Strongyloides stercoralis infection is more prevalent in tropical regions but autochthonous cases have been reported in Spain, mainly in La Safor (Valencia). The objective is to describe the strongyloidiasis cases registered in a regional hospital of Alicante province (Spain) and to determine if they were autochthonous cases.
MethodsRetrospective study of all diagnosed cases of strongyloidiasis in Vega Baja Hospital (Orihuela, Alicante) between January 1999 and March 2016.
ResultsA total of 10 cases were found, four of which were autochthonous cases. Two of them presented with a hyper-infection syndrome, with a fatal outcome. All autochthonous cases were in patients ≥69years old with gastrointestinal, cutaneous, and/or respiratory symptoms. Serology was positive in the 8 cases studied. Larvae were found in histopathological samples of the gastrointestinal tract of three patients.
ConclusionsWe communicate the first autochthonous cases of strongyloidiasis in the region of Vega Baja. Screening programs should be implemented, especially in immunosuppressed patients or patients under chronic corticosteroid treatment.
La infestación por Strongyloides stercoralis es más prevalente en regiones tropicales, pero existen casos autóctonos en España, principalmente en La Safor (Valencia). Nuestro objetivo era estudiar los casos de un hospital de la provincia de Alicante y conocer si existían casos autóctonos.
ProcedimientoEstudio retrospectivo de los casos diagnosticados de estrongiloidiasis en el Hospital Vega Baja (Orihuela, Alicante) entre enero de 1999 y marzo de 2016.
ResultadosSe registraron 10 casos, 4 de ellos autóctonos, presentando 2 de ellos un cuadro de hiperinfestación con desenlace fatal. Todos los casos autóctonos fueron en personas ≥69años con síntomas digestivos, cutáneos y/o respiratorios. La serología fue positiva en los 8casos en los que se realizó. En 3 casos se visualizaron larvas en el estudio histopatológico.
ConclusionesComunicamos los primeros casos autóctonos de estrongiloidiasis en la región Vega Baja. Se deben implantar programas de cribado principalmente en pacientes inmunosuprimidos o en tratamiento corticoideo.
Strongyloides stercoralis is an intestinal nematode usually contracted by walking barefoot on contaminated soil. It has the unusual characteristic of self-infection of the host, thereby producing infections that persist for decades.1 Clinical manifestations may vary from an asymptomatic state to cutaneous disorders (pruritus, larva currens, urticaria), digestive disorders (diarrhoea, abdominal pain), respiratory disorders (chronic cough, dyspnoea) or life-threatening conditions such as hyperinfection syndrome. This syndrome is associated primarily with situations of immunosuppression, especially therapy with corticosteroids.2
Strongyloidiasis is a parasitic infection that is most prevalent in tropical and subtropical areas; however, sporadic cases have been reported in temperate regions.1 In Spain, its incidence has recently increased due to migration flows and international travel.3 Furthermore, autochthonous cases have been reported in Spain, mainly in the La Safor and Marina Alta (Valencia) region.4 Our objective was to describe cases of strongyloidiasis at Hospital Vega Baja (Orihuela, Alicante), a regional hospital in eastern Spain, and to determine whether there were any autochthonous cases.
Material and methodsA retrospective analysis was performed of all diagnosed cases of strongyloidiasis recorded in the admission records and clinical, microbiology and anatomical pathology documentation of Hospital Vega Baja (Orihuela, Alicante) between January 1999 and March 2016. All cases with parasitological diagnosis (wet mount and/or stool culture, duodenal aspirate culture and other cultures), serological diagnosis (positive Strongyloides IgG) or anatomical pathology diagnosis (visualisation of Strongyloides larvae in biopsy) were included. Serological tests were performed at the National Microbiology Centre using the ELISA technique (DRG Instruments GmbH, Marburg, Germany), considering a titre of ≥1.1 to be positive. A stool concentration method was used for the intestinal parasites study, using the ParaSAF system (with 3.3ml of sodium acetate-acetic acid-formalin and Triton X) and collecting at least 3 samples per patient. For the Strongyloides culture, the specimen was streaked onto a Mueller-Hinton agar plate, incubated at 28°C and observed for 5 days to monitor the presence of sinuous tracks.
Cases were classified as follows: (a) autochthonous, if the patient had never travelled to an area considered to be a Strongyloides endemic region; or (b) imported, if the patient had come from (immigrant) or travelled (traveller) to an endemic region.
Data on the following patient characteristics were collected: demographic (age, gender, place of birth, trips to Strongyloides endemic regions, farm work); clinical (symptoms, co-morbidities, treatment and outcome); analytical (eosinophilia); and microbiological (antibody titre, visualisation of larvae, Strongyloides culture, HIV serology). An absolute figure of eosinophils >0.5×109/l was considered to show eosinophilia. Hyperinfection syndrome was defined as the onset of signs and symptoms attributable to accelerated autoinfection and increased larval migration. Larval migration outside the skin, gastrointestinal tract and lungs involving other organs was considered disseminated strongyloidiasis.
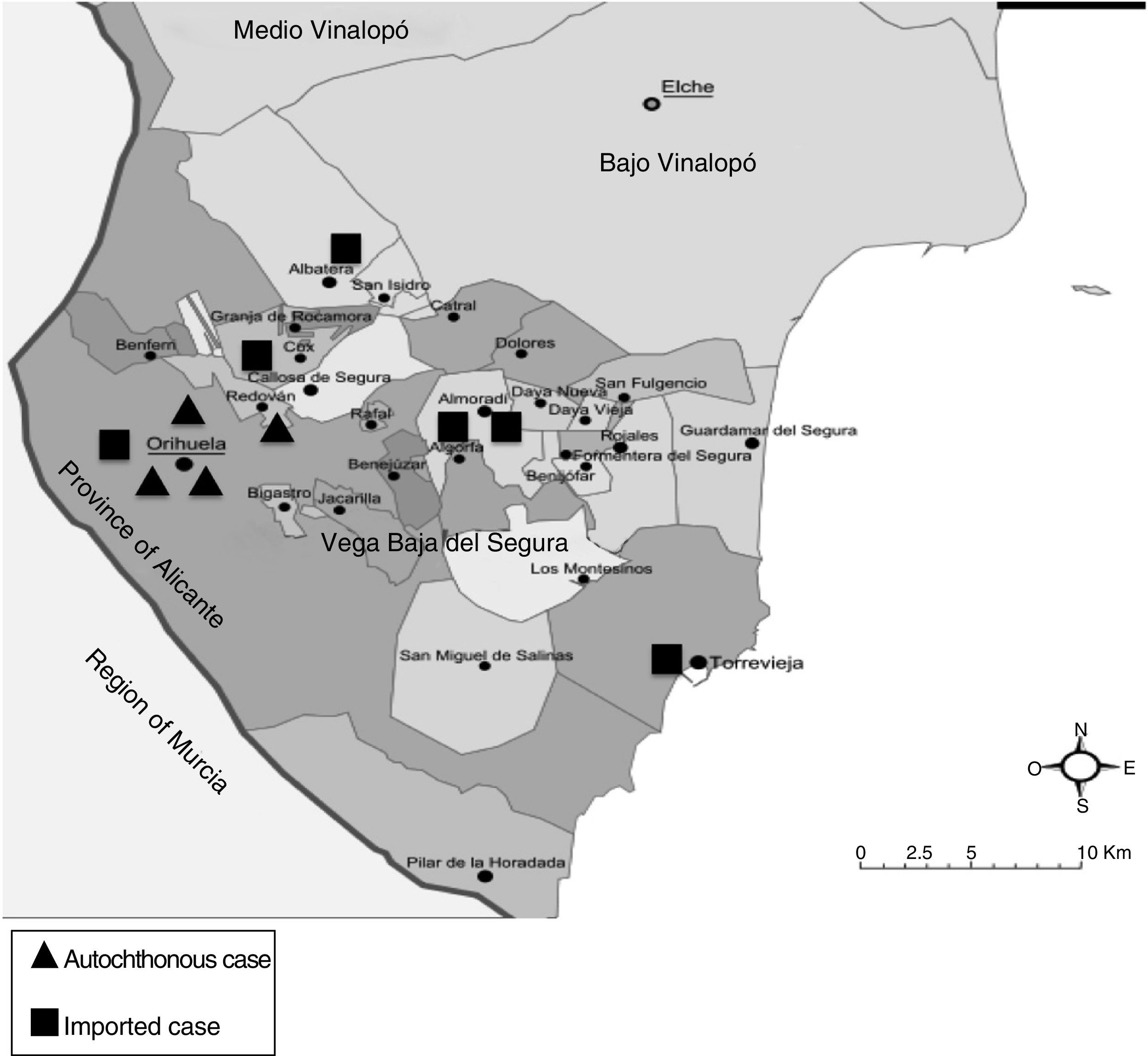
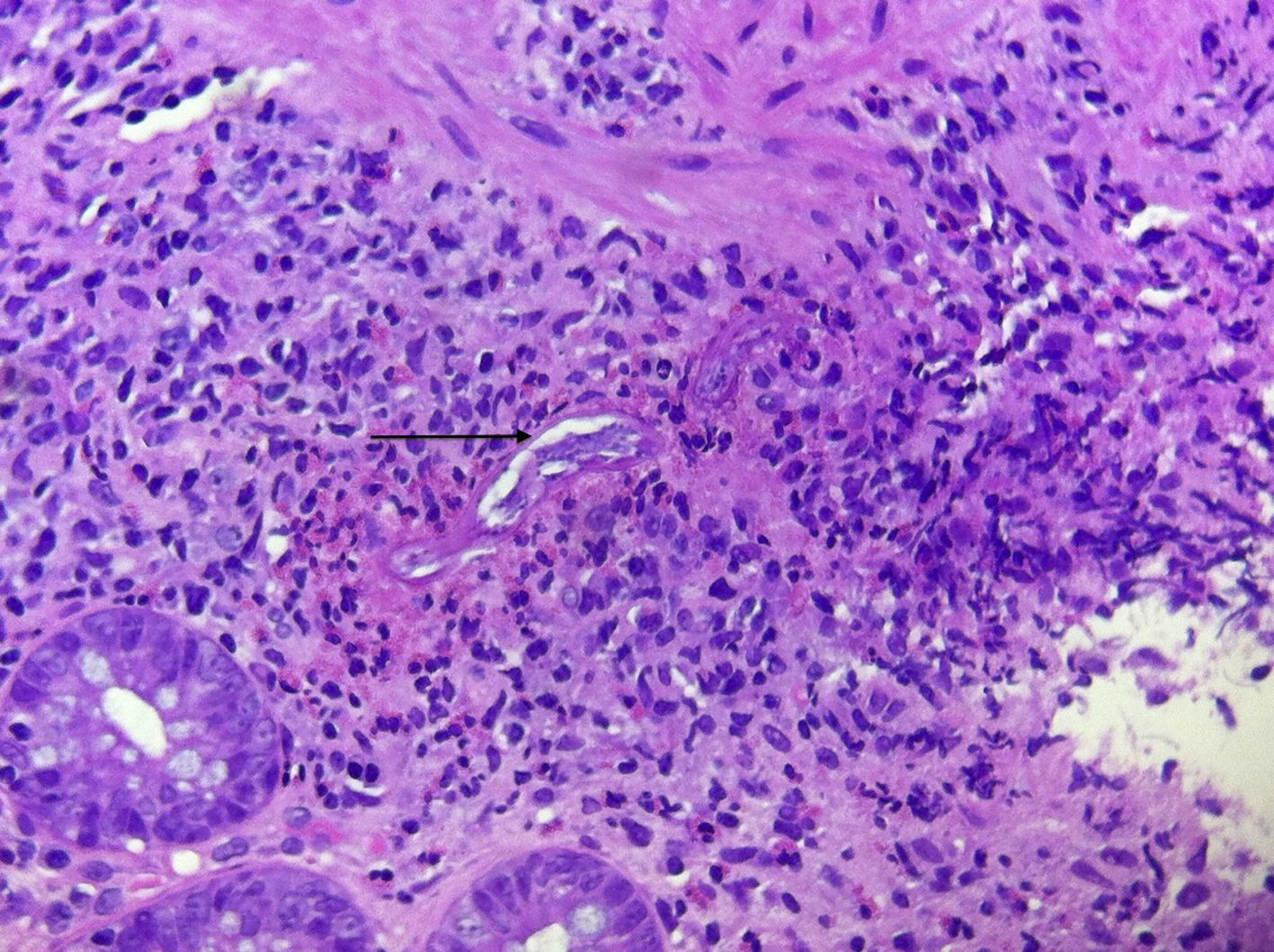
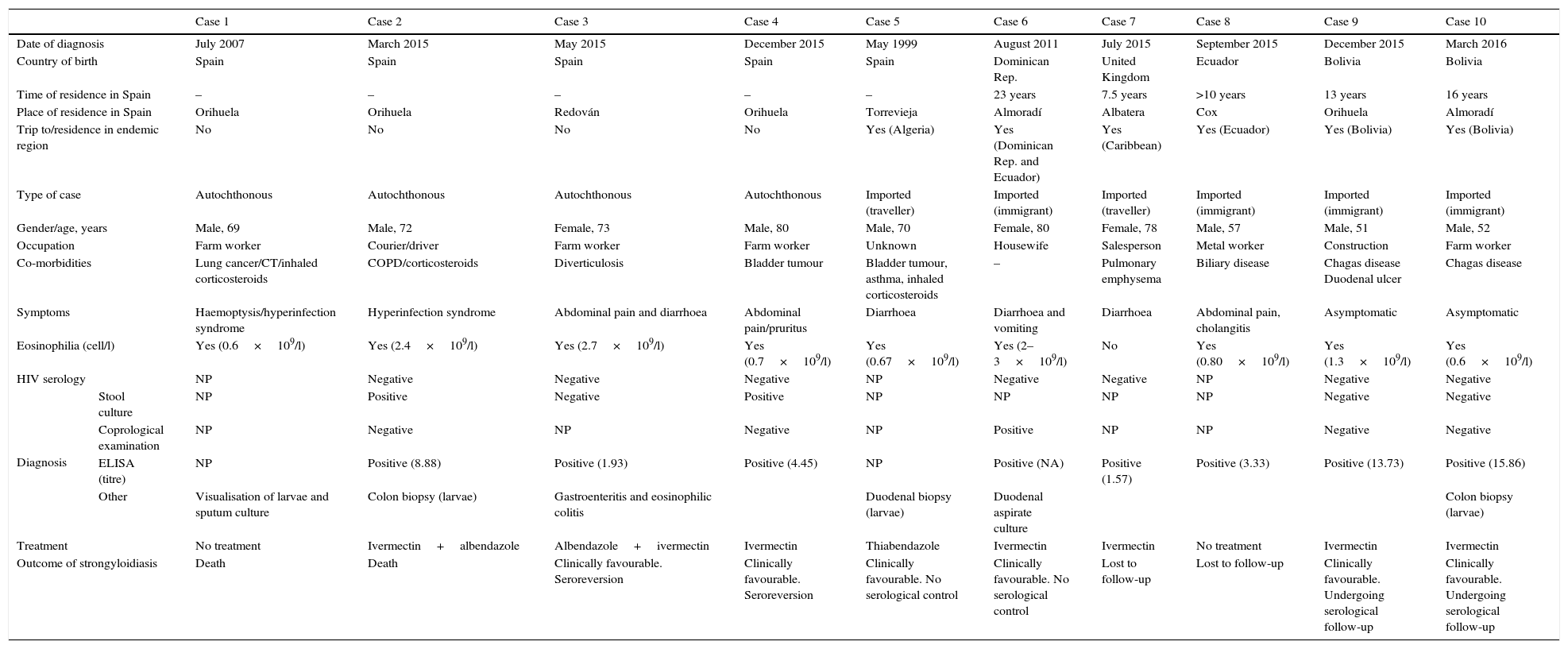
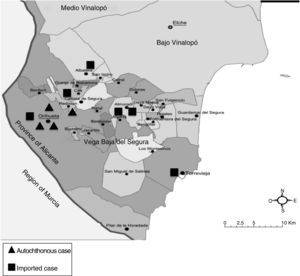
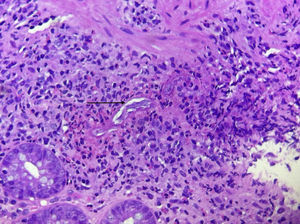
ResultsBetween January 1999 and March 2016, 10 cases of strongyloidiasis were diagnosed (70% male, mean age 68±11 years), 4 of which were autochthonous (Table 1). Patients carried out agricultural work in all 4 autochthonous cases, either as an occupation or as a hobby (case 2). Four of the imported cases were from Latin America (Dominican Republic [1], Ecuador [1] and Bolivia [2]), one case was an English woman who frequently travelled to the Caribbean (case 7) and another was a Spanish citizen who lived in Algeria for more than 5 years (case 5). In all cases, the time of residence in Spain at the time of diagnosis was >7 years. Fig. 1 shows the distribution of cases according to their town of residence in the Vega Baja region. Of the 6 imported cases, 2 were asymptomatic and the remaining 4 had digestive symptoms. All autochthonous cases were symptomatic, with digestive (mainly diarrhoea and abdominal pain) and/or cutaneous symptoms (pruritus, often present for several years). Two cases had hyperinfection syndrome. The first was a patient with lung cancer receiving chemotherapy (case 1) who developed dyspnoea, fever and haemoptysis, with abundant larvae visualised in the sputum test. This patient died 48 hours after admission and his death was attributed to cancer-related complications. The second case of hyperinfection was a patient with COPD undergoing chronic corticosteroid treatment (case 2) who was readmitted a few days after discharge because of worsening COPD with fever, abdominal pain and paralytic ileus. A colonoscopy was performed, which revealed granulomatous colitis. Strongyloides larvae were found in the colon biopsy and also in a subsequent stool culture. Treatment was started with ivermectin but had to be replaced with albendazole 2 days later due to a shortage of supply. The patient died 14 days later. 90% of the cases had eosinophilia at the time of diagnosis. The Strongyloides stercoralis test was positive in all 8 cases undergoing this test. A stool culture was performed in 6 patients and the results were positive in 2 of them. Diagnosis was made in 3 patients as a result of visualisation of larvae in anatomical pathology tests (2 colon biopsies [Fig. 2] and one duodenal biopsy). One patient was diagnosed by duodenal aspirate culture and another was diagnosed by sputum culture. One case was treated with thiabendazole, 5 were treated with ivermectin and 2 were treated with ivermectin plus albendazole. Three patients were lost to follow-up, one before starting treatment.
Cases of strongyloidiasis diagnosed at Hospital Vega Baja (Orihuela, Alicante) during the study period.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Date of diagnosis | July 2007 | March 2015 | May 2015 | December 2015 | May 1999 | August 2011 | July 2015 | September 2015 | December 2015 | March 2016 | |
| Country of birth | Spain | Spain | Spain | Spain | Spain | Dominican Rep. | United Kingdom | Ecuador | Bolivia | Bolivia | |
| Time of residence in Spain | – | – | – | – | – | 23 years | 7.5 years | >10 years | 13 years | 16 years | |
| Place of residence in Spain | Orihuela | Orihuela | Redován | Orihuela | Torrevieja | Almoradí | Albatera | Cox | Orihuela | Almoradí | |
| Trip to/residence in endemic region | No | No | No | No | Yes (Algeria) | Yes (Dominican Rep. and Ecuador) | Yes (Caribbean) | Yes (Ecuador) | Yes (Bolivia) | Yes (Bolivia) | |
| Type of case | Autochthonous | Autochthonous | Autochthonous | Autochthonous | Imported (traveller) | Imported (immigrant) | Imported (traveller) | Imported (immigrant) | Imported (immigrant) | Imported (immigrant) | |
| Gender/age, years | Male, 69 | Male, 72 | Female, 73 | Male, 80 | Male, 70 | Female, 80 | Female, 78 | Male, 57 | Male, 51 | Male, 52 | |
| Occupation | Farm worker | Courier/driver | Farm worker | Farm worker | Unknown | Housewife | Salesperson | Metal worker | Construction | Farm worker | |
| Co-morbidities | Lung cancer/CT/inhaled corticosteroids | COPD/corticosteroids | Diverticulosis | Bladder tumour | Bladder tumour, asthma, inhaled corticosteroids | – | Pulmonary emphysema | Biliary disease | Chagas disease Duodenal ulcer | Chagas disease | |
| Symptoms | Haemoptysis/hyperinfection syndrome | Hyperinfection syndrome | Abdominal pain and diarrhoea | Abdominal pain/pruritus | Diarrhoea | Diarrhoea and vomiting | Diarrhoea | Abdominal pain, cholangitis | Asymptomatic | Asymptomatic | |
| Eosinophilia (cell/l) | Yes (0.6×109/l) | Yes (2.4×109/l) | Yes (2.7×109/l) | Yes (0.7×109/l) | Yes (0.67×109/l) | Yes (2–3×109/l) | No | Yes (0.80×109/l) | Yes (1.3×109/l) | Yes (0.6×109/l) | |
| HIV serology | NP | Negative | Negative | Negative | NP | Negative | Negative | NP | Negative | Negative | |
| Diagnosis | Stool culture | NP | Positive | Negative | Positive | NP | NP | NP | NP | Negative | Negative |
| Coprological examination | NP | Negative | NP | Negative | NP | Positive | NP | NP | Negative | Negative | |
| ELISA (titre) | NP | Positive (8.88) | Positive (1.93) | Positive (4.45) | NP | Positive (NA) | Positive (1.57) | Positive (3.33) | Positive (13.73) | Positive (15.86) | |
| Other | Visualisation of larvae and sputum culture | Colon biopsy (larvae) | Gastroenteritis and eosinophilic colitis | Duodenal biopsy (larvae) | Duodenal aspirate culture | Colon biopsy (larvae) | |||||
| Treatment | No treatment | Ivermectin+albendazole | Albendazole+ivermectin | Ivermectin | Thiabendazole | Ivermectin | Ivermectin | No treatment | Ivermectin | Ivermectin | |
| Outcome of strongyloidiasis | Death | Death | Clinically favourable. Seroreversion | Clinically favourable. Seroreversion | Clinically favourable. No serological control | Clinically favourable. No serological control | Lost to follow-up | Lost to follow-up | Clinically favourable. Undergoing serological follow-up | Clinically favourable. Undergoing serological follow-up | |
COPD: chronic obstructive pulmonary disease; CT: chemotherapy; NA: not available; NP: not performed.
This study looks at cases of Strongyloides stercoralis infection at Hospital Vega Baja (Alicante), a hospital that covers an area of 171,000 inhabitants with an average of 15,479 admissions per year, which had not reported previous autochthonous cases.
In Spain, the first case of autochthonous strongyloidiasis was described in 1895 and the first case of disseminated strongyloidiasis was published in 1987 in a post-mortem study.5 A significant number of autochthonous cases has subsequently been reported, the majority of which have been limited to a specific area of the La Safor and Marina Alta regions, corresponding to Health Area 11 of the Valencia Community, and reported by a single group.4,6 In these regions, prevalence ranges between 0.3% for the general population and 12.4% for high-risk groups. Most cases affect males above the age of 50 engaged in farming activities.7 In a more recent study by the same group, prevalence in the town of Oliva was 0.9%. There is probably no active transmission at present given the absence of cases in young people and changes in farming practices.7 Four cases have also been reported in COPD patients in the rural region of Vega del Segura in Murcia, a region that is very close to the Vega Baja region.8,9 Outside these regions, a few isolated cases have been reported in autochthonous patients, most of which have only been diagnosed by serological diagnosis,10–13 which is why some authors consider that Spain should not be considered an endemic country for strongyloidiasis.14
In this study, we have described at least 4 autochthonous cases of strongyloidiasis in a different region that is relatively close to the region that, to date, has the highest number of cases. Sociodemographic characteristics seem to be similar to those described in that region, i.e. prevalence of elderly males engaged in farming activities.7 The fact that all autochthonous patients were symptomatic and 2 of them had hyperinfection syndrome is concerning and leads us to believe that strongyloidiasis is probably underdiagnosed in our region. Given the potential severity of strongyloidiasis in immunosuppressed patients, especially in those treated with corticosteroids, we believe strongyloidiasis screening protocols need to be introduced urgently in patients from Vega Baja who have occupational risk factors or eosinophilia or compatible symptoms, similar to the screening protocols recommended for immigrants and people travelling to endemic regions.2,15 One alternative, particularly if there are no adequate diagnostic techniques or sufficient time to complete screening, is to give empirical treatment with ivermectin to immunosuppressed patients at high risk of Strongyloides6 infection. The treatment of choice for strongyloidiasis is ivermectin, which is available in Spain as an imported drug. Other drugs, such as albendazole or thiabendazole, are less effective and their use is therefore not currently recommended. It is important, therefore, to have plenty of ivermectin in stock.
In our study, many of the cases occurred over the past year, probably because healthcare staff are more aware of the presence of autochthonous cases and the need for immigrant screening. However, we cannot rule out the possibility that the geohelminth was contracted in Spain in some of those cases classified as imported, given that several of the patients had lived in the Vega Baja region for a long period of time and had epidemiological risk factors. Another limitation of our study is the use of different diagnostic methods over time. It is well known that the sensitivity of the larvae detection and stool culture techniques does not exceed 50%.1 Serology is more sensitive, but has not been used on a regular basis until recently. On the other hand, it can produce false positives due to cross-reactions with other helminths, mainly filariae. However, it is considered a technique of choice for the screening of asymptomatic immigrants and can also be used to confirm the effectiveness of treatment.15,16 The use of RT-PCR assays for stool samples is promising, with a sensitivity of >90%,17 and this assay technique could be used in the future.
ConclusionsIn the Vega Baja region, there are autochthonous cases of strongyloidiasis that seem to mainly affect elderly people engaged in farming activities. Screening protocols for asymptomatic patients at risk of developing hyperinfection syndrome should be urgently implemented for both the autochthonous and immigrant population. Likewise, strongyloidiasis should be considered in all autochthonous or immigrant patients with compatible skin, gastrointestinal and/or lung symptoms, particularly in the presence of epidemiological risk factors.
FundingNone.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to thank the National Microbiology Centre and especially Dr Esperanza Rodríguez de las Parras for performing serological techniques. We would also like to thank all the physicians at Hospital Vega Baja involved in caring for these patients, especially Dr Belén Martínez López and Dr Carlos Jiménez Guardiola from the Internal Medicine Department and Dr Nieves Gonzalo Jiménez and Dr Emilio Federico Borrajo Brunete from the Microbiology Department.
Please cite this article as: Pacheco-Tenza MI, Ruiz-Maciá JA, Navarro-Cots M, Gregori-Colomé J, Cepeda-Rodrigo JM, Llenas-García J. Strongyloides stercoralis en un hospital comarcal del Levante español: una enfermedad no solo importada. Enferm Infecc Microbiol Clin. 2018;36:24–28.