The monitoring system based on standards of quality allows clinicians to evaluate and improve the patient's care. According to the quality indicators recommended by Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias, and due to the importance of prone position (PP) as a treatment in patients with acute respiratory distress syndrome, it is fundamental to keep accurate record of serious adverse events occurring during the prone position procedure and its posterior analysis.
ObjectivesTo establish fulfilment of the Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias standards of quality according to the register of serious complications.
To identify the incidence of serious complications registered as well as to identify possible factors related to these complications.
MethodRetrospective, cross-sectional descriptive study, polyvalent ICU (16 beds).
Study populationPatients with acute respiratory distress syndrome treated with PP (January 2012–December 2013).
Study variablesPP recording, accidental extubation, removal of catheters, decubitus ulcers (DU), ETT obstruction, urgency of the procedure, hours in PP, nutritional intake, type of feeding tube, food regurgitation/retention and use of prokinetics/muscle relaxant.
ResultsThe study sample comprised 38 cases, with an adequate record of complications in 92.1% of the cases.
DU were the only serious complication recorded, with a 25.7% incidence.
Possible factors related to DU: more hours in PP in patients developing DU (p=0.067). Less incidence of DU in well-nourished patients (p=0.577).
82.9% of patients were not appropriately nourished.
ConclusionsThe percentage of records duly completed is very high. The presence of DU (grade 1–2 mostly) is to be noted. There is no statistical significance, although a trend is obsersed, between DU and hours in PP.
El sistema de monitorización mediante indicadores de calidad permite evaluar y mejorar la calidad asistencial. Atendiendo a los indicadores recomendados por la Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias y dada la importancia del tratamiento postural en decúbito prono (DP) de pacientes con síndrome de distrés respiratorio agudo, resulta crucial el registro de las complicaciones que puedan producirse durante el procedimiento y su posterior análisis.
ObjetivosDeterminar el grado de cumplimiento del estándar de calidad recomendado por la Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias en relación con el registro de complicaciones graves.
Identificar la incidencia de complicaciones graves registradas y posibles factores relacionados.
MétodoEstudio descriptivo retrospectivo transversal, UCI polivalente (16 camas).
PoblaciónPacientes con síndrome de distrés respiratorio agudo tratados con DP (enero 2012-diciembre 2013).
VariablesRegistros DP, extubaciones accidentales, retiradas de catéteres, úlceras por presión (UPP), obstrucción del tubo endotraqueal, urgencia procedimiento, horas DP, aporte nutricional, tipo de sonda alimentaria, regurgitación, retención alimentaria, uso de procinéticos y/o relajantes musculares.
ResultadosLa muestra del estudio fue de 38 casos habiéndose encontrado un registro adecuado de las complicaciones en un 92,1% de los casos.
La única complicación grave registrada fueron las UPP con una incidencia del 25,7%.
Posibles factores relacionados con UPP: horas en DP superior en pacientes que desarrollaron UPP (p=0,067); menor incidencia de UPP cuando el aporte nutricional ha sido adecuado (p=0,577).
El 82,9% de los pacientes pronados no recibieron aporte nutricional adecuado.
ConclusionesEl porcentaje de registros adecuadamente cumplimentados es muy elevado.
Destaca la aparición de UPP (grado 1-2 mayoritariamente).
No hay significación estadística, aunque sí tendencia, entre UPP y horas DP.
The PP has been used for years as a coadjuvant in treatment with protective mechanical ventilation in patients with Acute Respiratory Distress syndrome. This postural treatment gives rise to an improvement in oxygenation that is described in many studies, and recently several authors have even shown there is an improvement in mortality in patients with severe acute respiratory syndrome treated at an early stage with the PP. Few studies exist of the PP, how to implement it and nursing care, which based on scientific evidence determine the causes of the serious complications that arise with the procedure and make it possible to suggest solutions.
Care applicability: identifying the percentage of severe complications that arise during the procedure and possible factors associated with them will make it possible to improve the quality of care by applying preventive measures.
Research applicability: this requires the design of broader multi-hospital studies which confirm the results obtains and help to define the factors associated with the severe complications described with greater precision. This may open the door to a highly interesting line of research to analyse, in depth, the determining factors that interfere with appropriate compliance of nursing record-keeping.
Implications of the study?In connection with the implications for clinical practice, knowledge of the degree of compliance with records of severe complications during the procedure and the incidence of the same means that nurses must be made aware of the need to find solution that reduce their appearance and favour better compliance with the need to keep records. This study shows the importance of the quality of clinical records and the need for nurses to be aware of this, as this permits the continuity of information and affects patient care, directly influencing their safety.
This also have implications in terms of training, with specific interventions (educational sessions on the importance of rigorous compliance with record-keeping, awareness of the procedure, its complications and how to prevent them).
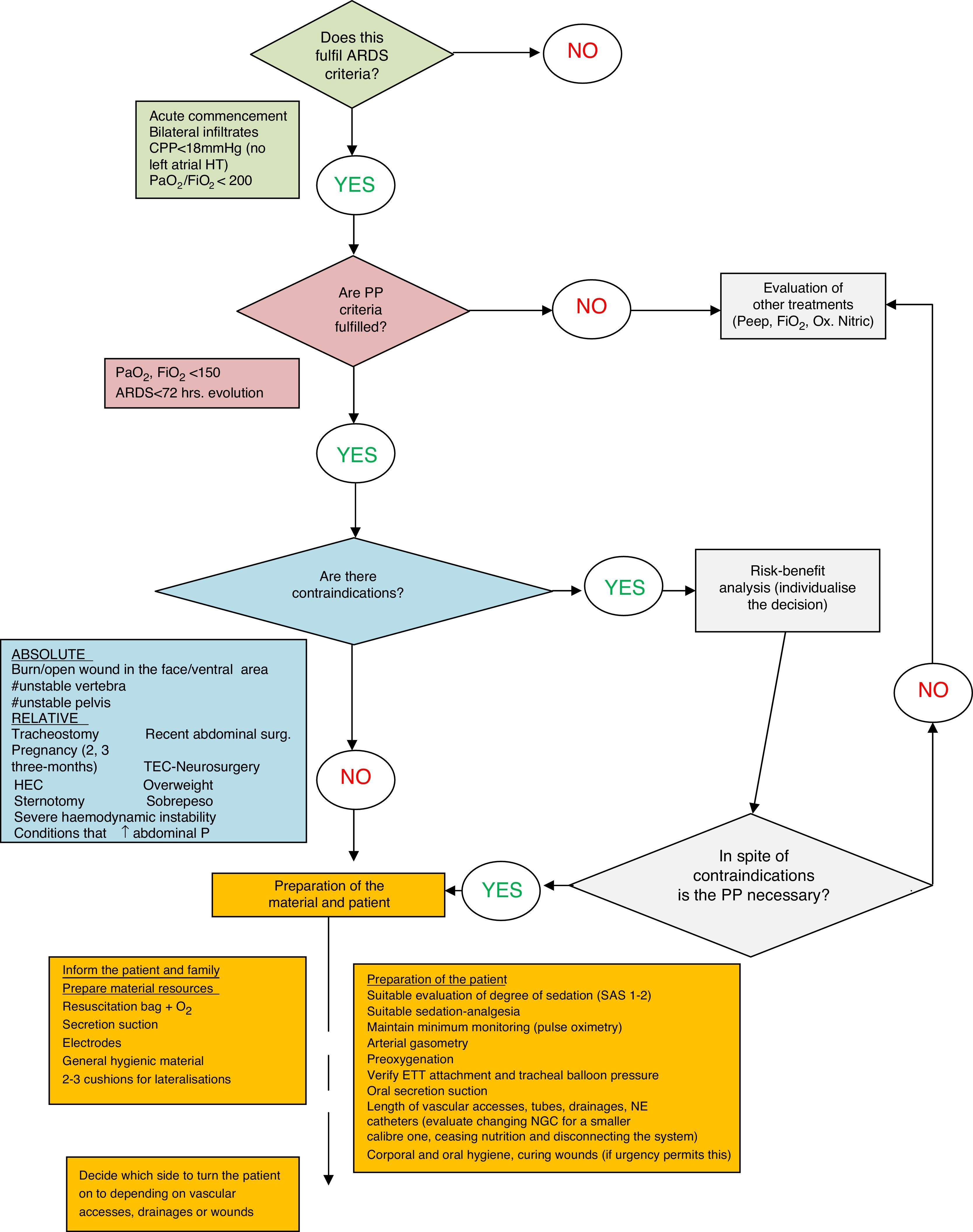
Acute respiratory distress syndrome (ARDS) is a severe acute alteration in pulmonary structure and function that is characterised by severe hypoxaemia, a fall in pulmonary compliance and residual pulmonary capacity1 secondary to an inflammatory lesion of the alveolar–capillary membrane which causes an increase in pulmonary capillary permeability and therefore a diffuse pulmonary oedema.2 ARDS affects more than one million patients in the world each year,3 leading to a high rate of morbimortality in intensive care units. A fall in mortality has been observed recently, although there are studies in different healthcare systems which cite a mortality of 25%–31%4 or even 58%.5,6
Apart from causing ARDS, the severe hypoxaemia which characterises the syndrome means that patients have to be ventilated mechanically to increase arterial oxygenation. Currently, as well as protective mechanical ventilation it is recommended that these patients be placed in the prone position (PP) as a coadjuvant to ventilation strategy, optimising the distribution of the ventilation-perfusion ratio.7
In 1974 Bryan8 described the technique of ventilating patients in the PP for the first time, showing an improvement in arterial oxygenation in patients with pneumonia and ARDS. Different studies were published after this showing an improvement in oxygenation but not that this postural treatment reduced mortality.9–11 Recently, several studies undertaken in the sub-group of patients with severe hypoxaemia (PaFiO2: 150) have suggested the opposite, and the study by Guérin et al.12 confirms the increase in survival of patients diagnosed severe ARDS who are placed in the PP at an early stage.
This postural treatment is a procedure that is increasingly used in Intensive Care Units (ICU). However, in spite of the proven improvement in the oxygenation of ARDS patients treated with this postural change, there is still a certain degree of reticence to use it due to the risk it involves.
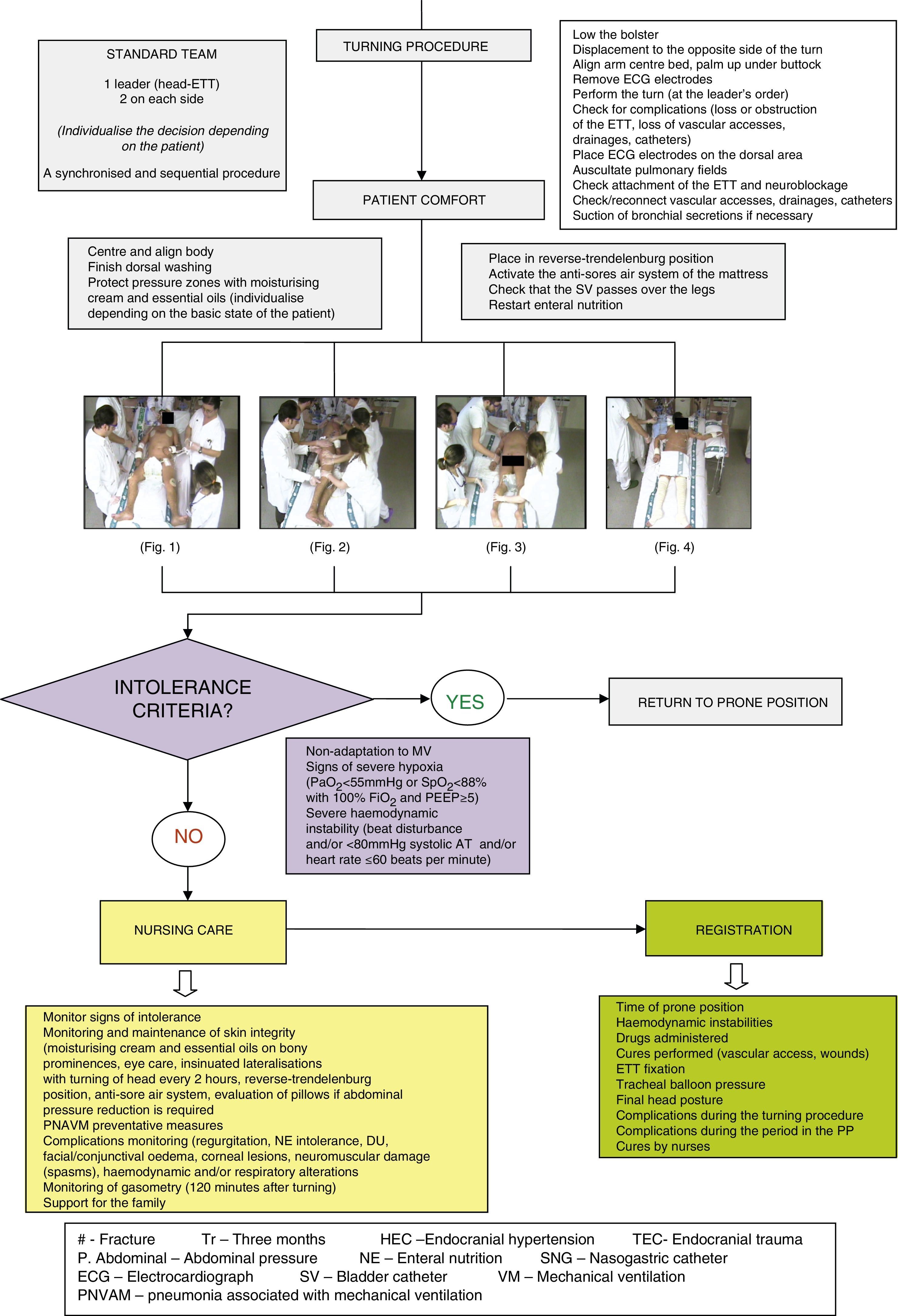
As is the case whenever patients are moved, the responsibility for this postural change lies with the nursing team which, to anticipate and minimise risks, must be aware of the complications associated with this procedure, such as9,13: the accident loss and/or obstruction of the ETT; the accidental loss of vascular accesses, drainages and catheters; cutaneous lesions; facial, palpebral and/or conjuntival oedema; corneal ulcers; muscular-skeletal spasms; brachial plexus lesion; regurgitation and/or intolerance of enteral nutrition and alterations in haemodynamic and/or respiratory state.
In our hospital the procedure for this postural treatment including its possible complications is standardised in a protocol, as may be seen in the algorithm of Appendix A, which schematically summarises all of the phases of the procedure.
Monitoring systems using quality indicators are a method of working that permits the evaluation and improvement of care practices. The Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias (SEMICYUC)14 considers that a quality standard for the PP procedure requires the existence of a registry of all the complications that may arise. These include at the least accidental extubation, the accidental withdrawal of intravascular catheters, the appearance of decubitus ulcers (DU) and ETT obstruction in 100% of cases. The severe complications associated with the implementation of PP treatment are rare. This does not make the monitoring of the same and their documentation any less important, as this makes it possible to evaluate the results of this care technique.
In spite of the importance of this procedure, there are few studies which use scientific evidence to determine the possible causes of severe complications when the PP is used and which make it possible to suggest solutions and improve the quality of care.
The objectives of this study are:
- -
To determine the degree of compliance with the quality standard recommended by the SEMICYUC for the PP.
- -
To identify the incidence of severe complications recorded during the procedures.
- -
To evaluate possible factors associated with the said complications.
A descriptive, retrospective and transversal study undertaken in a multipurpose adult ICU with 16 beds from January 2012 to July 2014.
Study populationPatients admitted to the adult ICU in Sabadell Hospital with a diagnosis of ARDS and treated using the PP from January 2012 to December 2013.
Inclusion criteriaThis study included all of the patients in the adult ICU of Sabadell Hospital admitted with a diagnosis of ARDS and treated with the PP.
Study variables- 1.
The main variable: registration of the PP.
- 2.
Secondary variables:
- •
Socio demographic variables: age and sex.
- •
Clinical variables: main diagnosis and days in the ICU.
- •
Procedural variables:
- -
Variables connected with severe complications of the procedure (during turning manoeuvres and while remaining in the PP): accidental extubations, the accidental withdrawal of catheters, tubes and/or drainages, the appearance of DU (degree and location) and obstruction of the ETT.
- -
Other variables connected with the procedure: hours in the PP, nutrition provided (considering a suitable provision of nutrition to be the administration of 100% prescribed enteral nutrition and parenteral nutrition), type of catheter used for nutrition, regurgitation and/or gastric retention (>250ml), the administration of prokinetic drugs and/or muscle relaxants and the appearance of facial and/or conjuntival oedema.
- -
- •
Two documents were designed to record data. One was used to record all of the PP that were implemented during the study period (including clinical history number, box number, date of the procedure and case number), while the other document was used to record all of the study variables associated with the corresponding case number, to ensure data confidentiality.
Recording processThe study was carried out in two phases. During the first study phase (January 2012–December 2013), the PP work group in the unit recorded all of the procedures in a standardised way. In the second phase of the study (the first six months of 2014) all of the clinical histories of the recorded PP procedures were reviewed, filling out the designed registration document with all of the study variables and analysis of the data obtained.
For those patients who were placed in the PP more than once during admission, each time they were turned was counted as an independent procedure.
Anonymity and data confidentiality were respected, according to Organic Law 15/1999 of 13 December on the Protection of Personal Data (BOE of 14 December 1999). The guidelines of the Ethics Committee of the Institution were followed.
Statistical analysisFor the univariate analysis of continuous variables the relevant measurements of the central and dispersion tendencies were described, as well as the normality tests. Frequency analysis was used for the qualitative variables.
Multivariate analysis with statistical indexes suitable for the characteristics of the variables was used to compare and define the associations between variables. The medians were compared using the Mann–Whitney U test for independent samples. The chi-squared test was used to compare proportions.
A value of p<0.05 with a confidence interval of 95% was considered to indicate statistical significance. The SPSS v. 17 program was used for statistical analysis.
ResultsDuring the first study period 32 patients were registered as diagnosed with ARDS and treated using the PP. A total of 38 cases of the PP were obtained, as 2 patients were placed in this position twice and 2 patients were placed in the prone position three times while in the ICU. In the second study period, after reviewing the clinical histories and determining the degree of compliance with the quality standard recommended by the SEMICYUC in connection with the PP procedure, 3 cases (7.9%) with incomplete records were detected. While in one case the procedure had not been recorded, in the other two although the procedure and the appearance of DU had been recorded, neither the grade nor the location of the latter had been documented. Subsequently the severe complications associated with the PP procedure were analysed together with the factors possibly associated with them in the remaining 35 cases, as the documentation of the incomplete records was not considered to be very reliable.
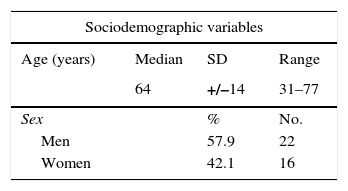
The sociodemographic and clinical variables (age, sex distribution, days of admission in the ICU and main diagnoses) are shown in Table 1, where the most frequent diagnosis is pneumonia.
Sociodemographic and clinical variables.
| Sociodemographic variables | |||
|---|---|---|---|
| Age (years) | Median | SD | Range |
| 64 | +/−14 | 31–77 | |
| Sex | % | No. | |
| Men | 57.9 | 22 | |
| Women | 42.1 | 16 | |
| Clinical variables | |||
|---|---|---|---|
| Days in ICU | Median | SD | Range |
| 26 | +/−27 | 6–123 | |
| Main diagnosis | % | No. | |
| Pneumonia | 42.9 | 15 | |
| ARD | 17.1 | 6 | |
| Aorto-femoral bypass | 8.6 | 3 | |
| Acute pancreatitis | 5.7 | 2 | |
| Septic shock | 5.7 | 2 | |
| Liver cirrhosis | 2.9 | 1 | |
| Alcoholic hepatitis | 2.9 | 1 | |
| Lung neoplasia | 2.9 | 1 | |
| Pulmonary TBC | 2.9 | 1 | |
| A influenza | 2.9 | 1 | |
| Buerguer's disease | 2.9 | 1 | |
| Polytraumatism | 2.9 | 1 | |
ARD: acute respiratory distress; TBC: tuberculosis; ICU: Intensive Care Unit.
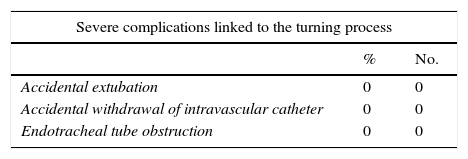
The severe complications associated with the PP procedure that the SEMICYUC includes in the quality standard are shown in Table 2. This shows that the incidence of severe complications due to the turning process (extubation, catheter withdrawal and ETT obstruction) is 0%, and that the only serious complication recorded is DU, with an incidence of 25.7%. These are associated with admission in the PP, and they are mainly grade 2 DU. 88.9% of the DU documented were grade 1 and 2 (reddening and blisters). A total of 9 DU were registered, of which 2 were grade 1 and 6 were grade 2. The grade 1 DU described were located on the ears, cheeks, chin and back of the foot, and the grade 2 ones were on the cheeks, eyelids, abdomen, genitals and scapular waist. Only one grade 4 DU was found, located on the thorax (in the zone of the breast).
Severe complications defined in the SEMICYUC quality standard for the PP.
| Severe complications linked to the turning process | |||
|---|---|---|---|
| % | No. | ||
| Accidental extubation | 0 | 0 | |
| Accidental withdrawal of intravascular catheter | 0 | 0 | |
| Endotracheal tube obstruction | 0 | 0 | |
| Severe complications linked to the duration of the PP | |||
|---|---|---|---|
| Decubitus ulcers | % | No. | Location |
| Grade 1 | 22.2 | 2 | Ears, cheeks, chin and back of foot |
| Grade 2 | 66.7 | 6 | Cheeks, eyelids, abdomen, genitals and scapular waist |
| Grade 3 | 0 | 0 | |
| Grade 4 | 11.1 | 1 | Thorax (breast area) |
| Total | 25.7 | 9 | |
| Facial oedema | 22.8 | 8 | |
| Conjuntival oedema | 14.3 | 5 | |
In 22.8% of cases a facial oedema was registered following the period of lying in the prone position, so that the appearance of conjuntival oedema was recorded in 14.3% of the procedures that were analysed.
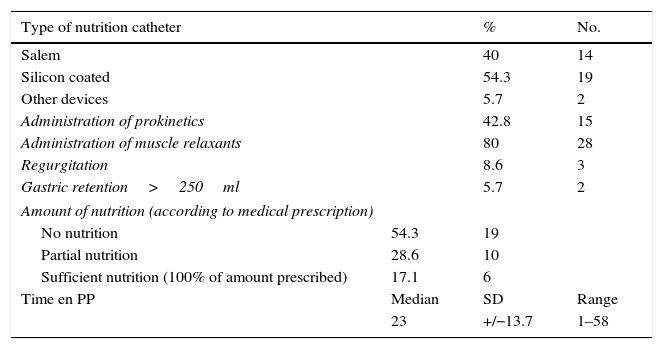
In connection with nutritional variables, such as hours in the PP, the administration of prokinetic drugs and muscle relaxants, nutrition catheter type and the nutrition given (Table 3), the high percentage of patients in the PP who were given muscle relaxants stands out (80%), as does the high percentage of prone patients who did not receive suitable nutrition (82.9%).
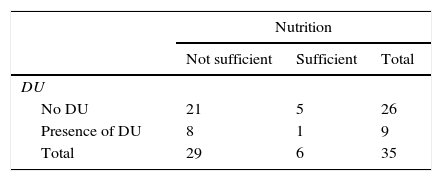
Variables linked to nutrition and the appearance of DU.
| Type of nutrition catheter | % | No. | |
|---|---|---|---|
| Salem | 40 | 14 | |
| Silicon coated | 54.3 | 19 | |
| Other devices | 5.7 | 2 | |
| Administration of prokinetics | 42.8 | 15 | |
| Administration of muscle relaxants | 80 | 28 | |
| Regurgitation | 8.6 | 3 | |
| Gastric retention>250ml | 5.7 | 2 | |
| Amount of nutrition (according to medical prescription) | |||
| No nutrition | 54.3 | 19 | |
| Partial nutrition | 28.6 | 10 | |
| Sufficient nutrition (100% of amount prescribed) | 17.1 | 6 | |
| Time en PP | Median | SD | Range |
| 23 | +/−13.7 | 1–58 | |
PP: prone position.
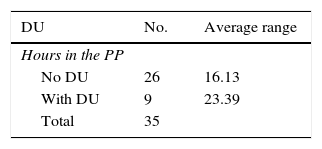
In connection with the possible factors associated with the appearance of DU and as may be seen in Table 4, although the average number of hours in the PP is higher in patients with DU, this difference is not statistically significant (p=0.067). On the other hand, as can be seen in Table 5, more DU were recorded in those patients who had not received appropriate nutrition, although this difference was not statistically significant (p=0.577).
There are several studies on the response of ARDS patients treated in the PP in terms of their oxygenation. They are classified as persistent responders, non-persistent responders or non-responders.13,15 Likewise, some papers describe the absence of improvement in the mortality of the patients subjected to this procedure,9,11 although other studies have been published more recently that suggest the contrary, obtaining an improvement in survival16 and even showing scientific evidence for this in patients with severe ARDS treated at an early stage with the PP.11
Nursing publications can be found on the PP procedure, how to implement it and the associated nursing care.17–19 Nevertheless, the truth is that there are few studies of the possible causes of severe complications due to the PP that provide scientific evidence which would make it possible to consider solutions.
It is true that few complications and adverse effects arise during the procedure, and that they generally involve no risk to life, as is shown by the study by Curley et al.20 in which no critical incident was recorded in more than 200 PP procedures, or the study by Mancebo et al.16 which describes a high incidence of complications, although the majority of these were not considered to be serious for the patient. These data agree with the results obtained in this study.
It should be remembered that the SEMICYUC quality definition for the PP procedure includes the existence of a register of severe complications. These include at least accidental extubation, the accidents withdrawal of intravascular catheters, the appearance of DU and obstruction of the ETT in 100% of cases. The PP protocol of our unit includes the need to record the said complications in the graph of the patient's clinical evolution.
In 92.1% of the cases analysed registration of the complications arising with the procedure was optimum. It should therefore be remembered that nursing records, as well as being a quality tool, make it possible to ensure the continuity of patient information and care.21 It is therefore important to improve compliance with the said clinical documents.22,23 Their absence may even be understood to be a legal, ethical and professional fault that would raise doubts about whether they had ever been prepared.
On the other hand, some studies show that malnutrition is a risk factor in morbidity, increasing the rate of infections, the length of admission to the ICU, days of mechanical ventilation, difficulty in wound scarring and an increase in mortality.24 There is also scientific evidence that nutritional support influences the achievement of better clinical results.25 In connection with the nutrition of these patients, our results (82.9% of ARDS patients treated using the PP did not receive correct nutrition) differ from those obtained in other recent studies. The latter conclude that ARDS patients in the PP tolerate enteral nutrition and receive suitable nutrition. They also suggest the benefit of the prophylactic administration of prokinetic drugs.26
On the other hand, some works show the incidence of intolerance to enteral nutrition in patients of this type amounts to 58.62%.27 Other studies, such as the one by Reignier et al.,28 state that in cases of early enteral nutrition in patients in the PP more episodes of intolerance are detected, at 82% vs 49%. Two options that should be considered to improve these complications are that smaller volumes be administered and that prokinetic drugs and nasojejunal catheters be used.
In connection with the high incidence of DU, the results obtained in this study are similar to those obtained by other authors. These state that grade 2 and 3 DU appear in 27.58 and 10.34% of cases, respectively,27 while palpebral and/or conjuntival oedema occurs in 17.24% of patients in the PP. Another aspect that should be taken into account in connection with the results obtained for DU would be the time spent in the PP. Currently there is no recommendation with a scientific basis for the time that a patient should spend in this position, although one recently published paper states that there is a tendency to increase the periods of time during which patients remain in the PP.12
To conclude, and respecting the severe complications associated with the turning procedure, no accidents loss of the ETT, tracheostomy cannula, catheter (nasogastric or bladder), drainage and/or vascular access. This result is similar to those obtained in other studies, so that the PP may be said to be a safe procedure, as other publications on this postural treatment conclude.9,29
This study took place in an ICU with broad experience in the PP procedure. Its main limitations are the size of its sample and single-hospital nature, as well as the bias intrinsic to a retrospective analysis that depends on the quality of the information collected.
ConclusionsNurses play an important role in preparing a patient for turning, implementing the turn and care of the patient while they remain in this position, as well as in the prevention of possible complications.
The percentage of suitably kept records in connection with the PP is very high, even though the quality standard recommended by the SEMICYUC was not met.
This study shows the procedure to have a high level of safety as no severe complications were recorded in any case that compromised the life of a patient.
DU is the only severe complication found in the implementation of this procedure, and they are mainly grade 1 and 2. In connection with possible factors associated with the appearance of DU it should be underlined that, even though the relationship between the appearance of DU and time spent in the PP is not statistically significant, a tendency may be observed here. On the other hand, fewer DU occur in patients who have received suitable nutrition, while the percentage of patients in the PP who do not receive suitable nutrition is very high.
The results obtained encourage us to continue performing studies that provide scientific evidence for the factors which may lead to the appearance of DU so that they can be prevented, while also considering how important nursing staff believe their own records to be.
It was also found to be important to create and implement a specific document to record the PP procedure, showing the sociodemographic and clinical data of the patient as well as the procedural data (hours in the PP, the appearance or absence of severe complications and a description of the same). This document must be included in the procedure protocol to standardise recording and improve the quality of care.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments took place in human being or animals for this research.
Data confidentialityThe authors declare that no patient data appear in this paper.
Right to privacy and informed consentThe authors declare that no patient data appear in this paper.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank everybody who has contributed to this work in the form of specific contributions or by their support and encouragement.
We would like to thank the whole Intensive Care nursing team for their enthusiasm during this time.
Ms. A. Estruga and Mr. Ll. Domènech and Mr. F. Rodríguez for their support and contribution.
Dr. X. García for his time, for sharing his knowledge, revising the manuscript and offering his remarks.
Very special thanks to Ms. R. Jam for her time, dedication and support in the development of this research, for sharing her knowledge, offering specific input and revising the manuscript, as well as for her support and encouragement.
Ms. Carmen Martín, Head of Intensive Care Nursing and Nursing Management, Ms. Carmen Díaz for her support and encouragement of the research and scientific development of the nursing profession.
Please cite this article as: Jové Ponseti E, Villarrasa Millán A, Ortiz Chinchilla D. Análisis de las complicaciones del decúbito prono en el síndrome de distrés respiratorio agudo: estándar de calidad, incidencia y factores relacionados. Enferm Intensiva. 2017;28:125–134.