To assess whether the benefits seen in nutrition, physical activity and body mass index were maintained at 2 years of completion of the educational intervention.
Material and methodsAn experimental, longitudinal, 4-year, two-arm, parallel study with cluster randomization to assess an intervention program aimed at children in their first year of primary schooling attending schools in the city of Granollers. Intervention consisted of promoting healthy dietary habits and increasing physical activity through the educational pedagogy Investigation, Vision, Action and Change (IVAC), applied over 2 school years (2006–2008). Weight and height of each child were measured in situ, and families self-completed a physical activity survey and the Krece Plus quick test in 2006, 2008, and 2010.
ResultsA greater increase in body mass index was seen in 2010 in children from the control group (2.84±0.22 vs 1.96±0.163kg/m2, <0.001). Prevalence of overweight and obesity increased by 8% and 0.5%, respectively in schoolchildren in the control group, while the intervention group showed a 5.3% increase in prevalence of overweight and a 3.6% decrease in prevalence of obesity. Prevalence of excess weight therefore increased by 8.5% in the control group and by 1.8% in the intervention group.
Reduction in body mass index increase was maintained 2 years after completion of educational intervention regardless of sex, origin, maternal obesity, and educational level of parents.
ConclusionsThese results confirm that school-based interventions may help contain the current increase in childhood obesity.
Determinar si los beneficios observados en alimentación, actividad física e índice de masa corporal se mantenían a los 2 años de haber finalizado la intervención educativa.
Material y métodoEstudio longitudinal experimental de 4 años de duración, aleatorizado por conglomerados, para evaluar un programa de intervención dirigido a escolares de primer curso de educación primaria de las escuelas de Granollers. La intervención consistió en promover hábitos alimentarios saludables y potenciar la actividad física mediante la pedagogía educativa Investigación, Visión, Acción y Cambio (IVAC) aplicada a lo largo de 2 cursos escolares (2006-2008). Se determinó in situ el peso y la talla de cada niño, y las familias autocompletaron una encuesta de actividad física y alimentación en el 2006, 2008 y 2010.
ResultadosEn el 2010 se observó un mayor incremento del índice de masa corporal de los escolares del grupo control (2,84±0,22 vs. 1,96±0,163 kg/m2, p<0,001). La prevalencia de escolares con sobrepeso y obesidad aumentó respectivamente en un 8 y un 0,5% en el grupo control, mientras que en el grupo intervención se incrementó la prevalencia de sobrepeso (5,3%) y se redujo la de obesidad (3,6%). La prevalencia de escolares con exceso de peso aumentó en un 8,5% en el grupo control y en un 1,8% en el de intervención. A los 2 años de finalizar la intervención educativa se mantuvo la reducción del incremento del índice de masa corporal, independientemente del sexo, la procedencia, la obesidad materna y el nivel de estudios de los progenitores.
ConclusionesLa intervención educativa mediante el empleo del método pedagógico IVAC ayuda a contener el actual incremento de obesidad infantil.
Obesity has become in recent decades a public health problem of epidemic proportions, affecting adults, adolescents, and children.1,2 Childhood obesity is associated with lipid metabolism disorders, high blood pressure, platelet aggregation, and hyperinsulinism, as well as with an increased risk of obesity in adult age.1,2
The efficacy of obesity management is low in both adults and children or adolescents.2 Obesity has been related to a high energy intake associated with the acquisition of sedentary lifestyle habits, hence the interest in implementing preventive schemes intended to increase physical activity and improve nutrition.3
School is an appropriate place for intervention in order to achieve healthy lifestyles because children stay there for almost half of their waking hours and many of them take two meals daily (breakfast and lunch) there. For this reason, many interventional studies have been undertaken at school in order to modify the dietary and physical activity habits of schoolchildren and thus decrease the incidence of childhood obesity.3 There are, however, few studies assessing changes in dietary habits, physical activity, and body mass index (BMI) some years after the intervention has been completed.4–7
The Avall study was a two-year educational intervention, using Research, Vision, Action, and Change (IVAC) methodology, on dietary habits and physical activity in first year schoolchildren. Its aim was to assess its impact on BMI.8 Once intervention was shown to be effective for reducing weight increase, the objective was to assess whether the effect of an intervention on dietary and physical activity habits and BMI in a school age population had been maintained two years after the end of the interventional study.
Subjects and methodStudy populationThe Avall project (Clinical Trial Government registry number: NCT01156805) has previously been reported in detail.8 It was approved by the ethics committee of the Hospital General de Granollers, and was supported by the Department of Education and Health of the Catalonian Government and the principals of all the schools concerned. In September 2008, the schools provided the identity, sex, and birth date of all first year schoolchildren, and their families were asked to provide written consent for participation in the study. The participants were children born in 2000 attending the 10 public schools and six state-assisted schools in the town of Granollers, located in the Vallés Oriental area of the province of Barcelona. Among the 704 children who started primary education in the 2006–2007 school year, the families of 598 (84.9%) agreed to their participation in the study, but data were collected from 566 children, or 80.4% of the sample.9 At the end of intervention, anthropometric variables were collected from all 704 schoolchildren (72.3%), 237 (78.8%) in the control group and 272 (72.7%) in the intervention group.
DesignThis was a cluster-randomized, parallel, two-arm, experimental, longitudinal, four-year study to assess an intervention scheme in first year schoolchildren (aged 5–6 years) attending schools in the city of Granollers. Two years after the completion of this intervention, in September 2010, questionnaires on dietary habits and physical activity were sent to each school. In October 2010, the same nurses in charge of the project went to each school to perform anthropometric measurements and to collect the questionnaires.8
InterventionIntervention consisted of the promotion of healthy dietary habits and physical activity using IVAC educational pedagogy for two consecutive school years (2006–2007 and 2007–2008). The IVAC method is used in health strategies because the perceptions and knowledge elaborated by schoolchildren are directed towards change, so that they make their own decisions based on their concepts of health, determination of priorities, and change. It is schoolchildren who investigate and reflect on how lifestyle, environment, and society affect their health. Teachers act as moderators in conversations between schoolchildren and help them develop the skills they need to be able to change these conditions. This method allows for the incorporation of educational activities related to healthy habits into any subject matter. At study start, a group of educators specializing in community projects trained teachers in the intervention group in the above methodology. During the two years of intervention, the research team, teachers, and specialists attended six meetings in order to gather information on the activities performed in each class and to plan further action.
Study variablesThe primary study variable was the change in BMI in schoolchildren from the intervention group as compared to the control group. The secondary variables assessed included changes in healthy lifestyle, dietary, and physical activity habits.
Weight, height, and BMI were measured as previously reported.
Dietary habits were evaluated using a weekly consumption frequency questionnaire and the KrecePlus test. Children were also asked if they walked to school, the time they spent watching television, video, or DVD (which was categorized as “1–2h daily” and “more the 2h daily”), and if they performed physical activity outside school hours (which was categorized as “Yes”, “No”, and “Sometimes”).
BMI was categorized as low weight, normal weight, overweight, and obesity according to the cut-off points proposed by the International Obesity Task Force.10 Age was categorized by proximity to the cut-off points proposed in the reference tables by age (10, 10.5, and 11 years). The BMI of each child was classified based on sex and age.
The weight status of the parents was classified based on their BMI, using Garrow criteria.
Statistical analysisQualitative variables are reported as absolute frequencies and percentages, and continuous variables as mean and standard deviation, after verifying that they followed a normal distribution.
Qualitative variables were analyzed using a Pearson's Chi-square test or a Fisher's exact test, and a McNemar test for paired data. Quantitative variables were analyzed using a Student's t test for independent data.
A value of p<0.05 was considered statistically significant in all tests.
A repeated measures analysis of variance based on a multivariate generalized linear model was performed to assess the effect of intervention on BMI changes in schoolchildren. This analysis tested whether any variable, mainly those that were unbalanced at baseline, including baseline BMI, changed the effect seen in the intervention.
SPSS 18.0 for Windows software was used for all statistical tests.
ResultsFull anthropometric data were collected in 2010 from 426 (83.7%) of the 509 schoolchildren participating in the study from whom data had been collected in 2006 and 2008. Of these, 201 children (84.8%) were in the control group and 225 (82.7%) in the intervention group.
A total of 178 schoolchildren from the control group (89.9%) and 216 from the intervention group (96.4%) completed the questionnaires. Of these, 47.5% and 48.2%, respectively, were girls.
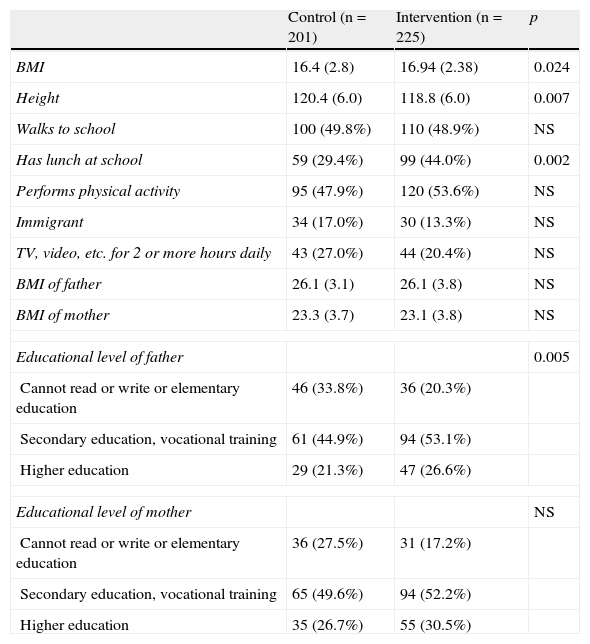
At study start on September 2006, mean age in both groups was 6.03±0.3 years. At baseline, BMI was higher in the intervention as compared to the control group (Table 1). Boys in the control and intervention groups had similar BMIs (16.6±2.7 and 16.9±2.1kg/m2, respectively), while girls in the control group had a lower mean BMI as compared to the intervention group (16.2±2.9kg/m2 vs 17.0±2.7kg/m2 respectively, p=0.024). Immigrant rates were similar in both groups, and no significant differences were found regarding whether or not children walked to school (Table 1) or performed physical activity out of school, the daily time they spent watching “television, videos, DVDs, or similar activities”, the mean BMI of parents, and the educational level of the mother. In the intervention group, a greater proportion of parents had an upper educational level and a greater proportion of schoolchildren had lunch at the school.
Baseline characteristics of both groups.
| Control (n=201) | Intervention (n=225) | p | |
| BMI | 16.4 (2.8) | 16.94 (2.38) | 0.024 |
| Height | 120.4 (6.0) | 118.8 (6.0) | 0.007 |
| Walks to school | 100 (49.8%) | 110 (48.9%) | NS |
| Has lunch at school | 59 (29.4%) | 99 (44.0%) | 0.002 |
| Performs physical activity | 95 (47.9%) | 120 (53.6%) | NS |
| Immigrant | 34 (17.0%) | 30 (13.3%) | NS |
| TV, video, etc. for 2 or more hours daily | 43 (27.0%) | 44 (20.4%) | NS |
| BMI of father | 26.1 (3.1) | 26.1 (3.8) | NS |
| BMI of mother | 23.3 (3.7) | 23.1 (3.8) | NS |
| Educational level of father | 0.005 | ||
| Cannot read or write or elementary education | 46 (33.8%) | 36 (20.3%) | |
| Secondary education, vocational training | 61 (44.9%) | 94 (53.1%) | |
| Higher education | 29 (21.3%) | 47 (26.6%) | |
| Educational level of mother | NS | ||
| Cannot read or write or elementary education | 36 (27.5%) | 31 (17.2%) | |
| Secondary education, vocational training | 65 (49.6%) | 94 (52.2%) | |
| Higher education | 35 (26.7%) | 55 (30.5%) | |
BMI: body mass index.
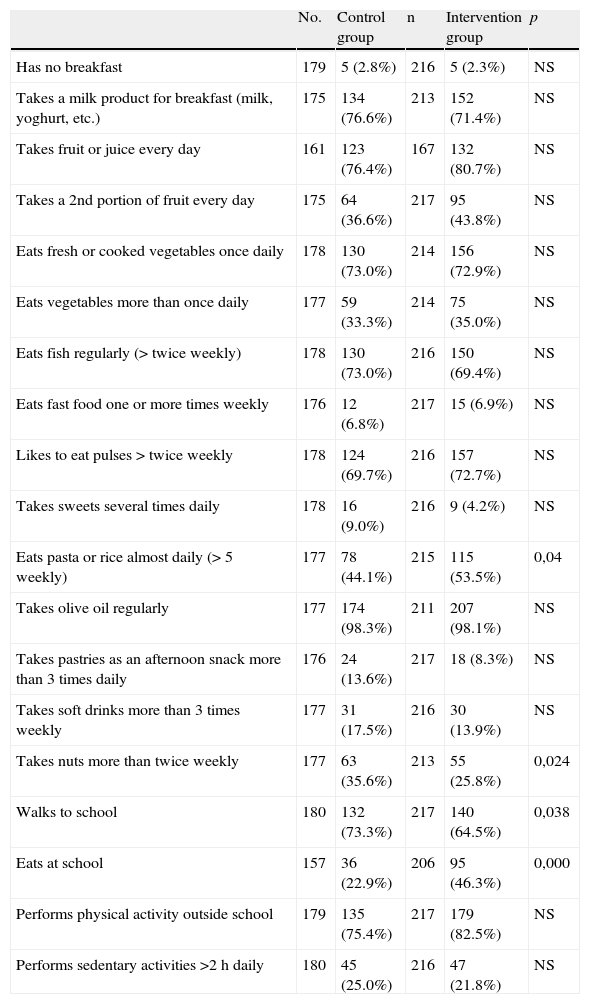
Two years after the educational intervention was completed, dietary habits were similar in both groups, except that a lower proportion of children in the control group ate almost no pasta or rice daily, consumed nuts more frequently, and showed a trend to a higher consumption of pastries as afternoon snacks (p=0.062) (Table 2). A higher proportion of control schoolchildren walked to school and had no lunch there, while a trend was seen for a greater proportion of children in the intervention group to perform physical activity outside the school (p=0.055) (Table 2). There were no differences in the daily time of sedentary activity between the two groups.
Results of the KrecePlus test.
| No. | Control group | n | Intervention group | p | |
| Has no breakfast | 179 | 5 (2.8%) | 216 | 5 (2.3%) | NS |
| Takes a milk product for breakfast (milk, yoghurt, etc.) | 175 | 134 (76.6%) | 213 | 152 (71.4%) | NS |
| Takes fruit or juice every day | 161 | 123 (76.4%) | 167 | 132 (80.7%) | NS |
| Takes a 2nd portion of fruit every day | 175 | 64 (36.6%) | 217 | 95 (43.8%) | NS |
| Eats fresh or cooked vegetables once daily | 178 | 130 (73.0%) | 214 | 156 (72.9%) | NS |
| Eats vegetables more than once daily | 177 | 59 (33.3%) | 214 | 75 (35.0%) | NS |
| Eats fish regularly (> twice weekly) | 178 | 130 (73.0%) | 216 | 150 (69.4%) | NS |
| Eats fast food one or more times weekly | 176 | 12 (6.8%) | 217 | 15 (6.9%) | NS |
| Likes to eat pulses>twice weekly | 178 | 124 (69.7%) | 216 | 157 (72.7%) | NS |
| Takes sweets several times daily | 178 | 16 (9.0%) | 216 | 9 (4.2%) | NS |
| Eats pasta or rice almost daily (> 5 weekly) | 177 | 78 (44.1%) | 215 | 115 (53.5%) | 0,04 |
| Takes olive oil regularly | 177 | 174 (98.3%) | 211 | 207 (98.1%) | NS |
| Takes pastries as an afternoon snack more than 3 times daily | 176 | 24 (13.6%) | 217 | 18 (8.3%) | NS |
| Takes soft drinks more than 3 times weekly | 177 | 31 (17.5%) | 216 | 30 (13.9%) | NS |
| Takes nuts more than twice weekly | 177 | 63 (35.6%) | 213 | 55 (25.8%) | 0,024 |
| Walks to school | 180 | 132 (73.3%) | 217 | 140 (64.5%) | 0,038 |
| Eats at school | 157 | 36 (22.9%) | 206 | 95 (46.3%) | 0,000 |
| Performs physical activity outside school | 179 | 135 (75.4%) | 217 | 179 (82.5%) | NS |
| Performs sedentary activities >2h daily | 180 | 45 (25.0%) | 216 | 47 (21.8%) | NS |
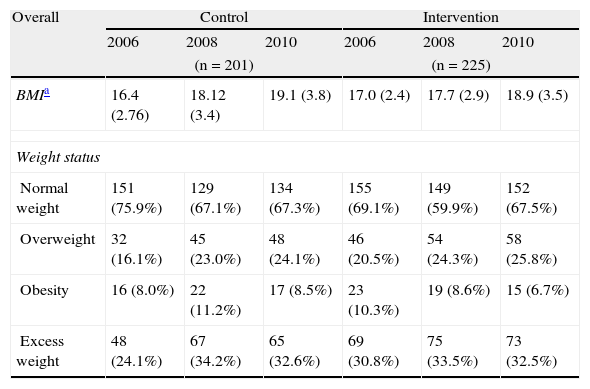
Table 1 shows changes in mean BMI in both groups. Reduction in BMI increase was seen at the end of the educational intervention, and this difference persisted in the years following the completion of the intervention.
The effect of the intervention seen in the second year of follow-up had been maintained two years after the end of the intervention, with a greater increase in BMI seen in the control group (2.73±2.07 vs 1.93±2.03kg/m2, p<0.001). This effect was shown in both boys (2.93±2.06 vs 1.96±2.12, p<0.001) and girls (2.48±2.06 vs 1.90±1.94, p=0.03).
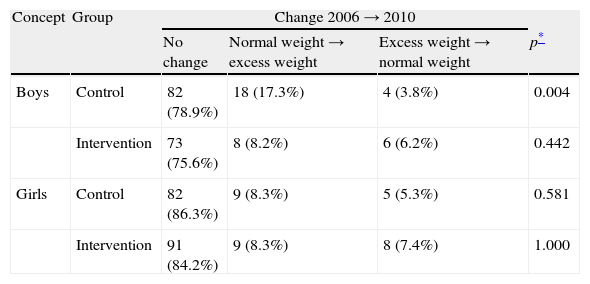
The prevalence of schoolchildren with overweight and obesity increased by 8% and 0.5%, respectively in the control group, while in the intervention group the prevalence of overweight increased by 5.3%, while obesity prevalence decreased by 3.6% (Table 3). The prevalence of overweight and obesity increased in girls from the control group (2.1% and 1.1%, respectively), while girls in the intervention group showed an increased prevalence of overweight (2.5%) but a decreased prevalence of obesity (3.8%). Control group children showed increased overweight (13.5%) but no increase in obesity, while the prevalence of overweight increased (7.8%) and obesity prevalence decreased (3.5%) in the intervention group. The prevalence of schoolchildren with excess weight (overweight and obesity) increased by 8.5% in the control group and by 1.7% in the intervention group. The prevalence of girls with excess weight increased by 3.2% in the control group and did not change in the intervention group (Table 3), while this prevalence increased in boys from both groups (13.5% and 4.3%, respectively). Control group boys showed a significant impairment in their weight status (Table 4).
Changes over time in weight status.
| Overall | Control | Intervention | ||||
| 2006 | 2008 | 2010 | 2006 | 2008 | 2010 | |
| (n=201) | (n=225) | |||||
| BMIa | 16.4 (2.76) | 18.12 (3.4) | 19.1 (3.8) | 17.0 (2.4) | 17.7 (2.9) | 18.9 (3.5) |
| Weight status | ||||||
| Normal weight | 151 (75.9%) | 129 (67.1%) | 134 (67.3%) | 155 (69.1%) | 149 (59.9%) | 152 (67.5%) |
| Overweight | 32 (16.1%) | 45 (23.0%) | 48 (24.1%) | 46 (20.5%) | 54 (24.3%) | 58 (25.8%) |
| Obesity | 16 (8.0%) | 22 (11.2%) | 17 (8.5%) | 23 (10.3%) | 19 (8.6%) | 15 (6.7%) |
| Excess weight | 48 (24.1%) | 67 (34.2%) | 65 (32.6%) | 69 (30.8%) | 75 (33.5%) | 73 (32.5%) |
| Girls | (n=95) | (n=109) | ||||
| BMIa | 16.5 (2.9) | 17.9 (3.6) | 18.7 (4.1) | 17.0 (2.7) | 17.8 (3.1) | 18.9 (3.8) |
| Weight status | ||||||
| Normal weight | 72 (75.8%) | 64 (69.5%) | 69 (72.6%) | 67 (62.0%) | 68 (63.6%) | 69 (63.3%) |
| Overweight | 15 (15.8%) | 19 (20.7%) | 17 (17.9%) | 29 (26.9%) | 30 (28.0%) | 32 (29.4%) |
| Obesity | 8 (8.4%) | 9 (9.8%) | 9 (9.5%) | 12 (11.1%) | 9 (8.4%) | 8 (7.3%) |
| Excess weight | 23 (24.2%) | 28 (30.5%) | 26 (27.4%) | 41 (37.0%) | 39 (36.4%) | 40 (36.9%) |
| Boys | (n=106) | (n=116) | ||||
| BMIa | 16.6 (2.7) | 18.4 (3.1) | 19.5 (3.4) | 16.9 (2.1) | 17.7 (2.6) | 18.8 (3.2) |
| Weight status | ||||||
| Normal weight | 79 (76.0%) | 65 (62.5%) | 65 (62.5%) | 88 (75.9%) | 81 (70.4%) | 83 (71.6%) |
| Overweight | 17 (16.3%) | 26 (25.0%) | 31 (29.8%) | 17 (14.6%) | 24 (20.9%) | 26 (22.4%) |
| Obesity | 8 (7.7%) | 13 (12.5%) | 8 (7.7%) | 11 (9.5%) | 10 (8.7%) | 7 (6.0%) |
| Excess weight | 25 (24.0%) | 39 (37.5%) | 39 (37.5%) | 28 (24.1%) | 34 (29.6%) | 33 (28.4%) |
BMI: body mass index.
Change over time in weight status two years after the end of intervention.
| Concept | Group | Change 2006→2010 | |||
| No change | Normal weight→excess weight | Excess weight→normal weight | p* | ||
| Boys | Control | 82 (78.9%) | 18 (17.3%) | 4 (3.8%) | 0.004 |
| Intervention | 73 (75.6%) | 8 (8.2%) | 6 (6.2%) | 0.442 | |
| Girls | Control | 82 (86.3%) | 9 (8.3%) | 5 (5.3%) | 0.581 |
| Intervention | 91 (84.2%) | 9 (8.3%) | 8 (7.4%) | 1.000 | |
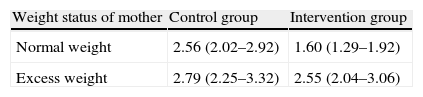
A multivariate repeated measures analysis of variance (generalized linear model) was performed to test the impact of sex and factors previously shown to be associated with overweight, such as parent obesity and educational level and potential second degree interactions between them. Finally, mother obesity was found to be the only factor requiring adjustment. The effect of intervention persisted in the resulting adjusted model (p<0.001, Table 5), and obesity/overweight in the mothers was also seen to condition a change to higher BMI values in both their control and obese children (p=0.006). Increased BMI values (p=0.043) were seen in children who had lunch at school, but this effect disappeared after adjustment for excess weight in the mother (p=0.138).
Mean BMI increase and confidence interval from 2006 to 2010.
| Weight status of mother | Control group | Intervention group |
| Normal weight | 2.56 (2.02–2.92) | 1.60 (1.29–1.92) |
| Excess weight | 2.79 (2.25–3.32) | 2.55 (2.04–3.06) |
Multivariate analysis of variance (generalized linear model) for paired data showed an effect of intervention (p<0.001), in the sense that BMI increase at two years of follow-up was lower in the intervention than in the control group, and this effect persisted despite the fact that obesity/overweight of the mother conditioned a trend in her children to higher BMI values in both controls and obese (p=0.006).
This study was the first to analyze in our environment the persistence of changes in dietary habits and physical activity and their impact on BMI two years after the completion of an educational intervention in schoolchildren.
Only a few studies are available on this subject, including three long-term studies.7,11,12 One of these, conducted in two towns from Northern France, monitored for 12 years the effect of three consecutive school-based interventions for preventing childhood obesity (the first period [1992–1997] focused on nutritional education at school, the second period [1997–2002] was an observational, longitudinal study on factors determining weight changes, and the third period [2002–2007] focused on the practice of physical activity and healthy nutrition through a number of community-based activities).11 From 2002 to 2004, a decreased prevalence of overweight was seen in schoolchildren, especially girls. The authors suggested that interventions may have synergistic effects on the prevalence of overweight, and that the trend to weight increase may be reversed through community-based actions. The other study, the so-called “Know Your Body” program, was conducted in Crete and was intended to prevent cardiovascular disease in schoolchildren.12 This intervention was performed at curriculum level and consisted of 13–17h class hours per school year devoted to healthy habits during the first to sixth years of primary school. A lower increase in BMI and a reduction in the risk factors for chronic diseases as compared to a control group were seen at 10 years of the implementation of this program. The third study was an obesity prevention study conducted in Kiel (KOPS), Germany.6,7 The results of the KOPS study, including interventions aimed at schoolchildren and their families, after four and eight years of follow-up revealed similar BMI increases in the intervention and control groups. However, the prevalence of excess weight was decreased in schoolchildren with a high socioeconomic level.
These studies had designs different from our study, because the interventions were performed at curriculum level and for more school years,12 there were several consecutive interventions during the monitoring period,11 healthy messages were given to both children and their parents and teachers, and a dietician gave six classes on nutrition followed by 20min of physical activity during playtime in the second part of the first school year.6,7
Other studies such as the DUTCH, CHOPPS, and APPLE studies4,5,13 had no such long-term evaluation.
The CHOPPS study, conducted in the United Kingdom, included a group of schoolchildren similar to those participating in our study. Intervention focused on the reduction of soft drink consumption and on inculcating in them healthy habits during a school year, at the end of which a significant reduction was seen in the prevalence of overweight and obesity. However, this improvement was not maintained at three years.5
The DUTCH study, conducted in teenagers, included 11 lessons on biology and physical education in a school year curriculum. The effect of intervention was assessed one year after its completion. A decrease in the sum of skinfolds was seen in girls, but not in boys.13 The authors suggested that the lack of impact on BMI was due to the fact that skinfolds are more sensitive to changes in fat mass in teenagers.
The design of the APPLE study was more similar to the one reported here, because it included a two-year educational intervention on diet and physical activity in schoolchildren of a similar age, and assessed its impact on BMI two years after the end of the intervention.4 While baseline data showed that the prevalence of overweight was lower in the intervention than in the control group and did not change during the study, a BMI z-score reduction was seen in the intervention group at two years and persisted for two years. These results agree with those found in our study. However, unlike in the APPLE study, mean baseline BMI in our study was lower in the control than in the intervention group, and BMI increase was higher in the control than in the intervention group. This effect was seen in both girls and boys. Analysis of change in weight status only showed a worsening in control group boys, while no changes were found in boys from the intervention group or in girls.
Certain childhood periods are crucial for obesity prevention and have been seen to be associated with marked changes in adiposity. These include the first year of life, from three to seven years of age, and puberty.2 The early occurrence of adiposity is associated with a greater risk of obesity during puberty and adolescence.14 At baseline, girls in the intervention group had a higher mean BMI as compared to those in the control group and a higher prevalence of excess weight (37% vs 24%). Despite the fact that a high baseline BMI represents a risk factor,2,6,14 intervention was able to reduce the increasing trend to obesity.
On the other hand, in developed countries puberty occurs between eight and 16 years of age.15 In the 20th century, improvements in the socioeconomic and health conditions of the populations led to an earlier start of puberty in girls.1,15,16 In addition, childhood obesity is associated with the earlier occurrence of puberty and menarche in girls.1,15,16 Girls experience a greater increase in fat mass during childhood and puberty, and it has also been noted that the greater the obesity, the greater the increase in fat mass during puberty.1 While pubertal state was not assessed in schoolchildren, the fact that girls in the intervention group had at study start a significantly higher mean baseline BMI and a greater prevalence of excess weight as compared to those in the control group may explain the differences found between both sexes in the intervention group.
This study showed that the improvement in dietary habits seen just after educational intervention was not maintained over time. Few studies based on school-based interventions have analyzed changes in dietary habits years after the completion of the intervention, and few of them have found a persistence of healthy habits acquired during the intervention.4,7 In the reported study, the lower BMI increase seen was not associated with either the maintenance or the improvement of the dietary habits acquired at the end of the educational intervention. A decreased consumption of farinaceous food and a higher consumption of nuts and pastry were only seen in the control group. The reason for this may be that the methodology used had no adequate precision for measuring such changes and/or that small changes have an additive effect in weight increase prevention.17
Contrary to previous reports,8 having lunch at school was not a determinant for BMI increase when analyzed together with the presence or absence of excess weight in the mother. This could be due to chance or to an inadequate sample size in our study.
As previously reported, a marked excess weight in the parents, particularly the mother, low socioeconomic and cultural levels, and a high baseline BMI of the child are risk factors for overweight, more relevant in boys than in girls.2,6,14 In the reported study, the effect of educational intervention was able to maintain the prevalence of excess weight in boys, as those from the control group had a greater increase in BMI and an impaired weight status. As shown in other studies, interventions are not always equally effective in both sexes.13,18
Study limitationsPercent losses were high, but the proportion was similar to that reported by other school-based intervention studies,5–7 and losses were similar in both groups. The reasons included change in school, relocation, voluntary withdrawal of the schoolboy/girl, and non-attendance at school on the day of weight and height control.
In this study, the intervention was similarly effective in the immigrant population. This may be explained by the low number of children in this group and/or by the wide race diversity. The results obtained at the end of the intervention were locally disseminated. It is difficult to assess how such an initiative may have influenced dietary and physical activity habits in the control group and, thus, changes in BMI. Such an effect may, however, have had an impact in the intervention group, and in this analysis the intervention group continued to show a lower BMI increase as compared to the control group. As regards physical activity, although schoolchildren in the control group walked to school, those in the intervention group performed physical activity outside school time. The physical activity involved in walking to school quite probably has a much lesser impact upon daily energy expenditure than out-of-school physical activities. The main reason for this is that the rules for access to public and state-assisted schools are mainly based on the proximity of the family home to the school.
The ineffectiveness of interventions in some groups of schoolchildren and increased childhood obesity have led to a reconsideration of strategy planning and evaluation. The community-based program planned in the IDEFICS project to be conducted in Europe is one result of such a reconsideration.19
Parents identify many barriers preventing the adoption of recommendations to prevent childhood obesity, including family preferences, resistance to change, and economic issues. Intervention programs should consider family and child priorities, as well as economic factors and measures to overcome the most relevant obstacles during the development of the program.20 The current setting of economic crisis may have contributed to a greater resistance to some changes, particularly as regards the performance of physical activity and the acquisition of some healthy foods. However, the educational methodology used (IVAC) in which the schoolchild him/herself decides what he/she can do for his/her health may be more effective than inclusion in the curriculum of classes aimed at teaching healthy habits.
This methodology, to the extent that it stimulates reflection on the part of people both on themselves and on their environment, is therefore a good way of encouraging people to become more interested in their habits and more willing to propose changes and to assume them as their own.
ConclusionsIn this study, mean BMI increase was lower in the intervention than in the control group in both sexes, regardless of the origin of the schoolchild, the educational level of the parents, and excess weight in the mother. This resulted in a lesser increase in the prevalence of schoolchildren with overweight and in a decreased obesity rate. Thus, educational intervention using IVAC methodology was able to contain the increasing trend to excess weight in schoolchildren in this study two years after the end of the intervention. Further long-term studies are, however, required to assess whether this two-year intervention using IVAC educational methodology continues to be effective and/or should be maintained for a longer period or be regularly repeated.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Llargués E, et al. Evaluación a medio plazo de una intervención educativa en hábitos alimentarios y de actividad física en escolares: estudio Avall 2. Endocrinol Nutr. 2012;59:288–95.