Pulmonary hernias are characterized by a protrusion of the lung through a defect of the chest wall. Herniations of the lung can be either acquired or spontaneous. Predisposing factors have been described, such as obesity, chronic obstructive pulmonary disease (COPD) or the chronic use of corticosteroids. We present the cases of 4 patients with spontaneous lung hernias treated at our hospital in 2015.
The first case is that of a 60-year-old patient who was overweight and had a history of COPD. In February, he reported the appearance of a hematoma on the right thoracic wall, and a CT scan diagnosed a right pulmonary herniation between the 8th and 9th ribs. By thoracotomy, primary closure was performed with non-absorbable sutures. In April, he was diagnosed with pleural effusion compatible with empyema due to S. aureus. A chest drain was inserted, and the treatment was complemented with the intrapleural instillation of urokinase for 4 days, leading to resolution of the condition. After outpatient follow-up, the patient was discharged in May 2015 after showing no signs of relapse.
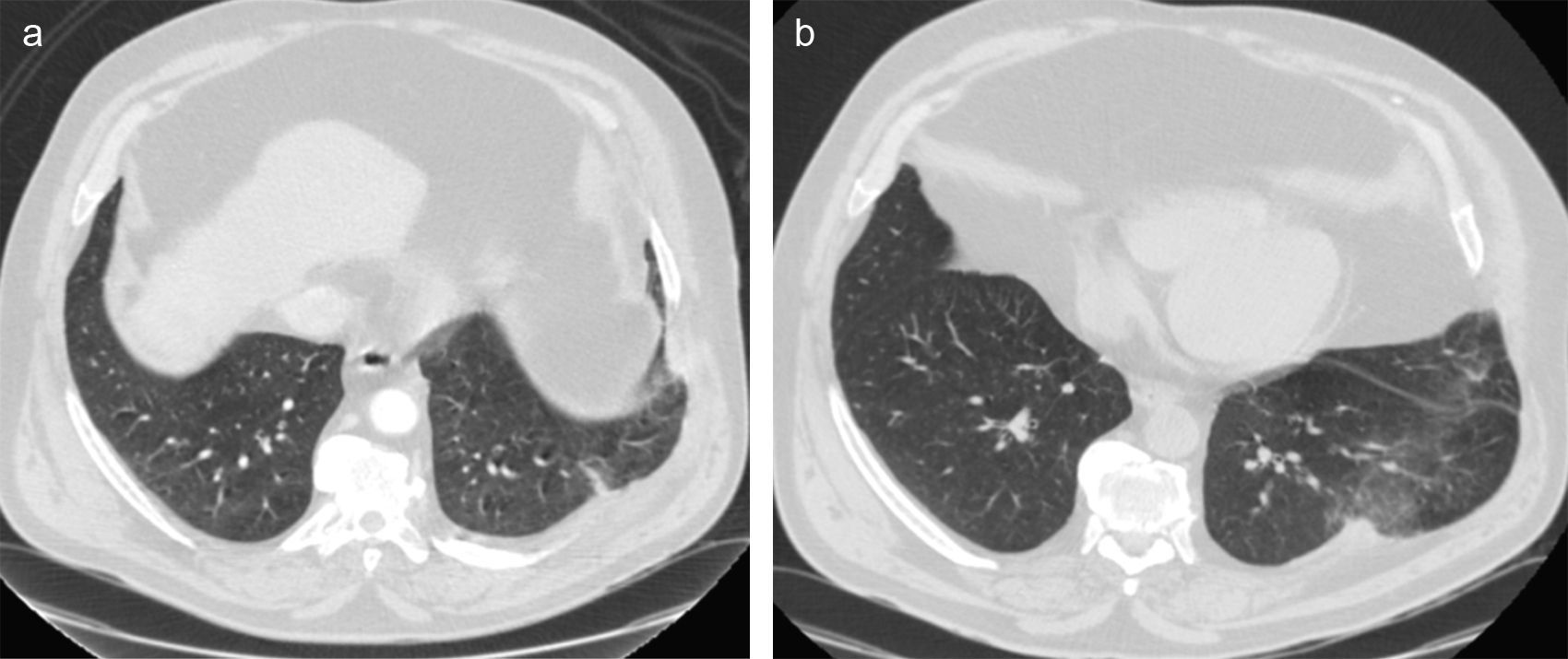
The second case is a 56-year-old patient with a history of COPD and grade III obesity who consulted in February for left chest pain accompanied by chest wall hematoma. CT scan revealed a left pulmonary hernia between the 9th and 10th ribs (Fig. 1a). Primary closure with non-absorbable sutures was performed by means of thoracotomy. In May, the patient again consulted for left rib pain; CT scan demonstrated an image compatible with left pulmonary herniation between the 8th and 9th ribs (Fig. 1b). The defect was closed with placement of polytetrafluoroethylene mesh. In February 2016, the patient presented with a respiratory infection and recurrence of the pulmonary hernia between the 8th and 9th ribs. The patient was treated conservatively with the use of a rib binder and referred to the endocrinology department for a weight loss regimen. The patient's progress is being followed in the outpatient clinic.
The third case is a 68-year-old overweight patient, who consulted in February for intense rib pain accompanied by the appearance of a hematoma. Thoracic CT scan detected a hematoma that was actively bleeding from the left 9th to 10th ribs, which ceased spontaneously. After 10 days, an induration was observed in the area of the hematoma, and the presence of a pulmonary herniation was confirmed. In the month of March, primary closure of the defect was performed with non-absorbable sutures by means of thoracotomy. The last follow-up visit was in the month of April 2016, at which time no signs of relapse had been observed.
The fourth case is that of a 60-year-old patient who was overweight and had a history of asthma. He presented with right chest pain in the month of August, and CT scan revealed a lung hernia between the 8th and 9th ribs. Scheduled surgery was performed in the month of November using thoracotomy with primary closure of the defect with non-absorbable sutures. The last follow-up visit was in the month of March 2016, at which time no signs of recurrence were observed.
Pulmonary herniations are a rare entity and were described for the first time in 1499 by Roland. In 1845, Morel-Lavallée provided a detailed description of lung hernias, classifying them according to their etiology and anatomical location.1,2
Lung herniations are defined as protrusions of the lung parenchyma through the chest wall. They can be classified as spontaneous, traumatic and postoperative. Spontaneous lung hernias account for 30% of cases, and most do not present complications.1,3
Lung hernias are usually asymptomatic and present as an inconsistent mass that protrudes through the intercostal spaces with the elevated pressure maneuvers of the thoracic cavity.1,2 Thoracic CT is a very sensitive test for the diagnosis of lung hernias and is able to assess the hernial orifice and sac as well as the relationship with the pectoral and intercostal muscles.2
The purpose of surgical treatment is to close the defect of the intercostal muscles by means of primary closure with intercostal sutures or with the placement of synthetic mesh material.2 Currently, there are no studies indicating which type of surgical repair is the best for the treatment of lung hernias.3
In summary, we have presented 4 cases of spontaneous pulmonary hernias from the year 2015. In all patients, primary closure of the defect was conducted with non-absorbable sutures, taking into account the size of the defect of the intercostal space and the possibility for rib approximation with sutures. The only case of hernia recurrence was observed in the patient with type III obesity, and it occurred despite the placement of a synthetic mesh. In our experience, obesity is a factor that negatively influences patient progress after the surgical repair of a pulmonary hernia. Primary closure with non-absorbable stitches, without mesh placement, may be adequate surgical treatment for simple spontaneous lung herniations.
AuthorshipsStephany Laguna Sanjuanelo: main writer of the case review and manuscript structure.
Iker López Sanz: main reviewer of the manuscript.
Jon Zabaleta Jiménez and Borja Aguinagalde Valiente: surgeons of the operations conducted, participants in the review of the manuscript.
José Miguel Izquierdo Elena: critical review and approval of the final version.
Please cite this article as: Laguna Sanjuanelo S, López Sanz I, Zabaleta Jimenez J, Aguinagalde Valiente B, Izquierdo Elena JM. Hernia pulmonar espontánea: presentación de 4 casos y revisión de la literatura. Cir Esp. 2017;95:237–239.
The data published in this article have been previously presented as an oral communication at the Spanish National Thoracic Surgery Conference, (SECT), May 5, 2016.