In December 1966, the first pancreas transplant ever was performed at the University of Minnesota. R. Lillehei and W. Kelly, transplanted a kidney and a pancreas in a diabetic patient on dialysis, getting function of both organs. Since then, the technical and immunological advances in this transplant have resulted in graft and patient survival results as the rest of the abdominal solid organ transplants. The balance of these 50 years is that more than 50,000 diabetic patients have been transplanted in more than 200 centers around the world. In our country the first transplant was performed 34 years ago in Barcelona and now 12 centers perform about 100 transplants per year. Although advances in diabetes control have been very important, pancreas transplantation continues to be the only method that allows normalization of the carbohydrates metabolism to improve the quality of life and, above all, to increase the survival of these patients.
En diciembre de 1966 se realizó en la Universidad de Minnesota el primer trasplante de páncreas de la historia. R. Lillehei y W. Kelly, trasplantaron un riñón y un páncreas a una paciente diabética en diálisis, consiguiendo función de ambos órganos. Desde entonces los avances técnicos e inmunológicos en este trasplante, han propiciado resultados en cuanto a supervivencia del injerto y del paciente superponibles al resto de los trasplantes de órganos sólidos abdominales. El balance de estos 50 años es que mas de 50.000 pacientes diabéticos han sido trasplantados en mas de 200 centros en todo el mundo. En nuestro país el primer trasplante se realizó hace 34 años en Barcelona y ahora 12 centros realizan alrededor de 100 trasplantes por año. Aunque los avances en el control de la diabetes han sido muy importantes, el trasplante de páncreas continúa siendo el único método que permite normalizar el metabolismo hidrocarbonado, mejorar la calidad de vida y sobre todo aumentar la supervivencia de estos pacientes.
Last December 17th was the 50th anniversary of the first pancreas transplantation in the history of medicine (12/1/1966).1
We should be reminded that, in the 1960s, the clinical application of organ transplantation was initiated in patients whose diseases had been irreversible until that time. The advent of organ transplantations was a wake-up call that definitively propelled the development of important technical and immunological advances. The era was one of social controversy as well as incredible technological development, culminating in the Space Race and man landing on the Moon in 1969.
Kidney transplantation had been developed before this wave of innovations, thanks to the vision and persistence of Hume, Kuss and, especially, Murray and Merrill who, at the Peter Bent Brigham Hospital in Boston, had successfully performed the first kidney transplantation between 2 twin brothers in 1954. These advances, made fundamentally in the US, were due to the willingness of a series of hospitals, whose objective was the clinical application of organ transplantation after many years of research programs. Liver (1963), lung (1963), heart (1967), pancreas (1967) and colon (1967) transplants and a group of pioneers including Starzl, Calne, Sunway, Barnard, Hardy, Lillehei, Kelly, Murray and Najarian blazed a trail that many surgeons throughout the world have later followed.2
For a long time, pancreas transplantation was considered the Cinderella of solid organ transplants. As the objective was to cure diabetes though the normalization of carbohydrate metabolism, it took a while to comprehend that, in order to substitute only 2% of insulin-producing pancreas cells, it was necessary to transplant the entire pancreas, which involved technical and immunological problems. Furthermore, the availability of insulin for the control of diabetes meant that many doctors did not adequately contemplate the deterioration caused by the disease, even with apparently good metabolic control.
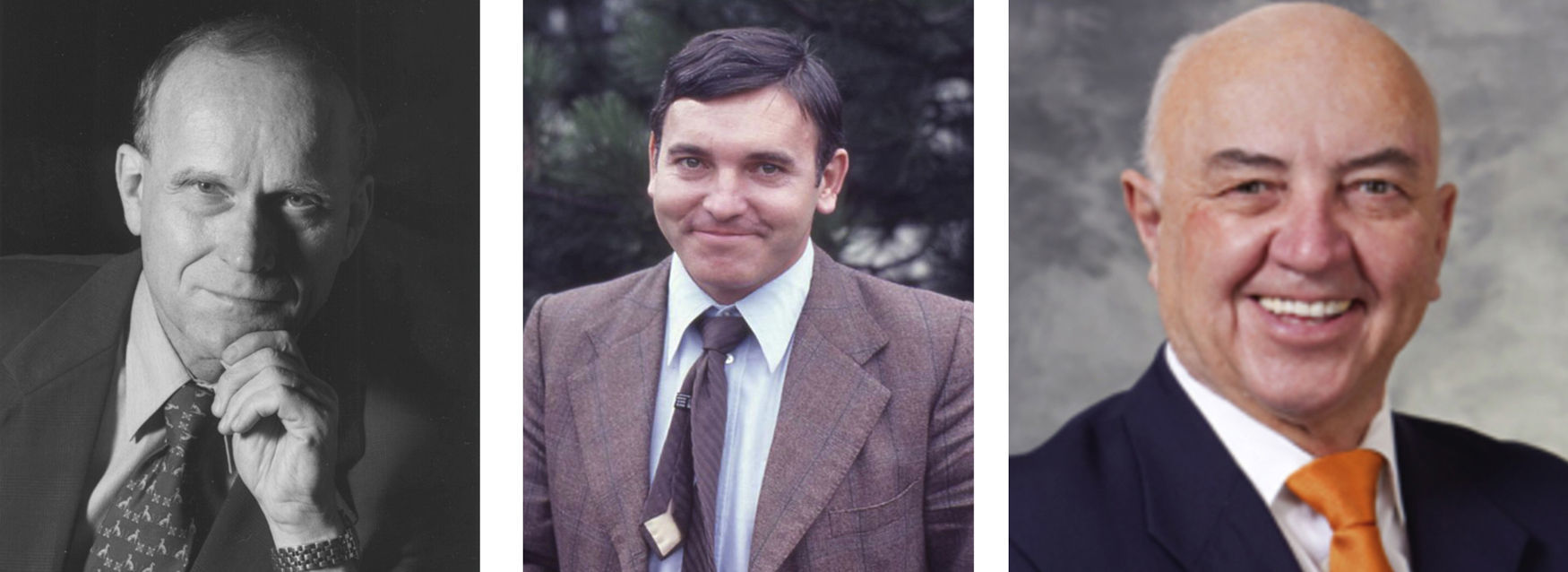
The University of Minnesota in Minneapolis is a prestigious hospital with a long tradition of clinical research thanks to a group of physicians who, under the leadership of Professor Wangensteen, were able to develop the first experiences in cardiac surgery thanks to Varco and the Lillehei brothers. Richard Lillehei, who had consolidated an important research program in shock, postulated that a pancreas transplant could be the solution for those patients with diabetes and kidney failure who, until that time, were practically given up on by medicine. Lillehei and Kelly, 2 surgeons with independent laboratories and research fellows, joined forces and, together with the diabetologist Goetz, made the unheard of decision to simultaneously perform kidney and pancreas transplantations in a 28-year-old patient who had been diabetic since the age of 9 and who presented end-stage renal disease. This transplantation, led by Kelly and assisted by Lillehei and Merkel, was done at the Mayo Memorial Hospital in Minneapolis, by the prestigious Surgery Department headed by Wangensteen.1
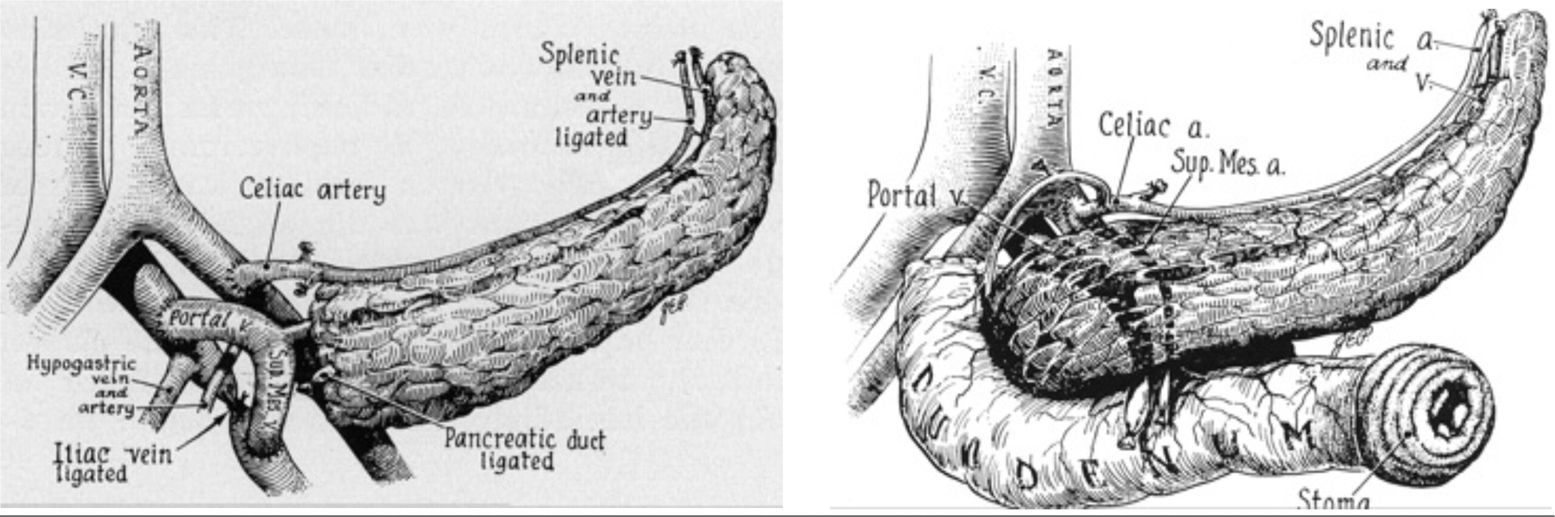
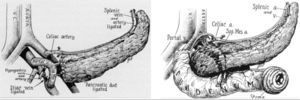
The pancreas transplant consisted of a segmental graft with the pancreas duct ligated. This patient remained insulin free for 6 days; however, after this period, insulin was required, probably related with the high doses of steroids necessary to try to avoid rejection. Likewise, the patient developed pancreatitis of the graft, possibly due to the duct ligation, and on February 14, 1967 Kelly and Lillehei removed the pancreas graft; the kidney was rejected shortly thereafter. The recipient died due to pulmonary embolism 13 days after the transplantectomy (Fig. 1).
This first case is an example of the morbidity that was associated with pancreas transplantation for many years: surgical complications, infections and rejection. In spite of this complicated first case, the Minnesota team demonstrated the technical possibilities of this transplantation. Prior to clinical application, Merkel had developed in the laboratory of Dr. Kelly a canine model of segmental pancreas transplantation, trying to reduce exocrine secretion by graft radiation.3,4 Meanwhile, in the laboratory of Dr. Lillehei, another 2 surgical fellows, Largiader from Zurich and Idezuki from Tokyo, worked on a canine pancreatic-duodenal transplant model, with drainage of the exocrine secretion by means of Roux-en-Y duodenojejunostomy.5,6 With this new surgical model, Lillehei led the second pancreas transplantation on the morning of New Year's day (1/1/1967). This transplant functioned for 4.5 months, with excellent follow-up of both organs. Acute rejection was controlled with high doses of prednisone, although in the end the rejection episodes affected the duodenum. After the first case, another 12 were carried out by the same team until 1973, using a complete pancreas-duodenum graft in most, with intestinal diversion of the exocrine secretion through a percutaneous duodenostomy. In this series of transplants, 9 were associated with kidney transplantation and 4 were isolated pancreas transplantation7,8 (Fig. 2).
The majority of the transplants functioned immediately, but the rejection—given the empirical immunosuppression of the time (azathioprine and corticosteroids)—and the surgical complications were reasons that influenced the loss of enthusiasm in this type of transplants. Lillehei performed the last of the transplantations of the series on January 11, 1973.9 Najarian, new director of the department since July 1967, had participated in some of the transplant surgeries with Lillehei and, as a result of the complications entailed, decided to manage the program with the aim to perform a less aggressive approach for the treatment of diabetes and kidney failure in these patients. New members of the team like Simmons and Kjellstrand developed an important kidney transplant program in uremic diabetic patients, and Sutherland initiated clinical research in islet transplantation.10,11
After the first pancreas transplants at the University of Minnesota in 1968, other hospitals in South America carried out 4 transplantations (Río de Janeiro, 1 case; Sao Paulo, 2 cases; and Buenos Aires, 1 case), although only in 1 was insulin independence temporarily achieved.12,13 In 1969, another 2 institutions in the US had experiences with pancreas transplantations: at the University of Colorado, Merkel and Starzl performed one case of simultaneous kidney and pancreas transplantation,14 and a second case at the University of California, at the Irvine Medical Center, under Connolly.15 In Europe, the first pancreas transplantation was conducted at the Guy's Hospital in London by Bewick in 1972.16
Until 1970, only 25 pancreas transplantations had been done at 6 institutions worldwide. Two-thirds of these experiences were conducted simultaneously with renal transplantations. Out of all these cases, only one case in the Lillehei series functioned for one year.
In November 1971, Gliedman performed his first transplant at the Montefiore Hospital in New York, diverting the exocrine secretion through an anastomosis of the Wirsung duct with the native ureter. With this technique, this group carried out 11 transplantations in the 1970s, with one case that functioned for 22 months and another for 50 months.17 In 1976, Bewick, once again at the Guy's Hospital in London, conducted a pancreatic transplantation technique leaving the duct open. Another similar case at the University of Minnesota done by Sutherland functioned with insulin independence for 18 months: at that time, it was the case with the longest graft survival.16,18
Until 1980, only 105 pancreas transplantations had been carried out across the world, half of which had been done in the US, with active programs in Minnesota and the Montefiore Hospital in New York. The other half had been performed in Europe, where the most active programs were at the Huddinge Hospital in Stockholm (Sweden), headed by Groth, and at the Eduard Herriot Hospital in Lyon (France), headed by Dubernard (Fig. 3).
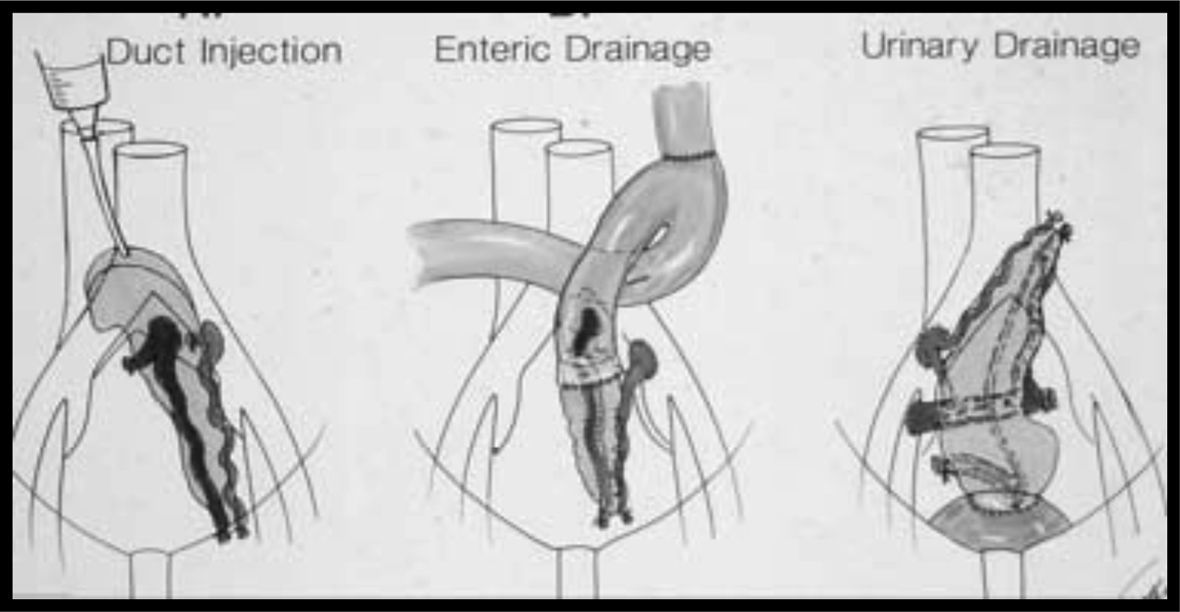
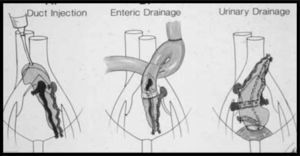
In 1978, Dubernad had developed a new technique, injecting a polymer in the pancreatic duct (Fig. 3A) to try to induce fibrosis and abolish the exocrine secretion and, therefore, the complications dependent on the exocrine pancreas. The success of this ingenious technique encouraged other surgeons to utilize different polymers in the pancreatic duct, such as prolamin, used by Land in Munich, polyisoprene, used by MacMaster in Cambridge, and silicone, used by Sutherland at the University of Minnesota.19–21
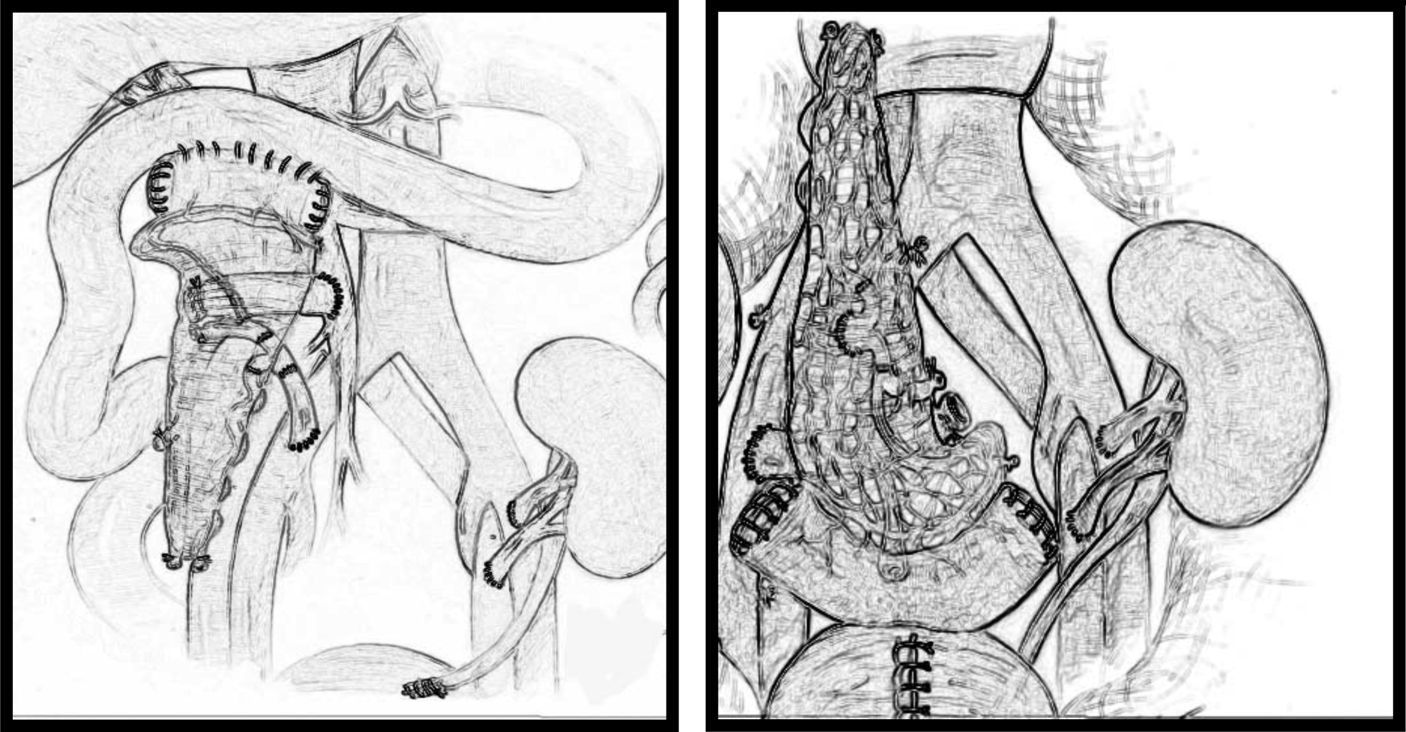
In the 1980s, at the University of Minnesota, Sutherland developed a major pancreas transplantation program with live donors using segmental grafts, whereas in transplants from cadaveric donors, the model used was a pancreas-duodenal graft with intestinal bypass.22–24
In 1983, Sollinger, a German surgeon who went to the University of Wisconsin to work with Beltzer, followed the experiences of Gliedman in New York and developed with good results a bladder diversion technique for exocrine secretions using anastomosis of the pancreas segment to the bladder. This technique was perfected by Corry and Ngheim at the University of Iowa, utilizing the bladder diversion of the entire pancreatic-duodenal graft by means of anastomosis of the duodenum with the bladder (Fig 3C).25–27
With this technique, in addition to a significant decrease in surgical complications, it was possible to measure urine amylase levels as a marker of rejection (Prieto).28 Therefore, bladder diversion was the choice in many programs in the 1990s. Despite this, urinary complications (urethritis, hematuria, metabolic acidosis, urinary fistula, etc.) caused some hospitals to reconvert many patients to intestinal diversion.
Simultaneously, at the University of Pittsburgh in 1984, Starzl had started a transplant program that returned to the original technique described by Lillehei using intestinal drainage. Likewise, the Stockholm group (Groth and Tyden) had already successfully developed intestinal diversion with a segmental graft (Fig. 3B).29–31
Encouraged by the improved results, at other medical centers in the US and Europe, pancreas transplantation programs were successfully initiated with variations of certain technical aspects related with the type of graft, the exocrine secretion diversion model and venous drainage of the graft.
From the standpoint of immunosuppression, Calne was the first to apply cyclosporine to pancreas transplantations at Cambridge,32,33 and Sutherland introduced quadruple therapy, including induction therapy.34 Starzl was the first to introduce tacrolimus in this transplant in 1989,35 and in the mid-1990s mycophenolate mofetil was introduced by Sollinger.36
From a technical standpoint, the diversion used in the decade of the 1990s was urinary, whereas in the decade of 2000 the diversion was intestinal (Fig. 4).
Since then, more than 50,000 diabetic patients have received transplants at more than 200 medical centers worldwide, with one-year patient survival rates of 95% and graft survival rates greater than 85%.37 The improvement of the results has been progressive thanks to a better knowledge of the particularities of this transplant type in all its stages, from appropriate early indication to meticulous technique and, especially, the application of a more effective regimen of immunosuppressants. The results are registered with the International Pancreas Transplant Registry (IPTR), founded by Sutherland, who has been a University of Minnesota surgeon and alma mater in the world in this type of transplant for more than 30 years.38,39
In Spain, the first pancreas transplantation was performed on February 3, 1983 by Dr Gil Vernet and Dr Fernandez-Cruz at the Hospital Clínico y Provincial in Barcelona.40 Dr. Gil Vernet had already performed the first successful kidney transplantation in our country and was very much aware of the trends in transplantation originating in other European countries and the US. Therefore, it was reasonable for this pioneer of renal transplantation in Spain, together with a young Fernández-Cruz (also a surgeon at the Hospital Clínico in Barcelona) to initiate this combined kidney and pancreas transplantation program. Professor Fernández-Cruz had done an internship at the University of San Diego in the US. He had also visited Dr. Sutherland in Minneapolis and started the program that has been a leader in our country ever since.
The donor of this first transplant was a 17-year-old boy, who had died as a result of a car accident; the recipient was a 32-year-old patient with type I diabetes on renal dialysis for kidney failure. The technique used was a kidney transplant in the left iliac fossa, and a segmental pancreas transplantation with obliteration of the duct using prolamin in the right iliac fossa. The patient survived 11 years and died of myocardial infarction. The nephrology team was comprised of Dr. Caralps and Dr. Andreu.41
After this experience, other centers in Spain, including Córdoba (Hospital Reina Sofía), Santander (Hospital Marqués de Valdecilla), Santiago de Compostela (Hospital Universitario), Málaga (Hospital Carlos Haya), Madrid (Hospital 12 de Octubre), Tenerife (University of the Canary Islands), etc., started pancreas transplantation programs. At present, there are 12 medical centers that have active programs that perform about 100 transplants per year.42,43
In 2005, a consensus meeting was organized by the National Transplant Organization in Spain. Following a debate among the parties involved (surgeons, nephrologists, endocrinologists, transplant coordinators), the criteria for indication, prioritization, organ distribution, hospital planning and accreditation mechanisms were established in order to optimize the treatment of diabetes in our country.44–46
After 50 years of history, we can say that pancreas transplantation has come a long way since its inception, thanks to the work of pioneering surgeons who have gone beyond conventional practice in the search for solutions to the complications of diabetes.
The complexity of diabetic patients means that the benefits of these transplants are sometimes underestimated when compared with other procedures, such as cardiac transplantation or liver transplantation, in which graft function acquires vital connotations. However, today, pancreas transplantation has the same results in terms of patient survival, graft survival and quality of life as other solid organs (Figs. 4 and 5).
As long as we do not have procedures for the prevention of diabetes, the solution for diabetic patients with risk of secondary complications will entail the replacement of functioning islet tissue by transplantation. Answers for this substitution are likely to involve cell transplantation in the future, but it is unquestionable that, after 50 years of progress, the fulfillment of these objectives involves vascularized pancreas transplantation. The clinical project initiated by Lillehei and continued by Sutherland and hundreds of enthusiasts came of age years ago, but it is time to pay homage to all those who dedicated part of their professional lives to try to improve the survival and quality of life of these patients (Fig. 6).
The author has no conflict of interests to declare
Please cite this article as: Casanova D, en nombre de Grupo Español de Trasplante de Páncreas. Trasplante de páncreas: 50 años de experiencia. Cir Esp. 2017;95:254–260.