Our patient is a 24-year-old woman of Paraguayan origin who had resided in Spain for the last 6 years, with a late diagnosis of HIV infection with cerebral toxoplasmosis, Pneumocystis jiroveci-induced pneumonia, Cytomegalovirus-induced viraemia and 12μl CD4 lymphocytes.
The patient progressed clinically and radiologically in a favourable manner with pyrimethamine 75mg/day orally (PO), clindamycin 900mg/8h intravenously (IV), primaquine 30mg/day PO (digestive intolerance to sulfonamides), and ganciclovir 300mg/12h IV, but by the third week the patient presented elevated transaminases with AST 890U/ml and ALT 1360U/ml, followed by recurring fever, polymorphic skin rash consisting of papules, vesicles and nodules, limited to the face and neck region (Fig. 1), and progressive pancytopaenia. No mucosal lesions were observed.
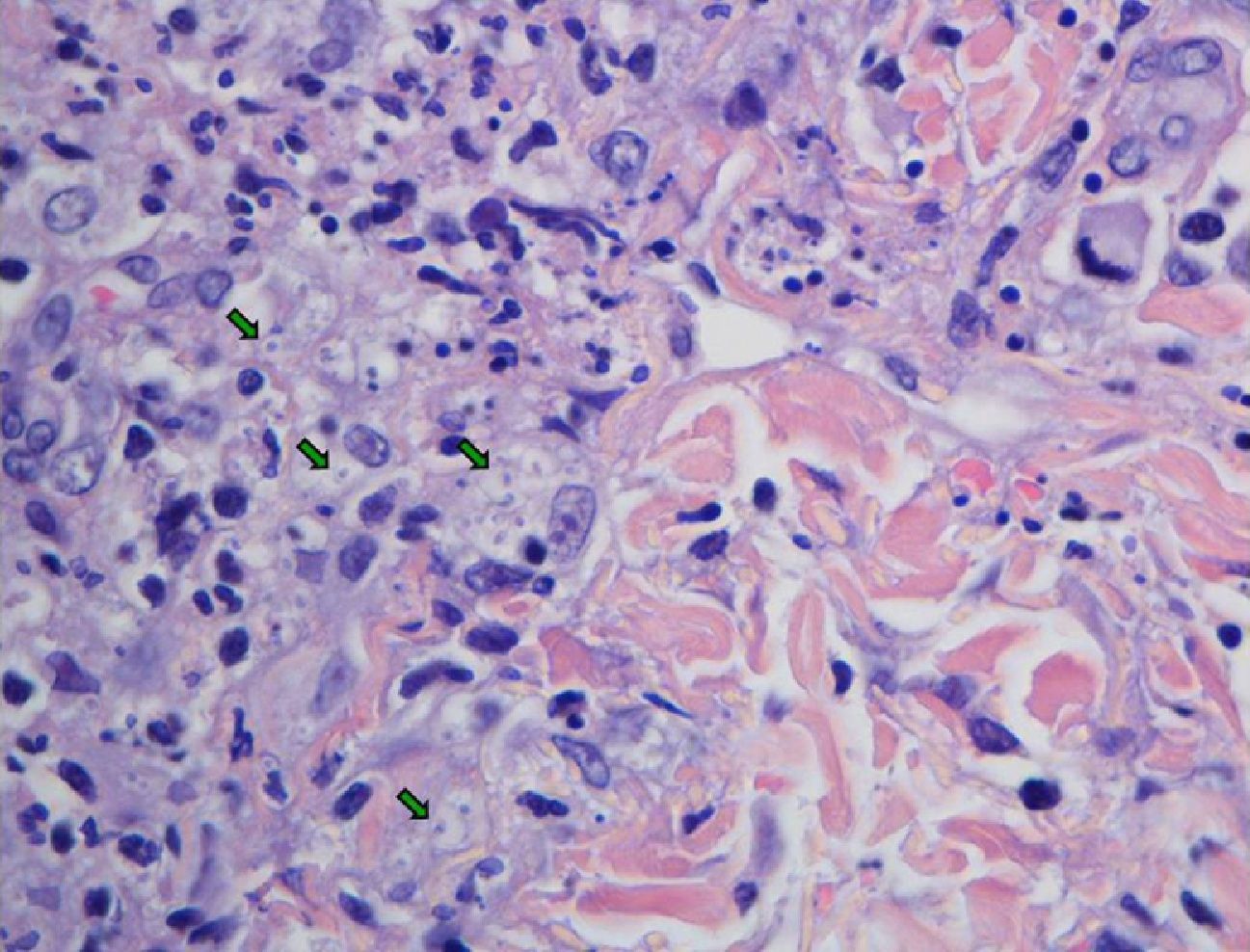
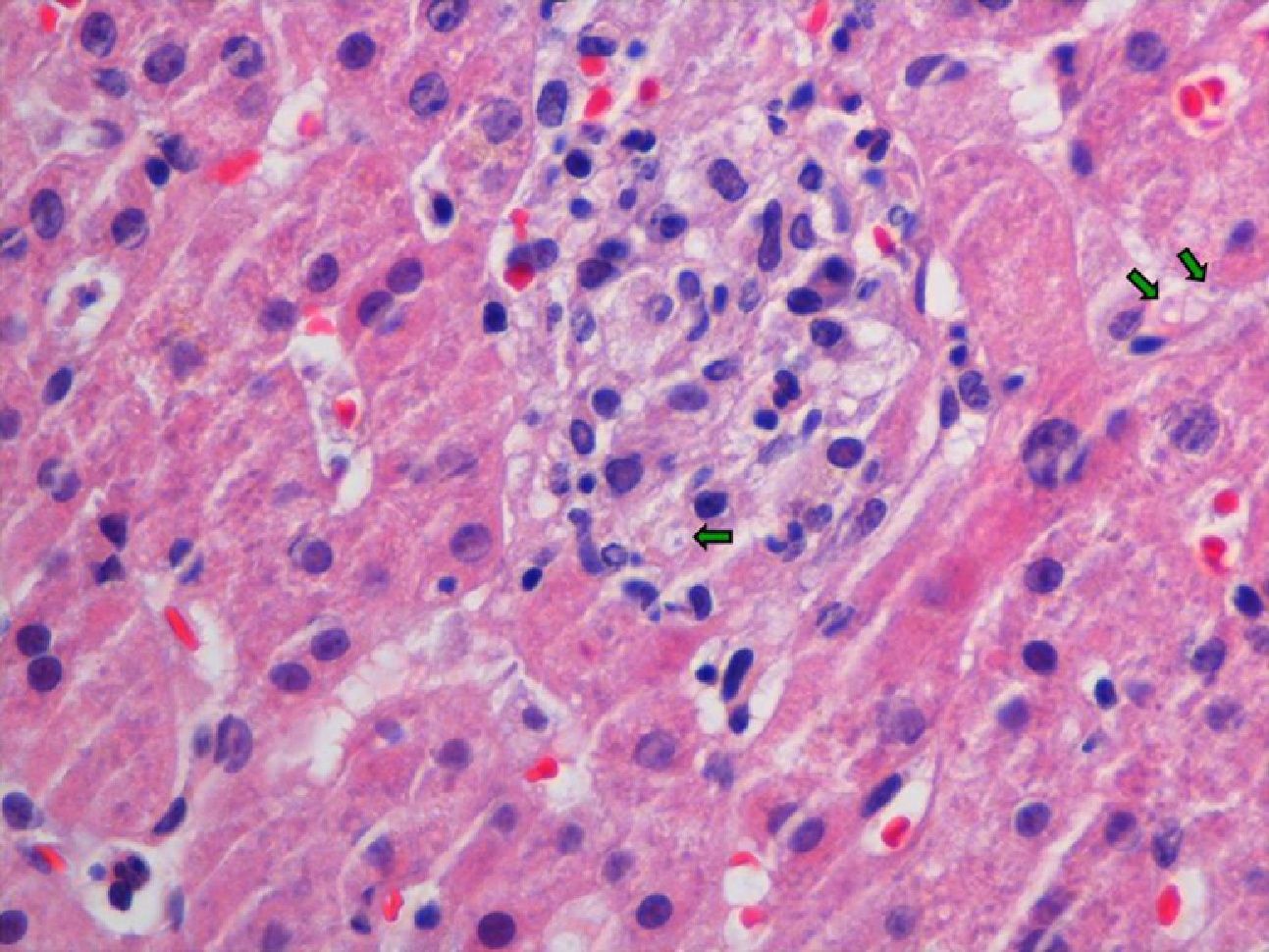
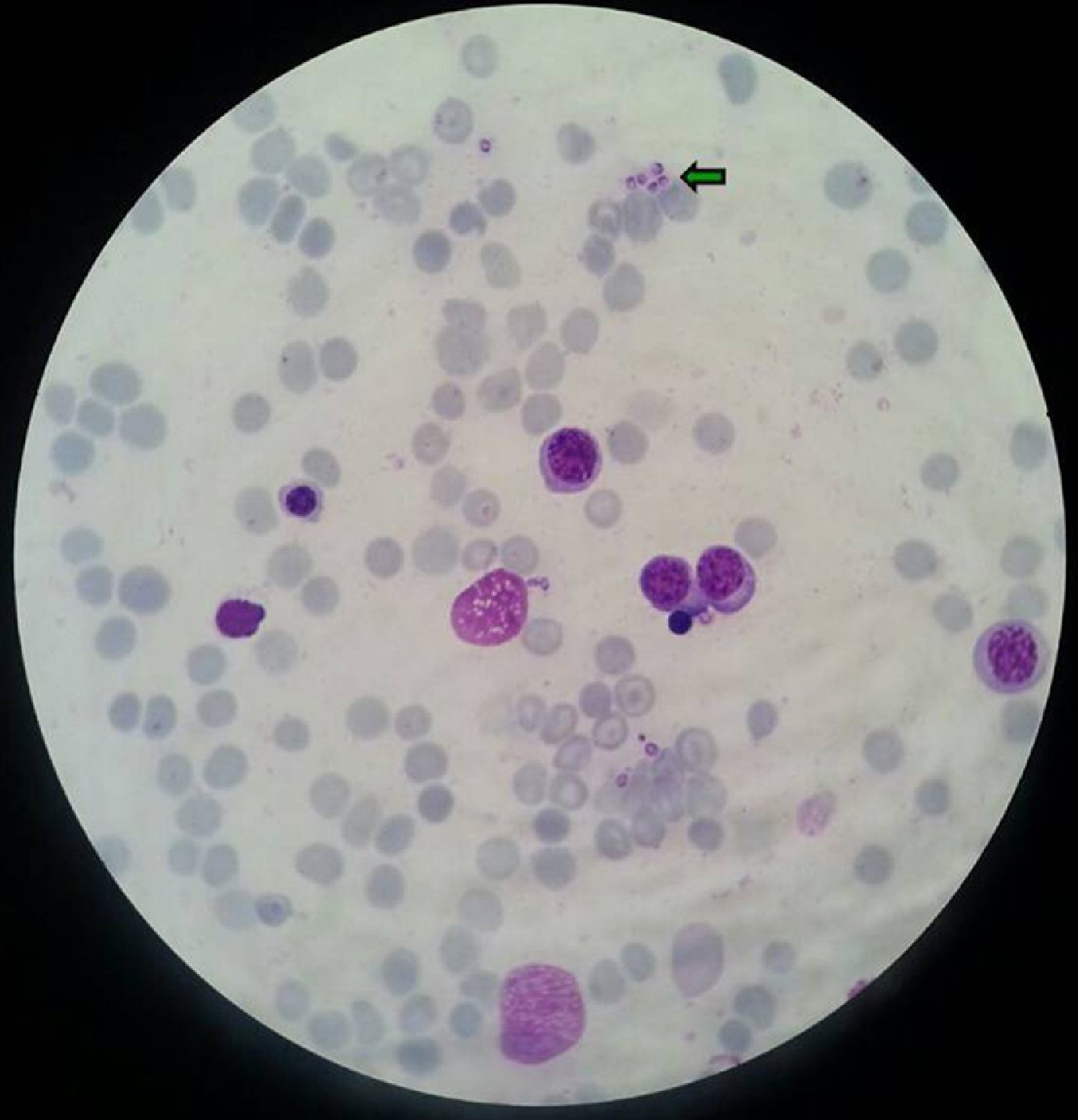
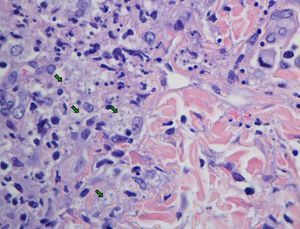
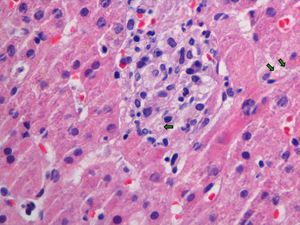
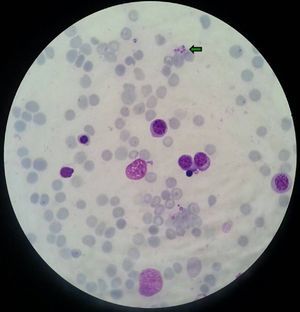
Clinical courseThe blood cultures showed serum cryptococcus antigen, and syphilis, hepatitis B, C, endemic mycosis (Histoplasma capsulatum, Coccidioides immitis, Paracoccidioides and Blastomyces dermatitidis) serology were negative. The abdominal CT scan only showed a 14cm splenomegaly. A skin biopsy (Fig. 2), liver biopsy (Fig. 3), and bone marrow aspiration (Fig. 4) were performed, where small yeast cells (<5mm) with a thin capsule were observed, compatible with H. capsulatum, which grew in BHI (brain heart infusion) agar plates on the 5th day.
The patient completed 6 weeks of toxoplasmosis treatment and 3 weeks of Pneumocystis treatment and continued secondary prophylaxis with pyrimethamine 50mg/day and atovaquone 5mg/12h. Antiretroviral treatment was introduced with one Truvada® tablet (200mg of emtricitabine and 245mg of tenofovir)/24h, darunavir 800mg/24h and ritonavir 100mg/24h, and the patient was started on amphotericin B lipid complex 5mg/kg/day for 15 days with good progress, followed by oral itraconazole 200mg/12h for 3 months. Due to the patient's financial difficulties, she continued treatment with amphotericin B lipid complex for 13 months (initially 5mg/kg/week IV for 4 months, followed by 5mg/kg/month for 9 months). By the time the secondary prophylaxis was suspended, the patient had received 15 months of antiretroviral treatment, the last 6 of which with CD4>150cells/μl.
DiagnosisDisseminated histoplasmosis.
CommentsH. capsulatum is an endemic dimorphic fungus found from the south of the United States through South America that behaves as an opportunistic pathogen, causing localised lung disease in HIV patients with high CD4 levels, and disseminated disease in patients with CD4<150cells/μl.1 In endemic regions, the annual incidence of histoplasmosis in HIV patients without antiretroviral treatment is 5%; therefore, primary prophylaxis with itraconazole (200mg/day) should be considered until CD4>150μl is maintained for at least 6 months.1
In our patient, the first clinical manifestation attributable to histoplasmosis was transaminases elevated more than 10-fold above the upper limit of normal, which was not attributable to hepatotoxicity or to other typical causes. Hepatitis as an initial manifestation of histoplasmosis reactivation is rare, although cases have been described in patients infected with HIV or with other causes of cellular immunosuppression.2–4
Skin lesions have been described in 10–15% of patients with disseminated histoplasmosis, and they are more common in patients with AIDS. Observable lesions include nodules, papules, plaques, ulcers, vesicles, pustules, abscesses and dermatitis. Our case presented the peculiarity that the lesions appeared exclusively on the neck and face, despite being a disseminated infection. Mucosal involvement is observed in two-thirds of patients, especially in the area around the oropharynx.5 Histoplasmosis serology is not typically useful for diagnosis given its low sensitivity in patients with severe immunodeficiency (as in our case, in which it was negative) and the lack of specificity in residents in endemic regions.1
Administering itraconazole at doses of 400mg/day was well tolerated (with no clinical toxicity and liver enzyme normalisation), despite the fact that the potentiated interaction with darunavir can increase the plasma levels of both drugs (www.hiv-druginteractions.org). Thus, it is recommended to monitor itraconazole levels if this technique is available at the hospital.
AuthorshipAll the authors contributed intellectually to this manuscript, meet the authorship conditions and have approved the final version.
Conflict of interestsThe authors declare that they have no conflicts of interest.
Please cite this article as: Sánchez G, Reus S, Rivero E, de Paz F. Lesiones faciales y hepatitis aguda en paciente infectada por el virus de la inmunodeficiencia humana procedente de Paraguay. Enferm Infecc Microbiol Clin. 2017;35:52–53.