The treatment of chronic anal fissure (FAC) differs depending on the professional. To come to a consensus, the current situation in Spain should be studied.
The aim of this study is to evaluate the current situation of the management of FAC in Spanish hospitals.
MethodsDescriptive study, with data from a survey of surgeons of the Spanish Association of Coloproctology. Data was collected according to the doctor's autonomous community, type of hospital and professional category; FAC management data and 3 clinical cases.
ResultsResponse was obtained from 152 surgeons. Pharmacological measures stand out as the first therapeutic step (93.38%). In patients with hypertonia and with no risk factors for fecal incontinence (FI), 55.9% use hygienic-dietary measures associated with nitroglycerin ointment (MHG+NTG). The second step is internal lateral sphincterotomy (ELI) (43.4%). MHG+NTG (75.7%) is used in patients with FI risk factors and in case of failure, ELI is used with a prior ultrasound and/or manometry. In young patients with unexplained hypertonia and incapacitating proctalgia with no risk factors for FI, MHG+NTG (55.9%) is used and, if it is not successful, they are treated with ELI (46.1%).
ConclusionsThe management of FAC in Spain shows similarities with the international guideline suggestions. Nevertheless, some differences can be seen from the first stages of treatment.
El tratamiento de la fisura anal crónica (FAC) difiere en función del profesional. Para plantear un consenso, sería conveniente conocer el estado actual a nivel nacional. El objetivo del presente estudio es conocer la situación actual del manejo de la FAC en los hospitales españoles.
MétodosEstudio descriptivo, con datos de encuestas a cirujanos de la Asociación Española de Coloproctología en las que se han recogido datos de la comunidad autónoma, tipo de hospital y categoría profesional, opinión sobre el manejo de la FAC en general y relativa a 3 casos clínicos específicos.
ResultadosSe ha recibido respuesta de 152 cirujanos. Las medidas farmacológicas constituyen el primer escalón terapéutico (93,38%). En paciente con hipertonía y sin factores de riesgo de incontinencia fecal (IF), el 55,9% emplea medidas higiénico-dietéticas asociadas a pomada de nitroglicerina (MHG+NTG). El segundo escalón lo constituiría la esfinterotomía lateral interna (ELI) (43,4%). En paciente con factores de riesgo de IF, se utiliza MHG+NTG (75,7%) y en caso de fracaso, ELI previa ecografía y/o manometría. En paciente joven con hipertonía inexplorable y proctalgia incapacitante sin factores de riesgo de IF, se trataría con MHG+NTG (55,9%) y si fracasa, ELI (46,1%).
ConclusionesEl manejo de la FAC en España presenta similitudes con las recomendaciones que realizan las guías internacionales. Sin embargo, se observan algunas diferencias incluso desde las primeras opciones de tratamiento.
Chronic anal fissures (CAF) are painful lesions of the anal region and one of the most frequent reasons for consultation with a surgeon. They consist of a linear ulcer that can extend from the pectineal line to the anal margin, usually located on the posterior midline of the anus. CAF cause symptoms that can significantly affect patient quality of life.
The condition is considered acute when it presents a short evolution and does not require more treatment than hygienic-dietary recommendations (HDR), which usually resolve in 6–8 weeks.1 Once this time has elapsed, the fissure becomes chronic and, in addition to the time progression, the persistence of symptoms and other signs, such as the evidence on examination of a sentinel papilla or even the visualization of fibers of the internal sphincter, help establish the diagnosis.
Current CAF treatments are aimed at treating the cause. According to the most accepted etiopathogenic theories, the most probable causes of CAF are hypertonia of the internal anal sphincter and local mucosal ischemia that occurs as a consequence of sphincter spasm, which contributes to the maintenance of the fissure and prevents its healing. Treatment should be aimed at reducing this elevated resting pressure, for which there are different therapeutic options, including: HDR; topical treatments such as nitroglycerin ointments (NTG) or calcium channel blockers (CCB); surgical measures, such as lateral internal sphincterotomy (LIS); and other techniques, such as intramuscular injection of botulinum toxin (BT).
Until a few years ago, LIS was the most widely used treatment, but the incontinence rate (mainly gases), which in some cases reached 45%,2 have motivated research of the possibility of using chemical sphincterotomy.
Therefore, these treatments are the first steps of most international guidelines. However, today the management of CAF continues to be very surgeon-dependent, and differences are observed in the therapeutic management among medical professionals.
The objective of this study is to determine the current situation of CAF treatment in Spain.
MethodsWe have conducted a descriptive study with data collected from surveys sent in 2015 to all surgeons who were members of the Spanish Association of Coloproctology Foundation (Fundación Asociación Española de Coloproctología), by email.
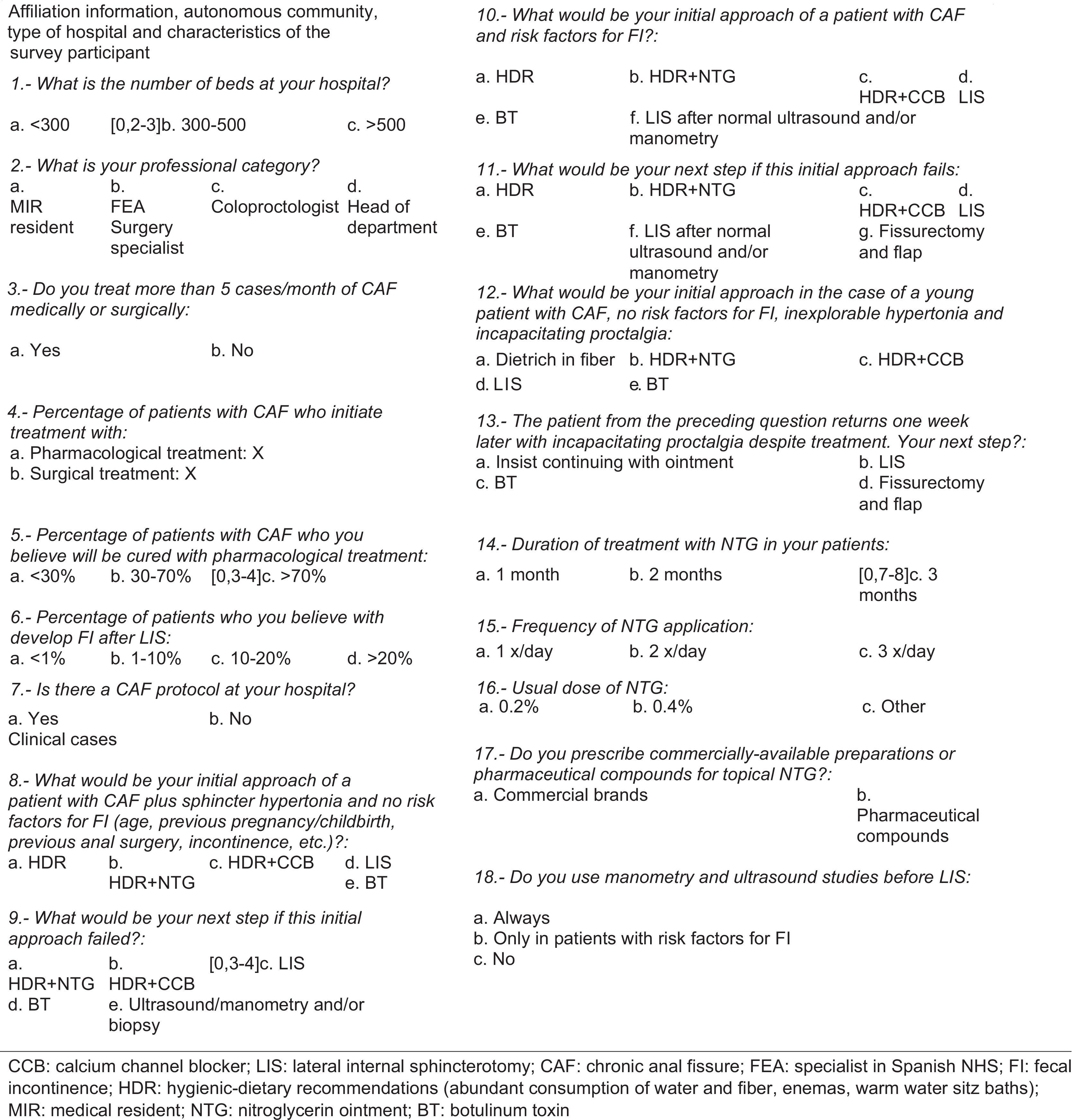
The survey (Fig. 1) consists of 18 questions. The first part includes questions regarding professional information of the surgeons surveyed. The second part presents 3 case reports and poses 6 questions about them. For more information about the overall management of anal fissure, the third case report refers to the treatment of acute anal fissure.
Fecal incontinence (FI) is defined as the uncontrollable and recurrent passage of fecal material for at least one month. Partial FI is defined as the inability to control gases or the appearance of soiling.
The statistical analysis has been done with SPSS version 24 computer software.
The descriptive statistics of the quantitative and qualitative variables have been analyzed. Likewise, a comparative study of the qualitative variables was carried out by applying the Chi-squared test and ANOVA for the analysis of quantitative and qualitative variables of 2 or more groups.
ResultsResponses were received from 152 surgeons throughout Spain. A total of 71 hospitals participated: 36 public, 20 private subsidized and 15 private.
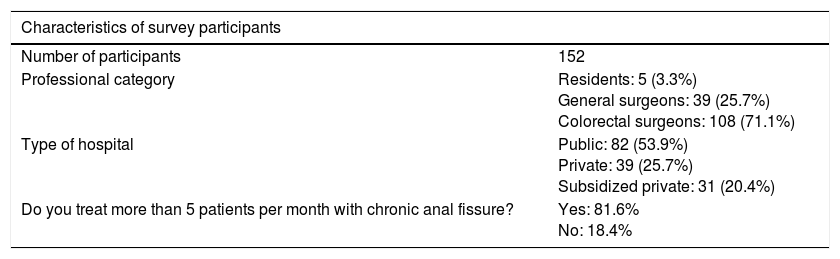
The demographic and professional characteristics are shown in Table 1.
Characteristics of the Surgeons Who Answered the Survey.
| Characteristics of survey participants | |
|---|---|
| Number of participants | 152 |
| Professional category | Residents: 5 (3.3%) General surgeons: 39 (25.7%) Colorectal surgeons: 108 (71.1%) |
| Type of hospital | Public: 82 (53.9%) Private: 39 (25.7%) Subsidized private: 31 (20.4%) |
| Do you treat more than 5 patients per month with chronic anal fissure? | Yes: 81.6% No: 18.4% |
MIR: medical resident.
General surgeon: surgeon treating patients with general surgery processes, with no specialized sub-area.
Colorectal surgeon: surgeon who is mostly involved with the treatment of coloproctology conditions.
CAF management data. When we analyzed the percentage of patients who initiated treatment with pharmacological measures or with surgical measures, there were significant differences depending on the professional category of the surgeon. Coloproctologists most frequently initiated treatment with pharmacological measures (94.2%), closely followed by surgery residents (MIR) (93%), with general surgeons in last place (91%). General surgeons most often indicated surgery as the initial treatment (8.9%), followed by residents (7%), and coloproctologists were the least aggressive in their original treatment (5.6%).
Regarding the existence of a CAF treatment protocol at their hospitals, most surgeons responded affirmatively (62.5%), and differences were observed according to the hospital to which they belonged.
According to the surgeons surveyed, the percentage of patients who began treatment with medical measures was 93.3%, with no statistically significant differences between different autonomous communities. There were, however, significant differences between hospital types. Medical treatment as the initial treatment was more frequently used at public hospitals (94.4%) and private hospitals (93.1%) than at subsidized hospitals (90.9%) (P=.03). A similar situation was observed in terms of surgical treatment and, although it was used less frequently as the first step, the figures were once again more similar between public hospitals (5.4%) and private hospitals (6.8%) than in subsidized private hospitals (9%) (P=.02).
Likewise, statistically significant differences were also observed when comparing the treatment of CAF according to hospital size (defined by number of beds); the surgeons working at larger medical centers were more conservative.
The next question is related to the cure rate of patients with CAF who only received medical treatment. The most frequent response was “30%–70%” (59.9%). As for the percentage of patients who developed FI after LIS, the majority of surgeons (58.6%) indicated that the incidence was “<1%”. When asked about the use of complementary tests, such as ultrasound or anorectal manometry, the majority of respondents (72.4%) used these studies only in situations of patients with FI risk factors.
Clinical cases. In this part of the survey, 3 clinical situations with different therapeutic options are presented.
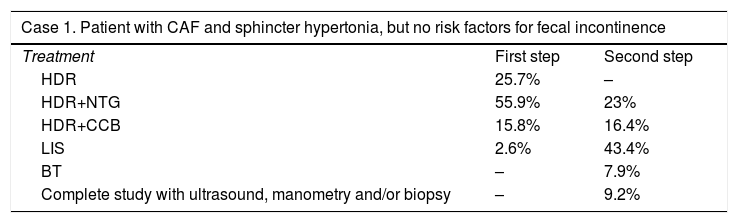
The first reports the case of a patient with CAF and sphincter hypertonia, but with no risk for FI. Among the possible options offered, the majority favored starting treatment with HDR+NTG (55.9%) and, in case of failure, performing LIS (43.4%) (Table 2).
Case 1.
| Case 1. Patient with CAF and sphincter hypertonia, but no risk factors for fecal incontinence | ||
|---|---|---|
| Treatment | First step | Second step |
| HDR | 25.7% | – |
| HDR+NTG | 55.9% | 23% |
| HDR+CCB | 15.8% | 16.4% |
| LIS | 2.6% | 43.4% |
| BT | – | 7.9% |
| Complete study with ultrasound, manometry and/or biopsy | – | 9.2% |
CCB: topical calcium channel blocker; LIS: lateral internal sphincterotomy; CAF: chronic anal fissure; HDR: hygienic-dietary recommendations; NTG: nitroglycerin ointment; BT: botulinum toxin.
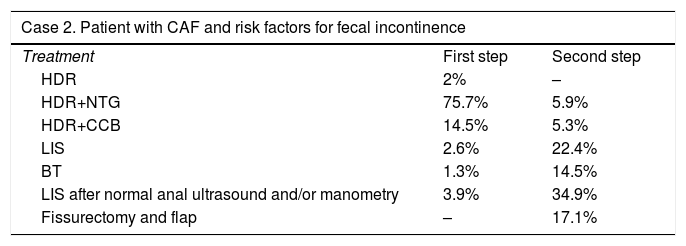
The second case was a patient with CAF and risk factors for FI. In this case, the option most frequently selected as the first step was, once again, HDR+NTG (75.7%), followed by HDR+CCB (14.5%); the third most frequent option was LIS after having performed ultrasound and manometry and having shown no internal sphincter defects or decreased baseline anal pressures (3.9%). The second therapeutic step in this situation was once again LIS after performing anorectal manometry and ultrasound, with no abnormal results in either (34.9%) (Table 3).
Case 2.
| Case 2. Patient with CAF and risk factors for fecal incontinence | ||
|---|---|---|
| Treatment | First step | Second step |
| HDR | 2% | – |
| HDR+NTG | 75.7% | 5.9% |
| HDR+CCB | 14.5% | 5.3% |
| LIS | 2.6% | 22.4% |
| BT | 1.3% | 14.5% |
| LIS after normal anal ultrasound and/or manometry | 3.9% | 34.9% |
| Fissurectomy and flap | – | 17.1% |
CCB: topical calcium channel blockers; LIS: lateral internal sphincterotomy; CAF: chronic anal fissure; HDR: hygienic-dietary recommendations; NTG: nitroglycerin ointment; BT: botulinum toxin.
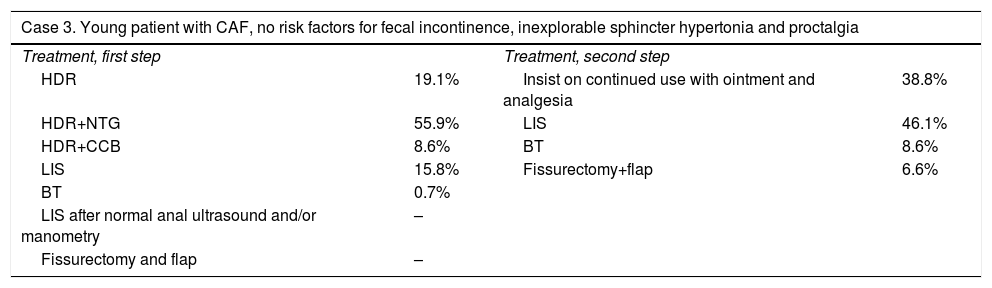
The third clinical case proposed was that of a young patient with CAF, with no FI risk factors, sphincter hypertonia that could not be examined and incapacitating proctalgia. Most surgeons again relied on HDR+NGT (55.9%). The question linked to the previous case reflects how the same patient, who had been treated for one week with HDR+topical treatments (NTG/CCB), reported disabling proctalgia one week later. In this case, LIS was the preferred option (46.1%) (Table 4).
Case 3.
| Case 3. Young patient with CAF, no risk factors for fecal incontinence, inexplorable sphincter hypertonia and proctalgia | |||
|---|---|---|---|
| Treatment, first step | Treatment, second step | ||
| HDR | 19.1% | Insist on continued use with ointment and analgesia | 38.8% |
| HDR+NTG | 55.9% | LIS | 46.1% |
| HDR+CCB | 8.6% | BT | 8.6% |
| LIS | 15.8% | Fissurectomy+flap | 6.6% |
| BT | 0.7% | ||
| LIS after normal anal ultrasound and/or manometry | – | ||
| Fissurectomy and flap | – | ||
CCB: topical calcium channel blockers; LIS: lateral internal sphincterotomy; CAF: chronic anal fissure; HDR: hygienic-dietary recommendations; NTG: nitroglycerin ointment; BT: botulinum toxin.
In the last part of the survey, Spanish surgeons were asked about their experience with NTG ointments. In terms of treatment time, most surgeons prescribed its use for 2 months (59.2%), 21.1% for one month and 17.8% maintained this treatment for 3 months.
The ointment that most surgeons prescribed was 0.4% NTG ointment (59.2%); 36.8% prescribed the 0.2% ointment, 7% preferred 0.3%, and 1.5% prescribed concentrations not included in the survey. The majority (52.6%) of the Spanish surgeons prescribed the pharmaceutical compound for the topical NTG more frequently than commercial preparations (45.4%).
DiscussionAnal fissure is the second most frequent reason for consultation in coloproctology units, surpassed only by hemorrhoid disease.
The therapeutic algorithm is controversial. Several guidelines make recommendations, but their application in daily practice varies greatly, depending on the surgeon, medical center and, of course, the patient.
However, there seems to be consensus that the initial treatment should be conservative, based mainly on HDR and on topical treatments such as NTG or CCB ointments. This can be seen in the guidelines of The Association of Coloproctology of Great Britain and Ireland (ACPGBI),3 The American Society of Colon and Rectal Surgeons,4 Italian Coloproctology Society (SICCR),5 the NICE Guidelines6 and the latest Cochrane review.7
The reflection of the application of these guidelines in Spain can be observed in the results of this survey sent to all the surgeons who are members of the Spanish Association of Coloproctology Foundation.
In this manner, by analyzing the results obtained, we can affirm that the initial treatment step is similar to the guidelines: among the 152 surgeons surveyed, 93.3% use conservative treatment at the beginning, while only 6.5% started treatment with surgical measures. This is the first agreement with the guidelines and with some articles in the literature that discuss adherence of CAF treatment to the ACPGBI guidelines.3
The cure rate percentage of healing that we found in the literature after performing conservative measures varies depending on the drug. Thus, compounds with NTG obtain variable rates, from 48.9%8 to 86%.9 For the case of topical treatments with CCB, this percentage also varies: 65%–94.5%,8 and if we differentiate between diltiazem or nifedipine, the percentages are 75% and 96%, respectively.9 In our survey, without differentiating by type of topical treatment, the majority of surgeons who have answered expect to have cure rates that range between 30% and 70%. Regarding topical treatments with NTG or CCB ointments, our results are in favor of the first, coinciding with the recommendations made in international guidelines. Therefore, it seems that there is an awareness that medical treatment should be the first therapeutic step in CAF.
However, we found studies in the literature in which the cure rate with NTG ointments is still small (40%), with important rates of headache (27.5%) and non-compliance (22.5%). In the case of treatment with CCB, cure rates similar to those obtained with NTG ointments are observed, but it has a lower associated incidence of headaches and, therefore, a lower non-compliance rate.2
When asked about the percentage of incontinence after performing LIS, most participants responded that less than 1% of patients developed this complication. However, in the literature these rates are significantly higher, and some articles report rates of 3%–45%,8,10,11 differentiating between incontinence for gases (20%), soiling (20%) and small stool leaks (3%–10%).12
Questions were also asked about 3 different situations that could occur in clinical practice. In all 3, the choice of conservative treatment at the beginning, leaving surgical treatment for the second step, is the most frequently chosen. It can be said, therefore, that the approach of Spanish surgeons is quite in line with the recommendations of international guidelines, except for one detail: the results show that in Spain there is a tendency to obviate the isolated HDR step and directly initiate CAF treatment with NTG ointment. Very few patients heal after HDR alone, and some studies report that for every 20 patients treated with HDR, only one experiences healing.8 However, others show that with isolated HDR, an 87% cure rate would be reached in the case of acute fissures, and this percentage would decrease up to 50% in the case of CAF.9
Regarding the treatment of CAF with intramuscular injection of BT, there are comparative studies with topical NTG ointments in which BT obtained similar cure rates with no adverse effects, so this technique may be the treatment of choice for many surgeons.13–15
The problem of this treatment is related to its availability and the high recurrence figure observed in other studies. To avoid the latter, a treatment with high doses of BT (100U), and even reinjection of 50U in recurrences, is preferred.15–17
Certain studies have observed that the persistence of pain after the first post-op follow-up visit is a risk factor for the development of recurrence (OR: 3.9, CI: 1.5–9.7; P=.003).18
In addition, there are studies that correlate these recurrences with the chronicity of the lesion (more than 12 months of symptoms) and conclude that, given the high risk of recurrence, surgical sphincterotomy should be the first therapeutic option.15,19
According to the results of this survey, treatment with BT in Spain is reserved for patients in whom medical treatment has failed and, normally, would present a high risk of incontinence if LIS were performed. However, the limited availability of this treatment in Spanish medical centers is one of the possible reasons why it is relegated to a third or fourth step in therapeutic management. It can be concluded that, in this aspect, the therapeutic algorithms of the guidelines are dissimilar from our standard clinical practice, as Spanish surgeons tend to perform more LIS than BT infiltrations.
In conclusion, the management of CAF in Spain presents similarities with the recommendations made by international guidelines, but some differences are observed.
Once the fissure is diagnosed as chronic, the first lines of treatment should be conservative, and patient treatment should begin with HDR. However, in Spain the initial treatment involves these measures together with NTG ointment, and at this point the management differs with the therapeutic algorithms of the international guidelines. In case of failure, the guidelines recommend the association of topical therapies with HDR. In Spain, the treatment indicated in this some phase is surgical.
The next step of the guidelines is occupied by invasive treatments. Among these, BT and LIS stand out. The limited use of BT in Spain is striking, which is normally due to its availability and the recurrence rate that is generally evident the third or fourth month after treatment and in patients who present a long history of CAF. Therefore, in our country, once topical treatments have failed, most cases are treated directly with LIS.
AuthorshipStudy design: M. Mar Aguilar, A. Arroyo, J. Santos, M.A. Gómez.
Data collection: M. Mar Aguilar, A. Arroyo, A. Fernández, M.J. Alcaide, P. Moya, M.A. Gómez.
Analysis and interpretation of the results: M. Mar Aguilar, A. Arroyo, P. Moya, R. Calpena.
Critical review and approval of the final version: A. Arroyo, R. Calpena.
Conflict of InterestThis manuscript presents no conflict of interests.
Please cite this article as: Aguilar MM, Moya P, Alcaide MJ, Fernández A, Gómez MA, Santos J, et al. Resultados de la encuesta nacional sobre el tratamiento de la fisura anal crónica en los hospitales españoles. Cir Esp. 2018;96:18–24.