La banda gástrica ajustable es una técnica afianzada en el mundo en el tratamiento de la obesidad mórbida. En España, las cifras de pacientes intervenidos de banda gástrica distan mucho de las cifras mundiales, habiéndose alegado un alto número de reintervenciones.
Material y métodosEn el año 2001 iniciamos,un programa de tratamiento quirúrgico de la obesidad mediante la implantación de banda gástrica ajustable. Paralelamente, desarrollamos un sistema exhaustivo de seguimiento para evitar complicaciones y mejorar los resultados.
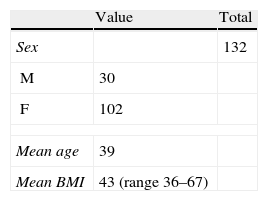
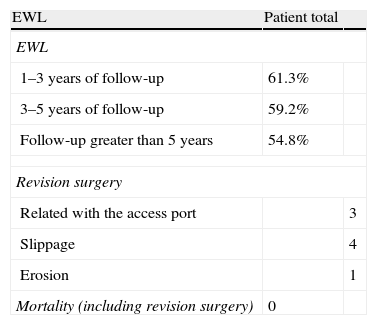
ResultadosDesde el año 2001 hasta el 2011 hemos intervenido un total de 132 pacientes, 102 mujeres y 30 hombres, con una edad media de 39 años y un índice de masa corporal medio de 43. El seguimiento fue superior a 5 años en 61 pacientes; en el resto, el seguimiento medio fue de 44, 4 meses. La mortalidad y complicaciones graves fue 0. Ocho pacientes requirieron cirugía de revisión (6,06%), 3 por complicaciones relacionadas con el reservorio, 4 por deslizamiento y una por erosión. Tres deslizamientos se convirtieron a otra técnica y otro se resolvió con colocación de una nueva banda de tipo Lap Band. El porcentaje de sobrepeso perdido medio se mantuvo en los pacientes con un seguimiento superior a los 5 años en 54,8%.
ConclusionesLos resultados de nuestra serie son superponibles a los publicados en la literatura mundial en nuestro medio y demuestran que, reproduciendo el seguimiento realizado, la banda gástrica es un método eficaz y seguro para el control del peso en los pacientes con obesidad mórbida también en España.
Adjustable gastric banding is a surgical technique used all over the world for the treatment of morbid obesity. In Spain, the number of patients treated with adjustable gastric banding is far lower than the average worldwide average. A number of reasons have been put forward to explain this difference.
Materials and methodsA program of bariatric surgery by means of implantation of an adjustable gastric banding was started in 2001, together with a dedicated follow-up protocol in order to prevent complications and improve results.
ResultsA total of 132 patients were operated on between 2001 and 2011. The mean age of the 102 female and 30 male patients was 39 years, and the mean body mass index was 43. Follow-up was longer than 5 years in 61 patients, while the mean follow-up in the rest was 44.4 months. There was no mortality or severe morbidity. Eight patients (6.06%) underwent reoperation, 3 of them for complications related to the reservoir, 4 for slipping of the band, and one for erosion. One slipped band was removed, and a new one (of the Lap Band type) was inserted. Three slipping bands were converted to other techniques. The percentage excessive body weight loss was maintained in 54.8% of the patients followed-up for longer than 5 years.
ConclusionsThe results of our series are comparable to those reported in the literature and show that, provided that a close follow-up, like that performed by most groups, is implemented, adjustable gastric banding can also be a safe and effective bariatric surgery technique in our country.
Obesity is an epidemiological health problem with an exponential growth, parallel to the development of our country.1 Just as in other European countries and the United States, the rate of obesity in Spain, especially that of morbid obesity, is becoming alarming. Consequently, surgeons have seen how obesity surgery has gone from an anecdotal procedure, performed by only a few experts, to being a common intervention in our surgery departments.2 Unfortunately, there is no perfect surgical technique for these patients. Their physical conditions, together with the high risk of these patients derived from their metabolic and proinflammatory state can turn any technique into a highly difficult intervention with an increased number of serious complications and mortality.3
For these reasons, surgeons around the world have been searching for techniques to reduce these risks. Such is the case of adjustable gastric banding, implemented in humans for the first time by Belachew and Legrand almost 20 years ago.4,5 The use of these bands has become more common in the United States and in Europe in recent years, and over half of bariatric surgery procedures are gastric band placements.2,6 Adjustable gastric banding is a technique with no mortality and only a few serious complications, unlike most other techniques used in obesity surgery.7
In Spain, however, to date we have not reproduced the outcomes published in the international literature. In most Spanish scientific forums, the effectiveness and even the safety of these devices have been questioned, and there have been reports of a high number of reinterventions for conversion to other techniques due to either failure of the procedure or long-term complications. Most of these poor results have not been published, although there are Spanish publications about the limited number of gastric band procedures performed.8
Today, now that in Spain we are starting to introduce gastric bands in our therapeutic arsenal for the treatment of morbid obesity,9 we still ask ourselves why gastric banding has met with such failure in our setting. In this paper, we present the results from the follow-up of 132 patients who have undergone this procedure in the last 10 years in Spain, with morbidity, mortality and efficacy results that are comparable to the data published internationally.
ObjectiveBy means of a retrospective analysis of our patients, our objective is to demonstrate that if we reproduce not only the technique but also the same follow-up method as other groups in Europe, we can achieve the same results and the same proportion of revision surgery.
Materials and MethodsIn 2001, we initiated a treatment program for morbid obesity using adjustable gastric bands. This program was started in order to reduce the risks of the interventions and mortality in an attempt at reproducing what authors such as Chevalier had published up until that time.7 The program was started at a private hospital and afterwards at a public hospital; the interventions in both centers were done by the same surgical team and with the same surgical and follow-up protocols.
Surgical TechniqueWe placed the adjustable gastric bands laparoscopically while maintaining pressures between 14 and 16mm Hg. Four 10mm trocars were used (Fig. 1) and the hiatus was approached using a pars flaccida technique with minimal posterior and angle of Hiss dissection. Later, the stomach was sutured to the gastric pouch using interrupted silk sutures in order to avoid anterior slippage. The port of access to the band was placed in the interior thoracic region and set in place with 4 polypropylene stitches. This technique has not varied since its introduction, except for the area of the port placement, which in the first few patients was in the upper abdomen (Fig. 2).
Patient SelectionIn our group, as in others,10,11 we have made no distinctions according to BMI: all the patients who met criteria for bariatric surgery and had given their consent underwent this procedure.
Perioperative ProtocolThe patients underwent surgery and were discharged from hospital when they were able to ingest liquids and had spontaneous urination. Most patients remained in the hospital for less than 24h: those who underwent surgery in the morning were discharged in the evening, and those who had surgery in the afternoon were discharged the following morning.
Follow-up ProtocolParallel to the procedure itself, we implemented a thorough follow-up protocol similar to that described by European groups and later by American and Australian groups.11 Office visits were scheduled for: 10, 21 and 28 days after surgery; 2, 3, 6 and 12 months after surgery; twice during the following year, and once a year thereafter. During these visits, we analyzed in detail the patients’ eating habits while providing appropriate nutritional education in order for the bands to induce satiety through the vagal afferent nerves, as recently reported by O’Brien.11–13 Band adjustments were done in the office during scheduled visits when the patients required them. We also used a telephone contact system for the patients to call us and for us to call them when necessary due to either poor treatment compliance or poor adaptation to the band.
Data Collection and AnalysisDuring the years of the study, we collected patient data for sociodemographics, complications, mortality and weight loss. Those patients who we had not seen in our consultation the last year were contacted by telephone in order to complete their data. We were not able to contact 9 out of the 132 subjects, but we analyzed their data up until the last consultation and have included them in the follow-up until the date of the last visit. We have analyzed the situation of our patients during a 10-year period, from 2001 until 2011, and we have compared this with the international literature.
ResultsBetween 2001 and 2011, we operated on a total of 132 patients: 102 women and 30 men (Table 1). Mean age was 39 and mean body mass index (BMI) was 43 (range 36–67). In 61 patients, follow-up was longer than 5 years; the mean follow-up of the remainder was 44.4 months. All patients had a follow-up longer than 1 year. All patients were contacted by phone to complete any missing follow-up data before their analysis. Six patients were impossible to contact and were therefore withdrawn from the study. The most frequent comorbidity was dyslipidemia, which was present in more than 50% of our patients.
The results are shown in Table 2. There was no mortality or serious complications in our series, except for one patient with a BMI of 67 who required 3 days of postoperative care in the ICU due to difficulties that arose during extubation related to restrictive lung disease caused by obesity. In the remaining patients, the mean hospital stay was less than 1 day, since all patients were admitted on the day of the procedure and discharged either that same afternoon or the following morning.
Most of the patients presented isolated vomiting episodes at some time during the follow-up period, which were generally associated with rapid or inappropriate eating. The incidence of more than 1 vomiting episode a week was higher in patients with small-diameter, high-pressure bands. With the appearance of wider, low-pressure bands, this adverse effect disappeared in our patients. Only 2 patients with this type of band had one or more vomiting episodes per week, both of whom had band slippage. There was no vomiting in the immediate postoperative period.
Eight patients required revision surgery (6.06%). Out of these 8, 3 were resolved with surgery under local anesthesia due to complications related with the access port; all 3 had appeared within the first 2 years of follow-up. Two of these 3 patients had an infection of the port that required its removal until the wound had healed completely, followed by the later implantation of a new port, after which no new signs of infection or complications appeared. The third patient had a leak in the system that required revision under local anesthesia, at which time the leak was discovered in the tube connecting the access port with the band; the leak was in a subcutaneous location, caused by accidental puncture during band adjustments because the tube was on top of the access port. This problem was resolved by cutting the segment of the tube that had the leak and reconnecting it with a metallic connector. After this complication, we started to situate the entire tube of the system intraabdominally.
The other 5 patients who required revision surgery presented band slippage in 4 cases (at 11, 14, 19 and 25 months of follow-up) and band erosion in one (after 2 years of follow-up).
The 4 slippages were resolved: in one case, the slipped band was removed and replaced with a new Lap Band (Fig. 3), with another posterior tunnelization; the other 3 cases were resolved by reconverting to another technique (2 gastric bypass and 1 biliopancreatic bypass). The 2 conversions to gastric bypass presented technical difficulties fundamentally with the release of the gastric pouch suture and in creating the posterior tunnel in order to perform the gastric pouch of the bypass. Moreover, although these 2 patients did not present postoperative complications, these anastomoses were considered to be a risk due to the poor local inflammatory conditions. For this reason, the last conversion was to a biliopancreatic bypass, which allowed us to avoid the hiatus and safely cut and create a gastric anastomosis in an area that had not been previously manipulated. Furthermore, in this third patient the withdrawal of the band was simple as it was not necessary to undo the previous gastric pouch suture. By simply cutting and pulling, it was easily extracted. The 4 patients with slippage, both those converted to another technique as well as the band replacement, were operated on laparoscopically.
The patient with gastric band erosion presented symptoms of food intolerance and the erosion was observed with endoscopy. The patient underwent laparoscopy under general anesthesia, the band was extracted and the gastric defect sutured. We did not carry out conversion to another technique due to the patient's preference. The postoperative course was favorable, just as in the cases of slippage.
There were no unscheduled rehospitalizations in any of our patients, since all associated complications were closely followed in our outpatient clinic. This allowed us to schedule interventions in previously diagnosed patients in the ambulatory setting. The cases that presented port infection were initially treated in the outpatient clinic and then later scheduled for treatment. Only one of the patients with slippage required semi-emergency hospitalization. This patient presented asymmetrical slippage diagnosed in our office that quickly progressed, requiring a faster surgical scheduling. Thus, the hospital and intervention were scheduled in a semi-emergency situation.
The percentage of excess weight loss (EWL) in the 61 patients who were followed for more than 5 years was 54.8%. The remaining patients were followed for between 1 and 5 years. The patients with a follow-up from 3 to 5 years had an EWL of 59.2%, and the patients with a follow-up between 1 and 3 years had an EWL of 61.3%. The patients converted to another technique were excluded from the weighted analysis.
Out of the 61 patients with a follow-up longer than 5 years, 11 (18%) presented an EWL lower than 50. Four of these patients never reached 50, while the rest did during the follow-up but later presented a weight gain that lowered their EWL to below 50.
In our series, we only had 4 super-obese patients with follow-ups that were longer than 5 years, 3 presented an EWL higher than 50, while one patient did not reach this objective.
DiscussionShortly after adjustable gastric banding was approved for use in the treatment of morbid obesity, published reports started to appear that demonstrated positive results. About a decade ago, authors including as Chevalier in France, Ponce in the United States, Super in the United Kingdom, O’Brien and Dixon in Australia, etc., started to publish series with thousands of patients who had undergone the procedure. These solid scientific studies demonstrated not only the effectiveness of the bands but also the low number of complications and, more importantly, the absence of mortality in the majority of the long series.7,14–17
Meanwhile, in Spain we have never been able to reproduce these results, as can be seen from data presented at scientific forums, communications at congresses and national publications. In all these forums, especially at the beginning of the last decade, there were reports of band removal above 50%18 and even reaching 100% in some unpublished series presented at national congresses. There is such a striking difference between national and international results that we sincerely believe that it is time for reflection and self-criticism.
If we contemplate this enormous difference in the results scientifically and rationally, we must consider other series, like those by O’Brien or Dixon in Australia, with their positive published results.11,14–16 It is then difficult to argue that the gastric band procedure is not a good method for treating obesity. Plus, Spanish patients cannot be that different.
Our series, although modest, reproduces the same results that have been published in the international literature using an identical technique to that reported in European articles and a similar follow-up protocol, which is undoubtedly important for reproducing the results.19
Our patients maintained an EWL for more than 5 years of 54%. Although this percentage does not reach the reports made by other authors, it does surpass the established limits for effectiveness with this technique according to the criteria of Fobi and Baltasar.20,21 On the other hand, although the rate of revision surgery needed seems high, it is similar to international series described and should not be interpreted as a failure of the technique.22 This percentage of revision surgery is invariably associated with banding and is something that patients should be informed of before the intervention.
Most publications communicate a need for revision surgery that ranges between 4% and 20%.22–24 Large part of this percentage is attributable to complications related with the access port, all of which are resolved under local anesthesia. Moreover, most complications requiring revision surgery are able to be resolved with surgical solutions that do not involve the removal of the band but instead, in cases of slippage, its readjustment.25 In the majority of series, after the introduction of the pars flaccida technique, band erosions practically disappeared. In our series, there was only 1 erosion out of 132 patients, which also agrees with international publications.26
We can affirm, therefore, that the results published in the literature regarding effectiveness and need for revision surgery are similar if we reproduce the same protocols for surgical technique and follow-up. In our series, mortality was also identical to that published in the literature: 0 mortality.7,11 These data are probably responsible for the exponential increase in the number of gastric band procedures done in obese patients around the world, and fundamentally in the United States.2 The majority of these patients are young people who have a risk factor that most still do not interpret as a disease, and therefore their main concern is safety. In our series, there was no overall mortality, not even when we took into account the patients who had been converted to another technique. As in international series, we are able to affirm that the use of gastric bands in our patients was the safest surgical procedure.25
So, how do we explain the difference in results between international series, other Spanish series and ours?
There is no doubt that all the Spanish authors have reproduced the surgical technique. However, does our health-care model allow us to reproduce the follow-up protocol utilized by the other groups?
Our experience with gastric band surgery patients treated within the public health-care system has taught us that such a protocol is difficult to reproduce. The follow-up of gastric band patients is enormously demanding if we want to achieve positive results. Recent publications have demonstrated that gastric banding works due to the stimulus generated by the passage of food through the band and over the vagal afferent nerve endings.12,13 For this to happen, patient collaboration is essential: the food that passes through the band should be solid enough to compress these receptors and soft enough not to become trapped above the band. Therefore, follow-up is fundamental, and patients need to learn a new way of chewing, swallowing, perceiving sensations and feeding themselves in general. This follow-up entails great effort on the part of both the surgeon and the patient and represents at least half of the gastric band results.19 The private health-care system is able to quickly adapt to these needs but, unfortunately, our public healthcare system is not always able to make such rapid modifications. In this series, the patients we had treated in the public system overloaded our outpatient clinics in order to obtain a positive outcome. If the number of patients had been greater, it would have been impossible to properly follow them all. Nonetheless, the assessment of the differences stated between the two systems is subjective since we observed no differences in our patients.
Our follow-up protocol was similar to other published European reports, and perhaps this explains the similar outcome. Unfortunately, our public healthcare model cannot always provide for such an approach, and this may be the cause of the poor results described in Spain.
Study LimitationsOur study is based on retrospective data obtained from patients who had been treated surgically over the course of a long time period. Even though the follow-up during these 10 years enables us to draw more solid conclusions, the experience in our group has doubtlessly varied along with the number of patients treated. The annual number of gastric band cases was not high, although the surgeons have been the same.
ConclusionsWith the data provided by our series, we cannot continue to argue that gastric band surgery is not a good procedure for the treatment of morbid obesity. Instead, it is an effective procedure and doubtlessly the safest procedure, which is probably why surgeons in the US are using it more and more to treat their patients (0% mortality in our series and 82% of patients with EWL above 50% with follow-ups longer than 5 years). Our future efforts should be focused on reproducing the same follow-up methods within our healthcare system, which would allow us to reach the results published in the international literature.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Lago Oliver J, Vázquez Amigo S, Sánchez García J, Pedraza Toledo G, Mercader Cidoncha E, Sanz Sánchez M, et al. La banda gástrica ajustable como tratamiento de la obesidad mórbida: ¿son reproducibles los resultados mundiales en España? Análisis de 132 pacientes intervenidos en los últimos 10 años. Cir Esp. 2013;91:301–307.