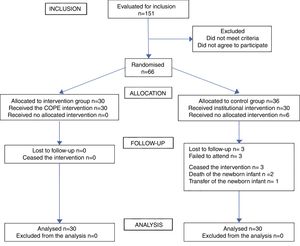
ResultsOne hundred and fifty-one mothers of PTNI were assessed for eligibility during the period that the sample was collected, of whom 85 were excluded (82 did not meet the inclusion criteria and 3 did not agree to participate), and 66 were included in the study. After the allocation of 30 mothers to the intervention group and 36 to the control group, 3 mothers stopped attending and 3 mothers ceased their participation (2 due to the death of the newborn and the other because she was transferred to a different health institution). There were no losses in the intervention group or subsequent exclusions. Finally, 30 mothers participated in each of the groups, who were studied for the primary result (Fig. 1).
The sample was gathered between 5 March and 8 September 2014. All the participants in each group were included in each analysis and this was undertaken according to the original allocation groups.
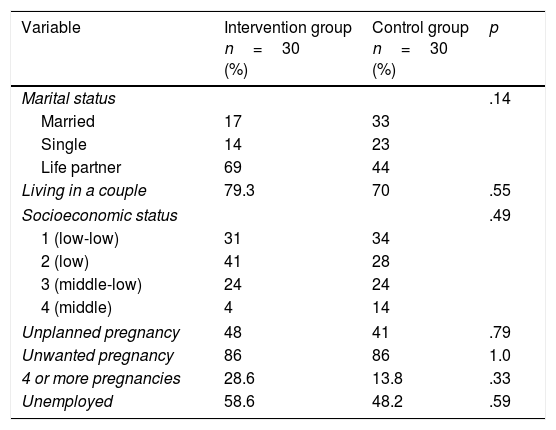
Sociodemographic featuresThe baseline sociodemographic features were similar in terms of marital status, living with a partner and economic status. The ages of the fathers and mothers did not did not follow Gaussian distribution (p<.05), therefore the non-parametric Mann–Whitney test ((Wilcoxon rank sum test) was used. The maternal age was 23±1.21 years in the intervention group, and 22±1.22 years in the control group (p=.61). The paternal age was 26±1.62 years in the intervention group, and 24±1.52 years in the control group (p=−56) (Table 1).
Comparison of the sociodemographic features of the participating mothers between the intervention group and the control group.
| Variable | Intervention group n=30 (%) | Control group n=30 (%) | p |
|---|---|---|---|
| Marital status | .14 | ||
| Married | 17 | 33 | |
| Single | 14 | 23 | |
| Life partner | 69 | 44 | |
| Living in a couple | 79.3 | 70 | .55 |
| Socioeconomic status | .49 | ||
| 1 (low-low) | 31 | 34 | |
| 2 (low) | 41 | 28 | |
| 3 (middle-low) | 24 | 24 | |
| 4 (middle) | 4 | 14 | |
| Unplanned pregnancy | 48 | 41 | .79 |
| Unwanted pregnancy | 86 | 86 | 1.0 |
| 4 or more pregnancies | 28.6 | 13.8 | .33 |
| Unemployed | 58.6 | 48.2 | .59 |
There were 7 mothers under the age of 18 years, but because they were so few they were not studied separately. The adult and adolescent participants were similar in terms of sociodemographic features and the newborn infant.
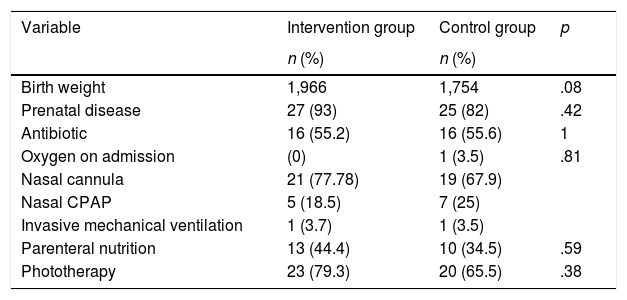
Features of the preterm newborn infantsThe newborn infants in the intervention group and those in the control group were similar in terms of morbidity and treatment received. The gestational age, the Apgar score and hospital stay did not follow Gaussian distribution (p<.05), and the non-parametric Mann–Whitney test was used (Wilcoxon rank sum test) to compare them. The intervention group were of 33±.32 weeks’ gestation and the control group 33±.42 weeks (p=.49). The Apgar score was 9±.84 and 9±1.59, respectively (p=.27). The intervention group had a shorter hospital stay (9 days) compared with the control group (11 days), but with no statistical significance (p=.55) (Table 2).
Features of the preterm newborn infant.
| Variable | Intervention group | Control group | p |
|---|---|---|---|
| n (%) | n (%) | ||
| Birth weight | 1,966 | 1,754 | .08 |
| Prenatal disease | 27 (93) | 25 (82) | .42 |
| Antibiotic | 16 (55.2) | 16 (55.6) | 1 |
| Oxygen on admission | (0) | 1 (3.5) | .81 |
| Nasal cannula | 21 (77.78) | 19 (67.9) | |
| Nasal CPAP | 5 (18.5) | 7 (25) | |
| Invasive mechanical ventilation | 1 (3.7) | 1 (3.5) | |
| Parenteral nutrition | 13 (44.4) | 10 (34.5) | .59 |
| Phototherapy | 23 (79.3) | 20 (65.5) | .38 |
The p values are based on the Fisher exact test.
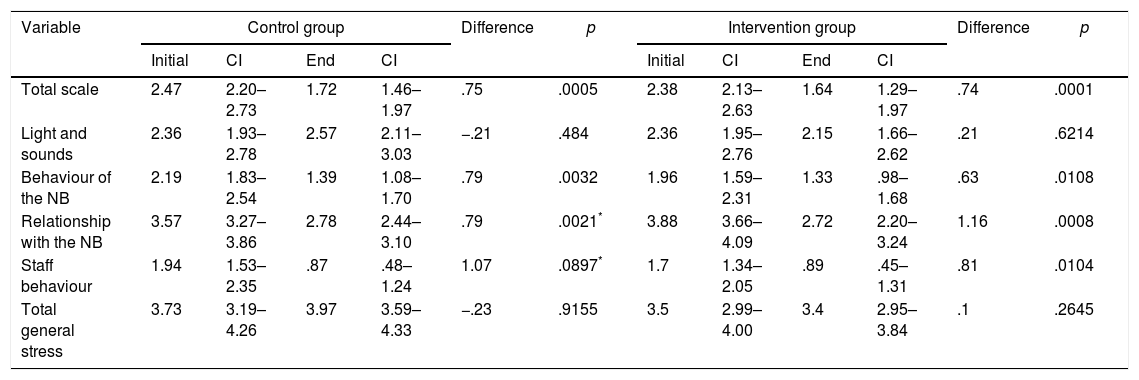
The initial stress assessment score in the control and intervention group in the different categories showed no significant statistical difference.
The scores of two of the four categories of the stress scale (relationship with the newborn infant and staff behaviour) did not behave normally (p<.05). Therefore, the non-parametric Wilcoxon test was used to analyse the initial values.
An increased final stress score was observed in the light and sounds category in the control group, while in the intervention group there was a reduction in the end values of all the categories. In terms of general stress, there was an increase in the end score of the control group and a slight reduction in the intervention group. We observed a statistically significant difference (p<.01) when we analysed the score obtained from the initial and final measurements of total general stress of the participating mothers. But when we made the comparison by group (control and intervention) controlling by the initial stress values using the ANCOVA analysis, we found no statistically significant difference (p=.4) (Table 3).
Average stress scale scores.
| Variable | Control group | Difference | p | Intervention group | Difference | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Initial | CI | End | CI | Initial | CI | End | CI | |||||
| Total scale | 2.47 | 2.20–2.73 | 1.72 | 1.46–1.97 | .75 | .0005 | 2.38 | 2.13–2.63 | 1.64 | 1.29–1.97 | .74 | .0001 |
| Light and sounds | 2.36 | 1.93–2.78 | 2.57 | 2.11–3.03 | −.21 | .484 | 2.36 | 1.95–2.76 | 2.15 | 1.66–2.62 | .21 | .6214 |
| Behaviour of the NB | 2.19 | 1.83–2.54 | 1.39 | 1.08–1.70 | .79 | .0032 | 1.96 | 1.59–2.31 | 1.33 | .98–1.68 | .63 | .0108 |
| Relationship with the NB | 3.57 | 3.27–3.86 | 2.78 | 2.44–3.10 | .79 | .0021* | 3.88 | 3.66–4.09 | 2.72 | 2.20–3.24 | 1.16 | .0008 |
| Staff behaviour | 1.94 | 1.53–2.35 | .87 | .48–1.24 | 1.07 | .0897* | 1.7 | 1.34–2.05 | .89 | .45–1.31 | .81 | .0104 |
| Total general stress | 3.73 | 3.19–4.26 | 3.97 | 3.59–4.33 | −.23 | .9155 | 3.5 | 2.99–4.00 | 3.4 | 2.95–3.84 | .1 | .2645 |
The results of this study, like those mentioned from other countries,10–12 showed a positive effect of the COPE programme in strengthening the role of the mother in the care of the PTNI in the NICU, which helps to reduce maternal stress levels. This RCT confirmed that this programme can be used in a population with different economic and cultural conditions.
There was no statistically significance difference in terms of the initial stress score in the four categories, but the general stress end score measured in the second part increased in the control group. This might indicate that routine activities in the NICU have a negative effect in themselves.
Despite the fact that the intervention and the assessment were undertaken over a short time, the changes observed, although not statistically significant, were important from a clinical perspective.
A short term effect was sought and therefore the final measurement was taken on the sixth day, showing changes that were small but valid from the point of view of the mothers’ mental health.
In Gertner's study (2010),14 where a short early intervention was applied, the subscale referring to the relationship of the mother with her newborn obtained a higher level of stress on initial measurement in both the control and the intervention group; unlike the results of this study, where the COPE intervention achieved a favourable result in the mothers of the intervention group, similar to the line of study by Ruiz et al.15
Melnyk et al.12 observed in their study that the mothers in the experimental group had less stress in the NICU, and interacted better with their children. They showed strong confidence in their ability to understand the behaviour of their babies, and in their knowledge about how to relate with him/her, and what sort of behaviours to expect during hospitalisation, as was expressed by the mothers in this study.
Another study undertaken by Ruiz et al.,15 that implemented an interdisciplinary programme (neonatologist, psychologist, physical therapist and nurse), managed to reduce stress levels in mothers of PTNI, attributing the effectiveness of the intervention to the emotional support provided to the mothers, and the guidance offered on interaction and stimulation to suit the needs of the PTNI. This was also evident in this study, and mentioned by the participating mothers.
Our findings are valid and suggest the possibility of effective intervention on parental stress levels associated with the experience in the NICU. It is important to highlight that the content of the interventions undertaken is similar and is closely related to the sources of stress in the NICU that are identified in the neonatal literature.16–18 This is largely because the intervention models stress the importance of emotional support to mothers, of their inclusion in the care of the newborn infant, of creating a more welcoming environment in the NICU, of fluid communication with staff, of providing knowledge about the behaviour of the preterm baby, and in activating social networks.9
Furthermore, the studies we reviewed coincide in that the treatments where parents take on a more active role tend to be more effective.10–12 Similarly, the interventions that take a short-term approach (intervening only during the period of hospitalisation, for example) tend to be less effective than those that follow up at home, although they involve greater costs. In relation to the latter, training of healthcare staff and the time they invest in the intervention do not always come at a high cost, because it is possible to obtain beneficial results using economical means, such as providing educational material and showing mothers how to use it.10–12 In turn, working with populations of a low socioeconomic level can present greater difficulties, due to a lack of resources, cultural differences, transport difficulties, and so on; however positive results are possible. Efforts made here are of great benefit, because the children from these families are at greater risk of developmental difficulties compared to babies from a higher economic level.12,15–18
Hospital stay in this study reduced as in other studies,10,11 which is of great benefit to mothers, healthcare staff and hospital administrators. A reduction in hospital stay is of great value because it implies, from a physiological perspective, a reduced risk of nosocomial infection and other complications. From a psychological perspective, it facilitates and strengthens bonding. Furthermore from an administrative perspective, it implies a significant reduction in costs, because currently a day's hospitalisation costs approximately 173USD, and in this case the hospital stay of the COPE intervention group reduced by 2 days, which is equivalent to 346USD per PTNI. In total, the institutions that participated in this study saved 10380USD from the 30 PTNI who were able to leave before the control group, which is a gain for the health system. Likewise, in the study by Melnyk and Feinstein,10 the experimental group showed a shorter hospital stay (3.9 days less), with the consequent reduction in costs.
It is important to highlight that, although there are common features in all the approaches that contribute towards their effectiveness, the literature emphasises the importance of tailoring interventions to the features of babies and their parents, their learning style and their coping strategies.12,15–18 To remain consistent, in this study the intervention was performed on the mother in the first week, when she has the highest stress levels,19 and intervention at this time might help her to cope better at the end of the hospital stay and on transition from hospital to home.20 In other words, this study shows that despite only having applied the first two phases of the COPE programme, it helped in the relationship between the mother and child.
A limitation of this study was not having included the fathers, since, from the design of the research study, the participating health centres showed that they did not attend the visits to their children during hospitalisation.
ConclusionsAgain we confirm that mothers have higher stress levels associated with hospitalisation, separation from the preterm newborn infant, and concern for their welfare. Similarly, the efficacy was observed of applying the first and second phases of the COPE programme in reducing stress levels of mothers of PTNI of less than 34 weeks’ gestation. The educational COPE programme covers various aspects during hospitalisation, such as emotional support, strengthening the mother's role as a caregiver, their interaction with their babies and their development in a friendly NICU, both in terms of the infrastructure and the relationship with healthcare personnel. Therefore it is important to implement this type of intervention in NICU to involve mothers in the daily care of the preterm infants, thus reducing the associated stress, and their feeling unable to perform their maternal roles.
Further research studies are needed that include the third and fourth phase of the COPE programme, preterm infants older than 34 weeks, different parent populations, and different times of stress measurement in the Latin-American context.
FundingThis article is the product of research project code 5697, funded by the Vicerrectoría de Investigación y Extensión de la Universidad Industrial de Santander, Bucaramanga, Colombia. The project received no external donations, all the material used was purchased by the University, and copyright was respected.
Conflict of interestsThe authors have no conflict of interests to declare.
The participants did not wish to be mentioned for reasons of confidentiality.
Please cite this article as: Villamizar-Carvajal B, Vargas-Porras C, García-Corzo JR. Disminución del nivel de estrés en madres de prematuros en la unidad de cuidados intensivos. Enferm Intensiva. 2018;29:113–120.