Bleeding is a common complication of proctitis secondary to radiotherapy of pelvic tumors. Between 5% and 10% may become severe and refractory to topical and endoscopic treatment. Experience with the application of 4% formaldehyde is presented.
Patients and methodsA retrospective and descriptive study was performed on a patient cohort with severe radiation proctitis admitted to the Hospital Universitario Donostia between January 2003 and September 2009. All patients were diagnosed by colonoscopy and admitted due to the severity of their treatment. Both 4% formaldehyde and the gauze technique were used, as well as using enemas, in cases refractory to topical and endoscopic treatment with argon. The technique was performed in theater with regional anesthetic. Clinical and endoscopic follow-up was carried out.
ResultsThe study included 25 men (73.5%) and 9 women (26.5%), with a mean age of 69 years (32–80) who had rectal bleeding due to radiation proctitis and required admission. All treatments failed in 6 (28.5%) patients, and 4% formaldehyde was used, with a complete response to the bleeding in all 6 patients, with 3 cases requiring one session, and the 3 others 2 sessions. The gauze technique was used in 4 patients and another 2 were given a formaldehyde enema due to the presence of stenosis. Pain appeared as the main complication in 2 (33.3%) patients. The median follow-up was 60 months (interquartile range 26–67 months).
ConclusionsThe use of 4% formaldehyde in bleeding due to radiation proctitis is an effective, easy to reproduce technique, with a low morbidity.
La hemorragia es una complicación frecuente de la proctitis secundaria a radioterapia de tumores pélvicos. Entre el 5 y el 10% pueden ocasionar cuadros graves y rebeldes a los tratamientos tópicos y endoscópicos. Se presenta la experiencia con la aplicación de formaldehído al 4%.
Pacientes y métodoEstudio retrospectivo y descriptivo de una cohorte de pacientes con proctitis actínica grave ingresados en el Hospital Universitario Donostia entre enero de 2003 y septiembre de 2009. Todos los pacientes fueron diagnosticados por colonoscopia e ingresados por su severidad para tratamiento. Se empleó formaldehído al 4% tanto con la técnica de la gasa como mediante enemas, en los casos rebeldes al tratamiento tópico y endoscópico con argón. La técnica se realizó en quirófano con anestesia regional. Se realizaron controles clínicos y endoscópicos.
ResultadosVeinticinco varones (73,5%) y 9 mujeres (26,5%), con una edad media de 69 años (32–80) presentaron rectorragia por proctitis actínica y precisaron ingreso. En 6 pacientes (28,5%) fracasaron todos los tratamientos y se empleó formaldehído al 4%. La respuesta a la hemorragia fue completa en los 6 pacientes, 3 casos con una sesión y otros 3 con 2 sesiones. En 4 pacientes se empleó la técnica de la gasa y en otros 2 (por presencia de estenosis) enema de formaldehído al 4%. En 2 pacientes apareció dolor como complicación principal (33,3). La mediana de seguimiento ha sido de 60 meses (rango intercuartílico 26 a 67 meses).
ConclusionesEl formaldehído al 4% en la hemorragia por proctitis actínica es una técnica eficaz, fácilmente reproducible y con poca morbilidad.
The stable central position of the rectum in the pelvis makes radiation proctitis a frequent complication caused by radiotherapy of pelvic and perineal organs, fundamentally prostate or uterine neoplasms. Acute lesions are usually self-limiting, but between 5% and 10% of patients can present chronic proctitis. This may present with different clinical symptoms: an inflammatory syndrome (pain, tenesmus, urgency, diarrhea, etc.), hemorrhage, and in rare cases, stenosis, fistulas or septic symptoms. Chronic lesions are irreversible and progressive, basically translating into arteritis obliterans and interstitial fibrosis of the entire rectal wall1,2 (Fig. 1).
Hemorrhage due to chronic proctitis can usually be managed with topical treatments (steroids, sucralfate, salazopyrin, etc.). Nonetheless, bleeding that is difficult to control may occur. After the failure of topical treatments, endoscopic techniques using argon, the hyperbaric chamber or formaldehyde are the most widely used. Surgery is the last resort as it is accompanied by important morbidity and is usually mutilating.
We present the experience of treatment of hemorrhage due to refractive radiation proctitis using 4% formaldehyde in a colorectal surgery unit.
Patients and MethodsA retrospective, descriptive study of a cohort of patients with severe radiation proctitis admitted to the Hospital Universitario in Donostia, Spain between 2003 and September 2009 was performed. Patients who were considered to have severe affectation had been diagnosed with radiation proctitis and required hospitalization for the control of their symptoms. All the patients were diagnosed with colonoscopy and presented a level III3 Haas severity index. Biopsy was only used selectively when there was a doubt regarding a possible malignancy. Initially, topical treatment was initiated with corticoid enemas, sucralfate, salicylates and therapeutic endoscopy with argon plasma coagulation. The most refractive cases were remitted to our Unit and treated with topical application of 4% formaldehyde. The technique was carried out in an operating room with hyperbaric local anesthetic and in the lithotomy position with protection of the anoderm and perineum with a 0.2% nitrofural ointment. Using anoscopy or rectoscopy, a gauze dressing that had been soaked in a 4% formaldehyde solution was inserted and placed on the affected areas for 2–3min intervals. Afterwards, the rectum was rinsed with saline solution. In cases of bleeding with rectal stenosis that impeded manipulation with a rectoscope, 4% formaldehyde enemas were applied for 3min followed by abundant saline rinsing. The patients were followed-up in the outpatient clinic and colonoscopy was repeated 6 months later. Anorectal function was evaluated by interviewing the patient and with physical examination.
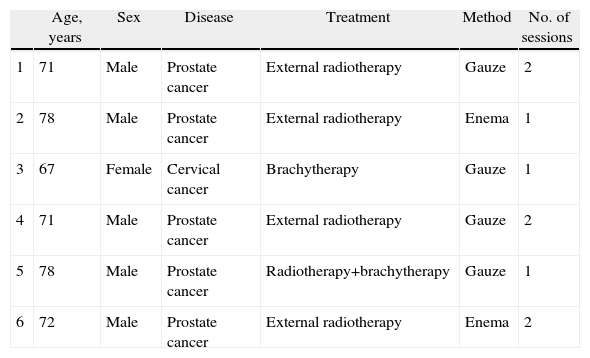
ResultsTwenty-five men (73.5%) and 9 women (26.5%) with a mean age of 69 (32–80) presented rectal bleeding due to radiation proctitis that required hospitalization. Two patients presented with rectoprostatic and rectovaginal fistulas and another 2 with rectal syndrome. Endoscopy was performed in all patients and biopsy was taken in only 5 cases (due to suspected recurrence of the original disease). The primary tumors were: 25 prostate (73.5%), 4 endometrial (11.8%), 3 cervical (8.8%) and 2 vaginal (5.9%). Sixteen patients received external RT (47.1%), 15 RT+BT (44.1%) and 3 BT (8.8%). All received some type of topical treatment: 17 corticosteroids (50%), 10 sucralfate (29.4%) and 7 salazopyrin (20.6%). In 21 patients, argon plasma was used (61.7%). In 6 patients (28.5%), all treatments had failed and 4% formaldehyde was used (Table 1). The response to treatment was complete in the 6 patients: 3 cases after one session, and the other 3 after 2 sessions (in one patient, 3 weeks after the first treatment). In 4 patients, the gauze technique was used; meanwhile, in another 2 (due to stenosis) a formaldehyde enema was used. In 2 patients, the main complication was pain (33.3%), which was treated with NSAIDS and remitted over the course of 2–3 weeks (one patient treated with gauze dressing and another with enemas). Six months later, follow-up colonoscopies were performed in the 6 patients treated with formaldehyde, and no complications or side effects were detected. Mean follow-up was 60 months (RI 26–67 months). All patients presented acceptable rectoanal function and there was no recurrence of hemorrhage during the follow-up period (Table 2).
Characteristics of the Patients Treated.
| Age, years | Sex | Disease | Treatment | Method | No. of sessions | |
| 1 | 71 | Male | Prostate cancer | External radiotherapy | Gauze | 2 |
| 2 | 78 | Male | Prostate cancer | External radiotherapy | Enema | 1 |
| 3 | 67 | Female | Cervical cancer | Brachytherapy | Gauze | 1 |
| 4 | 71 | Male | Prostate cancer | External radiotherapy | Gauze | 2 |
| 5 | 78 | Male | Prostate cancer | Radiotherapy+brachytherapy | Gauze | 1 |
| 6 | 72 | Male | Prostate cancer | External radiotherapy | Enema | 2 |
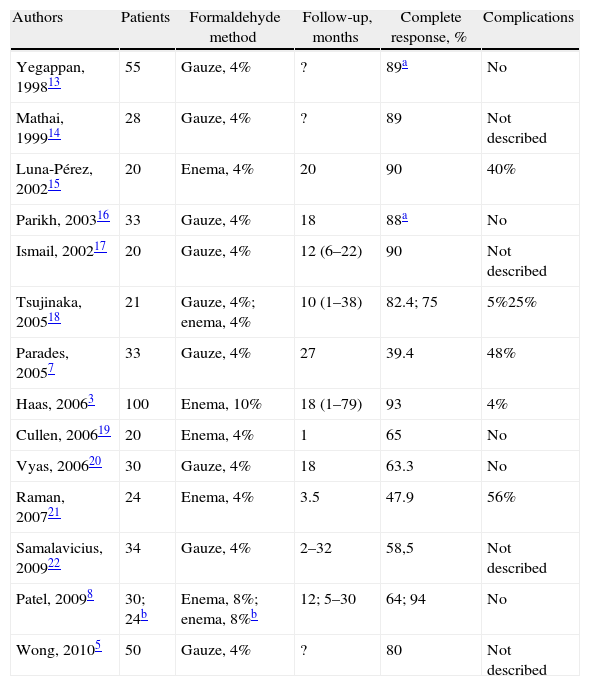
Main Series of Treatments With Formalin (More Than 20 Patients).
| Authors | Patients | Formaldehyde method | Follow-up, months | Complete response, % | Complications |
| Yegappan, 199813 | 55 | Gauze, 4% | ? | 89a | No |
| Mathai, 199914 | 28 | Gauze, 4% | ? | 89 | Not described |
| Luna-Pérez, 200215 | 20 | Enema, 4% | 20 | 90 | 40% |
| Parikh, 200316 | 33 | Gauze, 4% | 18 | 88a | No |
| Ismail, 200217 | 20 | Gauze, 4% | 12 (6–22) | 90 | Not described |
| Tsujinaka, 200518 | 21 | Gauze, 4%; enema, 4% | 10 (1–38) | 82.4; 75 | 5%25% |
| Parades, 20057 | 33 | Gauze, 4% | 27 | 39.4 | 48% |
| Haas, 20063 | 100 | Enema, 10% | 18 (1–79) | 93 | 4% |
| Cullen, 200619 | 20 | Enema, 4% | 1 | 65 | No |
| Vyas, 200620 | 30 | Gauze, 4% | 18 | 63.3 | No |
| Raman, 200721 | 24 | Enema, 4% | 3.5 | 47.9 | 56% |
| Samalavicius, 200922 | 34 | Gauze, 4% | 2–32 | 58,5 | Not described |
| Patel, 20098 | 30; 24b | Enema, 8%; enema, 8%b | 12; 5–30 | 64; 94 | No |
| Wong, 20105 | 50 | Gauze, 4% | ? | 80 | Not described |
The prevalence of chronic radiation proctitis varies from 5% to 10%. Hemorrhage is the most frequent complication (80%), which is resolved in most patients with topical treatments (corticoids, sucralfate, salazopyrin, etc.). Nevertheless, a recent systematic review has reported the absence of quality evidence to define which method is best.4
The treatment of rectal hemorrhage due to severe radiation proctitis with 4% formaldehyde is a simple, safe and effective technique that is an alternative in cases of failure with topical or endoscopic treatments.
In 1969, Brown described the use of formalin in post-radiotherapy cystitis, and Rubinstein introduced it in the treatment of proctitis in 1986.5
There are 2 techniques for applying formaldehyde: the traditional method with enemas and the gauze dressing technique developed by the Singapore group in 1993.6 We have used both, with no clear differences in efficacy. Nevertheless, caution must be taken with the use of enemas in the presence of stenosis due to the risk of retention of formaldehyde and local consequences due to absorption.7
Although the solution most often used is 4%, as in our series, formaldehyde solution at 8% and 10% has also been used, but with no clear advantages.4 Haas used the gauze dressing technique at 10% in an outpatient setting with a success rate of 70% and no complications. However, they included patients with variable severity and none had had previous treatment.3
More than 30% of patients require several treatment sessions. In our cases (selected due to their recurrence), a second treatment was necessary in 3 out of 6 patients. Patel et al., in a retrospective, controlled non-randomized study in 64 patients, found that the use of vitamin A improved results (94% of responses vs 64%) and reduced the number of sessions.8
The use of formaldehyde, at any concentration and with either technique, is not free of risks and the complications are variable (from 2% to 50%). Formaldehyde is a sclerosing agent that produces a chemical cauterization of the blood vessels of the mucosa. Pain, as in our case, is the most frequent complication, although it is generally self-limiting and affects one out of every 3 patients.7,9 Patients may present with diarrhea, transitory incontinence, rectal ulcerations, stenosis and even perforation. Saclarides10 comments that cases of incontinence or stenosis are more related with the use of retractors (in a very ischemic territory) than with the drugs used. It is very important to respect the contact times (less than 3–4min) and to finish the procedure with abundant saline rinsing. Recently, the Mount Sinai group has published the first two cases of anorectal carcinoma after treatment with topical formalin in a series of 49 patients,11 which demonstrates the rarity of this risk.
A recent prospective study with 12 patients has evaluated the use of an irrigation solution of water combined with oral antibiotics (ciprofloxacin and metronidazole), which was successful in 11 patients with no morbidity. In addition, 5 of them had had previous treatments with formalin and they preferred the new therapy.12
Treatment with 4% formaldehyde for hemorrhage due to radiation proctitis is an effective technique that is easily reproducible and has little morbidity, although it should be reserved for severe cases that are unresponsive to topical pharmacological or endoscopic treatments.
Conflict of InterestsThe authors declare no conflict of interests.
Please cite this article as: Placer C, et al. Proctitis actínica, hemorrágica crónica y refractaria. Experiencia con formaldehído al 4%. Cir Esp. 2013;91:111–4.