Registries are powerful tools for identifying factors predicting bad results. Our objective was to analyze data from the Spanish Registry of Incisional Hernia (EVEREG) to detect risk situations for the development of complications and recurrences.
MethodsWe have analyzed data of the cohort of hernias registered during the period from July 2012 to June 2014. We have compared the data between complicated and non-complicated patients in the short and long term follow-up. Data compared were: patient demographics, comorbid condition, hernia defect characteristics and surgical technique to determine which of them may be predictors of poor outcomes.
ResultsDuring the period of study, we collected data from 1336 hernias (43.7% males; 56.3% females) with a mean age of 63.6 years (SD 12.4) and BMI of 30.4 (SD 5.4). In the multivariate analysis, factors associated with complications were: age >70 years, previous neoplasm, diameter greater than 10cm, previous repair and bowel resection. Factors related with recurrences were: parastomal hernia, previous repair, emergency repair, postoperative complications and reoperation. A separation of components was the only protective factor for this type of analysis (OR 0.438; CI 0.27–0.71; P=.0001).
ConclusionsRisk factors for the development of complications and recurrences must be considered for promoting preoperative patient prehabilitation, planning the surgical technique and referring patients to specialized abdominal wall units.
Los registros son herramientas potentes para identificar situaciones de riesgo de mala evolución. Nuestro objetivo ha sido analizar los datos del Registro Nacional de Hernia Incisional (EVEREG) para detectar situaciones de riesgo para el desarrollo de complicaciones y recidivas.
MétodosSe analizan los datos de la cohorte de hernias registradas en el período desde julio de 2012 hasta junio de 2014. Se realiza una comparación estadística entre las hernias que presentaron complicaciones y recidivas, y su relación con los pacientes, las características de las hernias y la técnica quirúrgica, para determinar cuáles de ellos pueden predecir malos resultados.
ResultadosEn el período de estudio disponemos de datos de 1.336 hernias (43,7% varones; 56,3% mujeres), con una edad media de 63,6 años (DE: 12,4) e IMC de 30,4 (DE: 5,4). En el estudio multivariante las variables asociadas a la presencia de complicaciones fueron: edad superior a 70 años, neoplasia, longitud del defecto mayor de 10cm, reparación previa y resección intestinal. Las variables asociadas a recidiva fueron: las hernias paraestomales, la reparación previa, la cirugía urgente, la aparición de complicaciones postoperatorias y la reintervención quirúrgica. El uso de una separación de componentes fue el único factor protector en este tipo de análisis (OR: 0,438; IC: 0,27–0,71; p=0,001).
ConclusionesLa presencia de factores de riesgo para la aparición de complicaciones y recurrencias debe ser tenida en cuenta con el fin de proyectar la prehabilitación del paciente para la cirugía, planificar la técnica quirúrgica y su derivación a unidades especializadas.
National registries are very powerful tools that provide a large volume of data. Their analysis enables us to reach conclusions in order to: improve treatment, identify in advance which patients are at higher risk of complications, and identify subgroups requiring specific measures to avoid the appearance of postoperative complications.1–3
The use of registries for abdominal wall surgery has extended worldwide in recent years, and there are numerous contributions related to the analysis of the registered data to achieve a better understanding of this highly prevalent pathology and obtain better results in their treatment.4–7
The Spanish National Registry of Incisional Hernias (EVEREG) was initiated in July 2012. By July 2017, it included data from 160 Spanish hospitals and a total of 7505 cases of hernias related to previous laparotomy (no primary ventral hernias were registered). An initial analysis of the first years of data collection has been previously published, which demonstrated the need to introduce improvements in treatment, especially to reduce the number of complications and recurrences.8
The aim of this study is to analyze, in a cohort of registered cases, variables for patient-related data, surgical situation, hernia characteristics and the surgical technique used in order to predict the appearance of postoperative complications and recurrences, and, based on this knowledge, suggest the implementation of preoperative, technical and postoperative measures to improve results
MethodsThe registry is promoted by the Abdominal Wall and Sutures Division of the Spanish Association of Surgeons. Data are stored in an external server, whose global data are only accessible by the surgeons who head this nation-wide initiative.8 The data were collected prospectively from the Spanish National Registry of Incisional Hernias between July 2011 and June 2014. During this period, a total of 2181 hernias had been registered, and 1336 cases (61.25%) were considered valid for the analysis. The causes for exclusion of the remaining registries were: date of intervention prior to the start of the registry (n=108), errors in data collection that impede analysis (n=237) and absence of follow-up data during the first 30 days after surgery (n=530). The data collection process has been described previously.8 In short, it is an online database maintained by surgeons from each hospital that outlines the parameters for patients, hernias, operations, complications, and follow-up after one month, 6 months, one year and 2 years, for each of the incisional hernias treated. Complications were recorded specifically and classified according to the affected organ, situation (intraoperative and postoperative) and the time of onset (early or late).
The hernias were categorized especially for this study in terms of complexity (low, moderate and high) according to the criteria described by Slater et al.,9 which considered patient/hernia characteristics and the circumstances of the surgery.
Statistical AnalysisThe data were exported to the SPSS v.22 statistical analysis software (IBM Inc., Rochester, MN, USA). Quantitative variables were expressed as mean ± standard deviation and qualitative variables as proportions. To analyze the association between qualitative variables, we used the Chi-squared test (χ2), or Fisher's test when necessary, as well as the Student's t test or the Mann–Whitney test for quantitative variables. The normality of the distribution of the quantitative variables was verified using the Kolmogorov–Smirnov test. Statistical significance was established with a P<.05. In the multivariate analysis, the predictive capacity of each variable and its independence from the other predictor variables were analyzed using a binomial logistic regression model by sequentially introducing the variables with an input F of 0.5.
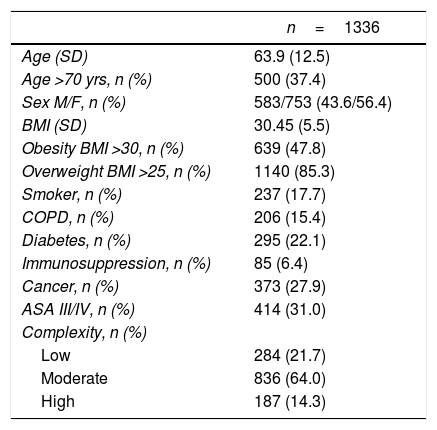
ResultsThe cohort of patients analyzed is shown in Table 1. During the postoperative period, complications occurred in 429 patients (32.1%), 22 of whom (1.7%) died. After a median follow-up of 15.43 months (CI: 12.3–22.5), there were 265 recurrences (20.7%).
Characteristics of the Cohort Patients.
| n=1336 | |
|---|---|
| Age (SD) | 63.9 (12.5) |
| Age >70 yrs, n (%) | 500 (37.4) |
| Sex M/F, n (%) | 583/753 (43.6/56.4) |
| BMI (SD) | 30.45 (5.5) |
| Obesity BMI >30, n (%) | 639 (47.8) |
| Overweight BMI >25, n (%) | 1140 (85.3) |
| Smoker, n (%) | 237 (17.7) |
| COPD, n (%) | 206 (15.4) |
| Diabetes, n (%) | 295 (22.1) |
| Immunosuppression, n (%) | 85 (6.4) |
| Cancer, n (%) | 373 (27.9) |
| ASA III/IV, n (%) | 414 (31.0) |
| Complexity, n (%) | |
| Low | 284 (21.7) |
| Moderate | 836 (64.0) |
| High | 187 (14.3) |
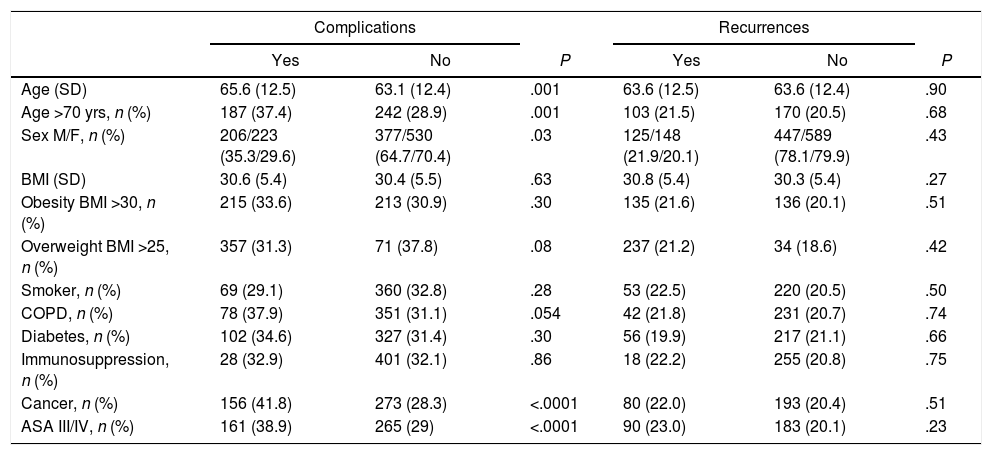
In the analysis of the patient-related factors, age over 70, male gender, history of neoplasm and anesthetic risk correlated with a statistically significant occurrence of postoperative complications (Table 2).
Comparison of Patient-Related Parameters and the Appearance of Postoperative Complications and Recurrences.
| Complications | Recurrences | |||||
|---|---|---|---|---|---|---|
| Yes | No | P | Yes | No | P | |
| Age (SD) | 65.6 (12.5) | 63.1 (12.4) | .001 | 63.6 (12.5) | 63.6 (12.4) | .90 |
| Age >70 yrs, n (%) | 187 (37.4) | 242 (28.9) | .001 | 103 (21.5) | 170 (20.5) | .68 |
| Sex M/F, n (%) | 206/223 (35.3/29.6) | 377/530 (64.7/70.4) | .03 | 125/148 (21.9/20.1) | 447/589 (78.1/79.9) | .43 |
| BMI (SD) | 30.6 (5.4) | 30.4 (5.5) | .63 | 30.8 (5.4) | 30.3 (5.4) | .27 |
| Obesity BMI >30, n (%) | 215 (33.6) | 213 (30.9) | .30 | 135 (21.6) | 136 (20.1) | .51 |
| Overweight BMI >25, n (%) | 357 (31.3) | 71 (37.8) | .08 | 237 (21.2) | 34 (18.6) | .42 |
| Smoker, n (%) | 69 (29.1) | 360 (32.8) | .28 | 53 (22.5) | 220 (20.5) | .50 |
| COPD, n (%) | 78 (37.9) | 351 (31.1) | .054 | 42 (21.8) | 231 (20.7) | .74 |
| Diabetes, n (%) | 102 (34.6) | 327 (31.4) | .30 | 56 (19.9) | 217 (21.1) | .66 |
| Immunosuppression, n (%) | 28 (32.9) | 401 (32.1) | .86 | 18 (22.2) | 255 (20.8) | .75 |
| Cancer, n (%) | 156 (41.8) | 273 (28.3) | <.0001 | 80 (22.0) | 193 (20.4) | .51 |
| ASA III/IV, n (%) | 161 (38.9) | 265 (29) | <.0001 | 90 (23.0) | 183 (20.1) | .23 |
The situation in which the surgery was performed (elective vs urgent) correlated with the appearance of complications (elective 30.5% vs urgent 52%, P<.0001), mortality (elective 1.4% vs urgent 10%, P<.0001) and recurrences (elective 20% vs urgent 32%; P=.006).
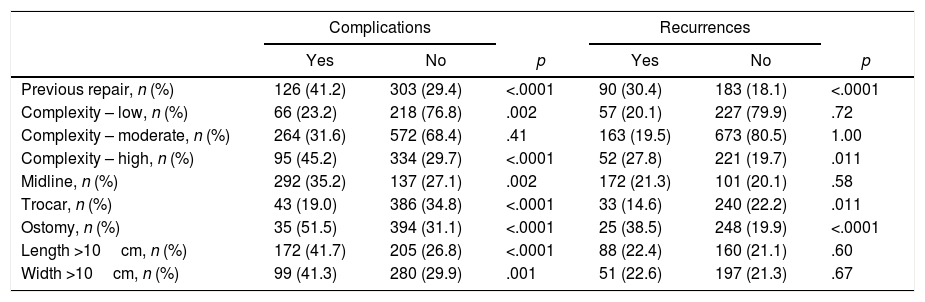
The characteristics of the hernias that were associated with a greater number of complications were (Table 3): previous incisional hernia repair, location in the midline, hernias associated with an ostomy, and the diameter of the defect (transverse and longitudinal diameters greater than 10cm were both significant). In general, more complex hernias were associated with a greater number of complications (45.2% vs 29.7%; P<.0001), mortality (11% vs 0.4%; P<.0001) and recurrences (27.8% vs 19.7%; P=.011). In contrast, trocar hernias presented a lower frequency of complications (P<.0001) and recurrences (P=.011).
Comparison of Hernia Characteristics With the Appearance of Postoperative Complications and Recurrences.
| Complications | Recurrences | |||||
|---|---|---|---|---|---|---|
| Yes | No | p | Yes | No | p | |
| Previous repair, n (%) | 126 (41.2) | 303 (29.4) | <.0001 | 90 (30.4) | 183 (18.1) | <.0001 |
| Complexity – low, n (%) | 66 (23.2) | 218 (76.8) | .002 | 57 (20.1) | 227 (79.9) | .72 |
| Complexity – moderate, n (%) | 264 (31.6) | 572 (68.4) | .41 | 163 (19.5) | 673 (80.5) | 1.00 |
| Complexity – high, n (%) | 95 (45.2) | 334 (29.7) | <.0001 | 52 (27.8) | 221 (19.7) | .011 |
| Midline, n (%) | 292 (35.2) | 137 (27.1) | .002 | 172 (21.3) | 101 (20.1) | .58 |
| Trocar, n (%) | 43 (19.0) | 386 (34.8) | <.0001 | 33 (14.6) | 240 (22.2) | .011 |
| Ostomy, n (%) | 35 (51.5) | 394 (31.1) | <.0001 | 25 (38.5) | 248 (19.9) | <.0001 |
| Length >10cm, n (%) | 172 (41.7) | 205 (26.8) | <.0001 | 88 (22.4) | 160 (21.1) | .60 |
| Width >10cm, n (%) | 99 (41.3) | 280 (29.9) | .001 | 51 (22.6) | 197 (21.3) | .67 |
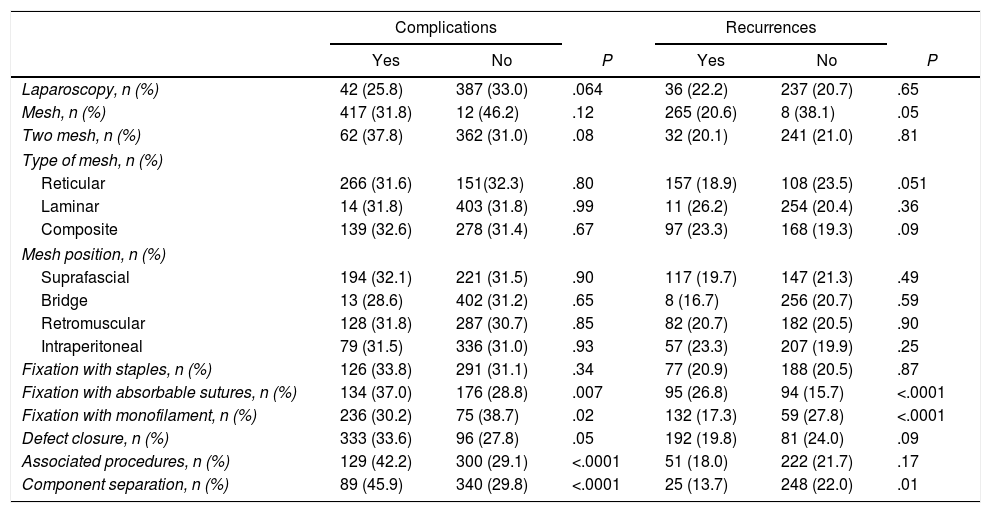
Regarding the surgical technique (Table 4), the approach (open or laparoscopic) showed no significant differences. The use of mesh correlated with a lower number of recurrences (20.6% vs 38.1%; P=.05). The position of the mesh showed no influence on the development of complications or recurrence. On the other hand, significant differences were detected when the mesh fixation systems were compared (Table 4). In order to better examine these technical data, we considered the approach separately. In open surgery, the use of mesh was associated with fewer recurrences (20.3% vs 38.1%; P=.05). Upon comparing the prostheses according to their configuration (reticular, laminar and composite), no differences were found. The use of staples as a fixation system in open surgery presented a greater number of complications (39.5% vs 31.1%; P=.02), but with no influence on mortality and recurrences. The monofilament material produced the fewest complications (30.3% vs 38.3%; P=.03) and recurrences (17.3% vs 30.0%; P<.0001). The use of absorbable suture for mesh fixation was associated with more complications (36.9% vs 28.8%; P=.008) and recurrences (26.9% vs 15.7%; P<.0001). There were no differences between the use of continuous or simple sutures.
Comparison of the Technical Circumstances and the Appearance of Postoperative Complications and Recurrences.
| Complications | Recurrences | |||||
|---|---|---|---|---|---|---|
| Yes | No | P | Yes | No | P | |
| Laparoscopy, n (%) | 42 (25.8) | 387 (33.0) | .064 | 36 (22.2) | 237 (20.7) | .65 |
| Mesh, n (%) | 417 (31.8) | 12 (46.2) | .12 | 265 (20.6) | 8 (38.1) | .05 |
| Two mesh, n (%) | 62 (37.8) | 362 (31.0) | .08 | 32 (20.1) | 241 (21.0) | .81 |
| Type of mesh, n (%) | ||||||
| Reticular | 266 (31.6) | 151(32.3) | .80 | 157 (18.9) | 108 (23.5) | .051 |
| Laminar | 14 (31.8) | 403 (31.8) | .99 | 11 (26.2) | 254 (20.4) | .36 |
| Composite | 139 (32.6) | 278 (31.4) | .67 | 97 (23.3) | 168 (19.3) | .09 |
| Mesh position, n (%) | ||||||
| Suprafascial | 194 (32.1) | 221 (31.5) | .90 | 117 (19.7) | 147 (21.3) | .49 |
| Bridge | 13 (28.6) | 402 (31.2) | .65 | 8 (16.7) | 256 (20.7) | .59 |
| Retromuscular | 128 (31.8) | 287 (30.7) | .85 | 82 (20.7) | 182 (20.5) | .90 |
| Intraperitoneal | 79 (31.5) | 336 (31.0) | .93 | 57 (23.3) | 207 (19.9) | .25 |
| Fixation with staples, n (%) | 126 (33.8) | 291 (31.1) | .34 | 77 (20.9) | 188 (20.5) | .87 |
| Fixation with absorbable sutures, n (%) | 134 (37.0) | 176 (28.8) | .007 | 95 (26.8) | 94 (15.7) | <.0001 |
| Fixation with monofilament, n (%) | 236 (30.2) | 75 (38.7) | .02 | 132 (17.3) | 59 (27.8) | <.0001 |
| Defect closure, n (%) | 333 (33.6) | 96 (27.8) | .05 | 192 (19.8) | 81 (24.0) | .09 |
| Associated procedures, n (%) | 129 (42.2) | 300 (29.1) | <.0001 | 51 (18.0) | 222 (21.7) | .17 |
| Component separation, n (%) | 89 (45.9) | 340 (29.8) | <.0001 | 25 (13.7) | 248 (22.0) | .01 |
In open surgery, component separation presented complications more frequently (45.8% vs 30.5%; P<.0001) as well as mortality (6.3% vs 1.4%; P<.0001), but a lower incidence of recurrences (13.9% vs 21.9%; P=.015). The association of another surgical procedure had a negative influence on complications (44.5% vs 29.5%; P<.0001) and mortality (7.7% vs 0.6%; P<.0001), but not in recurrences (18.7% vs 21.2%; P=.40).
In the laparoscopic repair group, composite mesh was associated with a greater number of recurrences, although without reaching statistical significance (25.6% vs 10.8%; P=.06). Physiomesh (Ethicon, NJ, USA) was not associated with a greater number of complications, but instead with a significantly higher frequency of recurrences (29.1% vs 14.5%; P=.03). No other parameter was associated with a higher frequency of complications and recurrences.
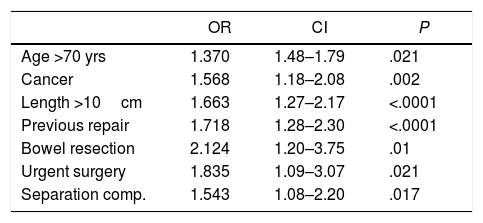
In the multivariate logistic regression analysis (Table 5), a significant relationship was demonstrated between the appearance of complications and age over 70 years, history of neoplasm, longitudinal diameter >10cm, previous repair, urgent surgery, bowel resection and component separation. The combination of these factors was able to predict 70.4% of complications.
Multivariate Analysis of Variables Associated With Postoperative Complications.
| OR | CI | P | |
|---|---|---|---|
| Age >70 yrs | 1.370 | 1.48–1.79 | .021 |
| Cancer | 1.568 | 1.18–2.08 | .002 |
| Length >10cm | 1.663 | 1.27–2.17 | <.0001 |
| Previous repair | 1.718 | 1.28–2.30 | <.0001 |
| Bowel resection | 2.124 | 1.20–3.75 | .01 |
| Urgent surgery | 1.835 | 1.09–3.07 | .021 |
| Separation comp. | 1.543 | 1.08–2.20 | .017 |
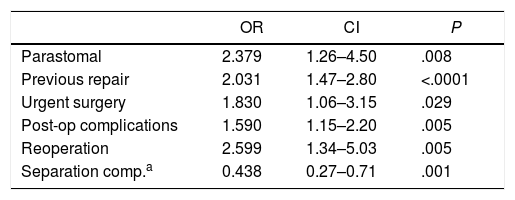
In the multivariate study, factors associated with a higher frequency of recurrences included: parastomal hernias, previous repair, urgent surgery, appearance of postoperative complications and reoperation (Table 6). The use of a separation of components was the only protective factor in this analysis (OR: 0.438; CI: 0.27–0.71; P=.001). In view of the fact that urgent surgery was one of the main factors both for complications and recurrences, we performed an analysis only of patients undergoing elective surgery. After logistic regression, the parameters that maintained a significant relationship with complications were: age over 70 years (OR: 1.329; CI: 1.00–1.75; P=.04), history of neoplasia (OR: 1.572; CI: 1.17–2.11; P=.003), longitudinal diameter >10cm (OR: 1.364; CI: 1.20–1.54; P<.0001), previous repair (OR: 1.720; CI: 1.27–2.33; P<.0001) and associated dermolipectomy (OR: 2.220; CI: 1.04–4.75; P<.04). For recurrences in elective surgery, the model yielded: parastomal hernias (OR: 2.538; CI: 1.31–4.91; P=.006), transverse diameter >10cm (OR: 1.316; CI: 1.09–1.58; P=.003) and previous repair (OR: 2.062; CI: 1.47–2.89; P<.0001); meanwhile, component separation was a protective factor (OR: 0.397; CI: 0.23–0.67; P=.001). Both models were able to predict 85% of complications and recurrences in elective surgery.
Multivariate Analysis of Variables Associated With Recurrences.
| OR | CI | P | |
|---|---|---|---|
| Parastomal | 2.379 | 1.26–4.50 | .008 |
| Previous repair | 2.031 | 1.47–2.80 | <.0001 |
| Urgent surgery | 1.830 | 1.06–3.15 | .029 |
| Post-op complications | 1.590 | 1.15–2.20 | .005 |
| Reoperation | 2.599 | 1.34–5.03 | .005 |
| Separation comp.a | 0.438 | 0.27–0.71 | .001 |
The analysis of our study revealed very interesting data that can be applied to the treatment of incisional hernias. First of all, the registry itself, as previously shown by registries from other countries,4–7 confirms its usefulness for the collection and analysis of data. The main limitations of our study are the inability to study all the patient data recorded in the registry, as many cases from the database were not useful due to the lack of basic elements for analysis or errors in their compilation. Another limitation is that they are just a sample of reality, because Spain does not have a universal registry like other national registries,5 which may lead to biases related to the type of patients and the hospitals that treat them. In our study, the high frequency of complications, affecting 32.1% of surgeries, is striking. This demonstrates that we are facing a pathology with a considerable surgical risk. Likewise, the number of recurrences (20.7%) is high, demonstrating that improvements are necessary for treatment.
Patient-related risk factors affect the appearance of postoperative complications and not recurrence. Age over 70 years, male sex, history of cancer and anesthetic risk were significantly associated with complications, while other factors such as COPD, DM and immunosuppression did not reach significant differences. These factors must be taken into account in order to prioritize the programming of elective repair, as has been suggested by other authors.10,11
The lack of correlation between the BMI and complications/recurrences is noteworthy, since other authors9,12–14 have found an association of this parameter with both. This is probably due to the characteristics of our population, in which a considerable number of patients were obese with a high average BMI (30.45kg/m2).
We fund this specific datum very interesting as, like other authors,12 we believe that reducing the BMI of patients should be a priority objective to reduce postoperative complications and recurrences. This is also one of the few patient-related factors that can be modified before surgery.
The circumstances of the repair correlated with a greater number of complications and recurrences. Therefore, any repair in an emergency context could have better results if treated by an expert team. Other studies on urgent incisional hernia surgery10 have shown a low frequency of intestinal resections due to strangulation and even lower mortality than other types of hernias, so that initially considering a conservative approach can be safe in well-selected cases.
Hernia characteristics are crucial to be able to predict the appearance of both postoperative complications and recurrences. As a protective variable, our data show that trocar herniation had the lowest recurrence rate, although this was not confirmed in the multivariate analysis. In this case, it is likely that these data are related to the size of the defect.
In studying complexity,9 we have found that this classification system is useful for predicting complications and recurrences. In fact, all the statistically significant factors in our study are taken into account in this classification system. So, in our opinion, our study validates this method as useful for the decision-making process of incisional hernia repair, and even encourages us to again recommend that moderately to highly complex hernias be treated by expert surgeons whenever possible.
As for the technical aspects, the approach, the type of mesh used and its position do not stand out as factors related with prognosis. Other details, however, are relevant. Mainly, the association of component separation correlated with a greater number of complications, probably because it was used in more complex hernias. However, patients treated with this technical resource presented fewer recurrences. These same data were maintained among the factors revealed in the multivariate study, both in the group of patients as a whole and in only those undergoing elective surgery. Again, we found another detail that seems to indicate that treatment conducted by specialized teams could be associated with better prognosis, this time in the case of recurrences.
When the repair was associated with other procedures, there was a higher frequency of complications in the univariate analysis. Specifically, bowel resection was the only significant procedure in the multivariate analysis of all the patients. Surely this factor is unmodifiable and related to urgent surgery, therefore entailing a poorer prognosis.
Another datum of the technique that has not been highlighted by the literature on this subject is that the use of absorbable sutures for mesh fixation is related to a greater frequency of complications, and especially of recurrences. In contrast, monofilament sutures are associated with fewer complications and recurrences. Therefore, based on our data, we recommend using non-absorbable monofilament sutures for mesh fixation in these patients.
Finally, regarding the separate analysis of the different types of prosthetic mesh, our study confirms what has been demonstrated by other research15 in reference to an increased frequency of recurrences with Physiomesh (Ethicon, NJ, USA).
In summary, several measures for improvement should be implemented in the treatment of patients with incisional hernia. Surgeons should insist on reducing patient BMI, referring patients to or creating specialized weight loss units for the global treatment of obesity. Patients should be very carefully evaluated in the emergency room to improve their status and ensure that they are referred to specialized units, if required. In view of the results, the creation of specific abdominal wall surgery units seems recommendable; in this manner, the negative effects of complex hernias can be attenuated and the use of technical resources for their treatment can be streamlined. This suggestion has also been included in other studies about abdominal wall surgery16 and intestinal anastomoses.17 In order to provide data on surgeons, it seems clear that we should incorporate parameters related to surgical training in the registry.
FundingB. Braun.
Conflict of InterestsThe authors have no conflict of interests to declare.
Silvia Martínez and Xavier Masramón; SAIL (Servicio de Asesoría a la Investigación y Logística)
Antonio Utrera González, Hospital Juan Ramón Jiménez, Huelva
José M. Capitán Vallvey, Complejo Hospitalario de Jaén, Jaén
Matías Pradas, Hospital Comarcal de Ronda, Ronda, Málaga
Daniel Pérez Gomar, Hospital Universitario Puerta del Mar, Cádiz
Manuel Bustos, Hospital Virgen del Rocío, Sevilla
Francisco Antonio Herrera Fernández, Hospital Comarcal Santa Ana, Motril
Juan A. Blanco, Hospital Civil de Málaga
Joaquim Robres Puig, Consorci Sanitari Integral de l’Hospitalet, Barcelona
Rafael Villalobos, Hospital Arnau de Vilanova, Lleida
Dolors Güell Puigcercos, Hospital de Terrassa, Terrassa
José María Puigcercós Fusté, Hospital Dos de Maig, Barcelona
Vicente Ayuso Osuna, Hospital Espíritu Santo, Santa Coloma Gramanet
Marta Piñol, Hospital Espíritu Santo, Santa Coloma Gramanet
Carles Olona Casas, Hospital Joan XXIII, Tarragona
Francisco Martínez Ródenas, Hospital Municipal de Badalona, Badalona
Jordi Comajuncosas, Hospital Parc Sanitari Sant Joan de Déu, Sant Boi
Enric Sebastián Valverde, Hospital Parc Sanitari Sant Joan de Déu, Sant Boi
Sara Amador, Hospital de Granollers
Jaume Gelonch, Hospital de Palamós
Helena Vallverdú, Hospital de Vic
Magda Abelló Sala, Hospital Pius, Valls
Antonio Veres Gómez, Hospital de la Cerdaña
Rosa Gamón, Hospital General de Castellón
Pedro García Peche, Hospital General Universitario Reina Sofía, Elche
Miguel González Valverde, Hospital General Universitario Reina Sofía, Elche
Miguel Ángel Martín Blanco, Hospital de Vinaroz
Ramón J Ferri, Hospital Lluís Alcanyís, Valencia
Elena Martí Ciñat, Hospital Malvarrosa, Valencia
Providencia García Pastor, Hospital Universitario La Fe, Valencia
Carlos Montero, Hospital Virgen de los Lirios, Alcoy
Miguel Ángel Lorenzo Liñán, Hospital General de Onteniente
Vicente Barbero, Complejo Hospitalario Virgen de la Salud, Toledo
Miguel Ángel Morlan, Complejo Hospitalario Virgen de la Salud, Toledo
José María Jover, Hospital de Getafe
Isabel Delgado Lillo, Hospital Clínico San Carlos, Madrid
Maria Mercedes Sanz Sánchez, Hospital General Universitario Gregorio Marañón, Madrid
Leire Zarain Obrador, Hospital General Universitario Gregorio Marañón, Madrid
Alejandro Lusilla, Hospital General Universitario Gregorio Marañón, Madrid
Juan Jesús Cabeza Gómez, Hospital Clínico San Carlos, Madrid
Antonio López, Hospital Nuestra Señora del Prado, Talavera de la Reina
Teresa Butrón, Hospital Universitario 12 de Octubre, Madrid
Guillermo Supelano Eslait, Hospital Universitario 12 de Octubre, Madrid
José Luis Álvarez Conde, Complejo Hospitalario de Palencia
Baltasar Pérez Saborido, Hospital Río Ortega, Valladolid
Mario Rodríguez López, Hospital Río Ortega, Valladolid
Santiago Revuelta Álvarez, Hospital Universitario Marqués de Valdecilla, Santander
Pedro Trillo Parejo, Complexo Hospitalario Universitario, Orense
José Luis Rodicio, Hospital Universitario Central de Asturias, Oviedo
Antonio Blanco, Hospital Universitario Central de Asturias, Oviedo
Members of the EVEREG registry are listed in Appendix A.
Please cite this article as: Pereira JA, Montcusí B, López-Cano M, Hernández-Granados P, Fresno de Prado L, Miembros del registro EVEREG. Factores de riesgo de mala evolución en la reparación de hernias incisionales: Lecciones aprendidas del Registro Nacional de Hernia Incisional (EVEREG). Cir Esp. 2018;96:436–442.
This work was presented at the Congress of the European Hernia Society (May 2017, Vienna) with the title: “Registries as tool to identify risk factors for bad outcomes”.