Pheochromocytomas are catecholamine-producing neuroendocrine tumors arising mainly from chromaffin cells in adrenal medulla. The first test to be performed in a patient with suspected pheochromocytoma is measurement of catecholamine metabolites (metanephrine and normetanephrine) in blood or 24-h urine, which is more sensitive and specific than measurement of free catecholamines. However, high levels of these metabolites are not always associated to presence of pheochromocytoma, as pharmacokinetic and pharmacodynamic interferences exist with some drugs used in standard clinical practice. We report the case of a 71-year-old female patient monitored at the endocrinology clinic for nodular thyroid disease. Her clinical history included high blood pressure (HBP), dyslipidemia, rheumatoid arthritis, and depression. The patient was being treated with simvastatin 40mg/day, enalapril 5mg/day, prednisone 5mg/day, tramadol as needed, paroxetine 20mg/day, and venlafaxine 150mg/day. At one of the control visits, the patient reported episodes of profuse sweating in the past four months with no associated palpitations. Blood pressure measurements during the episodes were not available, but patient provided home blood pressure measurements of approximately 130/80mmHg. She also reported a change in her bowel habits after the symptoms occurred, with alternating diarrhea and constipation, as well as pain in lower abdomen and left iliac fossa during episodes of sweating. Laboratory tests revealed no significant changes, with normal thyroid function (TSH=1.11mIU/L). Patient had undergone colonoscopy with no significant findings in the prior months. Tests for 5-OH-indoleacetic acid in 24-h urine and catecholamines and metanephrines in 24-h urine were requested to rule out carcinoid syndrome and pheochromocytoma respectively. Levels of 5-OH-indoleacetic acid were normal (5.1mg/24h; normal range: <10mg/24h). Normetanephrine levels in 24-h urine were clearly elevated (1179μg/24h; normal: <444μg/24h), while all other parameters were within the normal range: metanephrine=193μg/24h (normal: <341μg/24h), epinephrine=3.4μg/24h (normal: <20μg/24h), norpinephrine=47μg/24h (normal: <76μg/24h). Repeated measurements taken one month later showed persistent elevation of normetanephrine (1119μg/24h). Normetanephrine increase to almost three times the upper normal limit alerted about a possible pheochromocytoma. Drugs currently received were however reviewed, and a possible drug interaction with measurement of metanephrines was found. Treatment with venlafaxine was withheld for three weeks, and hormone measurements in 24-h urine were repeated. Normetanephrine level was within the normal range in these tests (237μg/24h; normal: <444μg/24h). An adrenal CT scan ruled out pheochromocytoma.
Venlafaxine is a drug commonly used in daily clinical practice for the treatment of major depressive episodes, generalized anxiety disorders, and social phobia. Its main mechanism of action is inhibition of serotonin and norepinephrine uptake without affecting the function of monoamine oxidase (MAO). It is structurally different from tricyclic antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs), or MAO inhibitors (MAOIs). Because of its mechanism of action, venlafaxine may induce elevations of catecholamines and their metabolites in urine and plasma similar to those occurring in pheochromocytoma.1 TCAs should be totally avoided in patients evaluated for pheochromocytoma, because up to 45% false positive results have been reported.2 Life venlafaxine, TCAs inhibit norepinephrine and serotonin reuptake. MAOIs inhibit oxidation of epinephrine and norepinephrine to 3,4-dihydroxyimandelic acid by the MAO enzyme, and therefore significantly increase their levels. SSRIs would be alternative drugs for patients on long-term treatment with other antidepressants during evaluation of pheochromocytoma. They partially inhibit norepinephrine reuptake and are not a significant source of false positive results. Drugs used for the treatment of HBP require special care in patients with suspected pheochromocytoma. Drugs such as phenoxybenzamine block presynaptic α2-adrenergic receptors in adrenal medulla cells without inhibiting norepinephrine release. This drug class is associated to high false positive rates, and should therefore be avoided like TCAs. Other alternatives that may be used for the treatment of HBP include diuretics, ACEIs, or ARBs, which are not associated to interference with catecholamine metabolism.3 β-Blockers are associated to 12.5% of false positive results of elevated plasma metanephrine levels, and may therefore be maintained, and discontinued only in the event of inconclusive results.2 Doxazosin (selective α1-adrenergic blocker), β-blockers, and dihydropyridine calcium channel blockers are associated to false positive results less frequently than phenoxybenzamine and clonidine, sometimes causing elevation of a single metabolite in blood and/or urine, but continue to cause interference. However, they may be continued in some cases. The different guidelines4,5 include in the list of drugs interfering with measurement of catecholamines and their metabolites in urine and blood TCAs, phenoxybenzamine, MAOIs, levodopa, and α-methyldopa.4 However, based on the results found in our patient and in another report,1 we should alert of the interference of venlafaxine with measurement of normetanephrine levels both in 24-h urine and plasma. Before any imaging test is performed, all drugs clearly susceptible of causing interference with biochemical diagnosis of pheochromocytoma should be discontinued (Table 1).4,5 Biochemical tests would have to be repeated at least two weeks after drug discontinuation.1
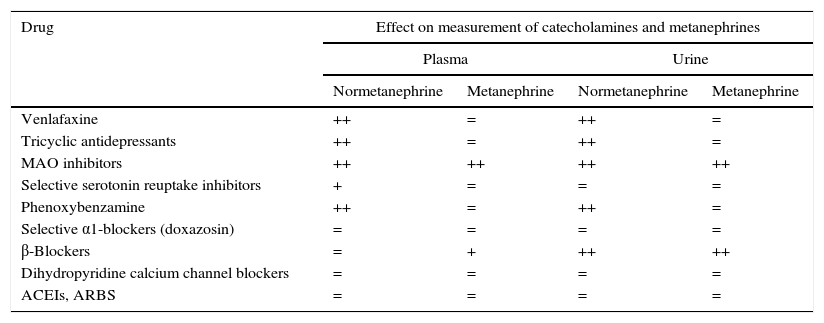
Drug interference with measurement of metanephrine levels in plasma and urine.
| Drug | Effect on measurement of catecholamines and metanephrines | |||
|---|---|---|---|---|
| Plasma | Urine | |||
| Normetanephrine | Metanephrine | Normetanephrine | Metanephrine | |
| Venlafaxine | ++ | = | ++ | = |
| Tricyclic antidepressants | ++ | = | ++ | = |
| MAO inhibitors | ++ | ++ | ++ | ++ |
| Selective serotonin reuptake inhibitors | + | = | = | = |
| Phenoxybenzamine | ++ | = | ++ | = |
| Selective α1-blockers (doxazosin) | = | = | = | = |
| β-Blockers | = | + | ++ | ++ |
| Dihydropyridine calcium channel blockers | = | = | = | = |
| ACEIs, ARBS | = | = | = | = |
+ slight increase; ++ increase; = no interaction.
Please cite this article as: Mañas-Martínez AB, Aragoneses-Calvo A, Matei A, Ojeda-Rodríguez S, García-Durruti P. Interacción farmacológica de venlafaxina en el diagnóstico de feocromocitoma. Endocrinol Nutr. 2016;63:569–570.