Acute aortic occlusion (AAO) is a rare disease with high morbidity and mortality. The aim of this study was to describe the results of surgical treatment of acute aortic occlusion and risk factors for mortality.
MethodsRetrospective review of the clinical history of 29 patients diagnosed and operated on for AAO during 28 years. The following variables were analysed: age, sex, tobacco use, diabetes, chronic renal insufficiency, chronic heart failure, atrial fibrillation, arterial hypertension, symptoms, diagnosis and treatment, 30-day mortality and long-term survival. A univariant analysis was performed of variables related to mortality.
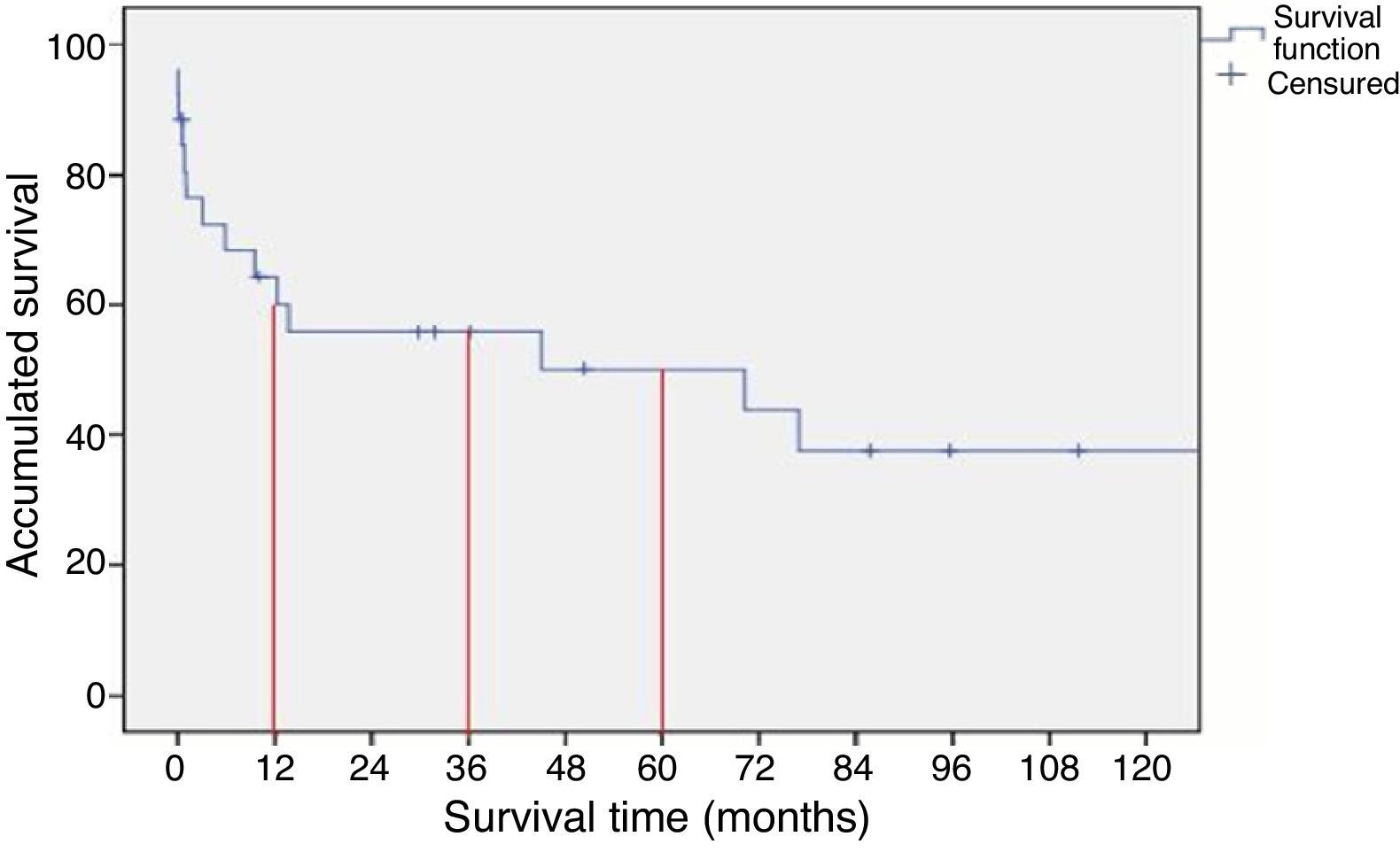
ResultsTwenty-nine patients were included (18 male) with a mean age of 66.2 years. The aetiology was: embolism (EM) in 11 cases and Thrombosis (TR) in 18 cases. The surgical procedures performed included bilateral transfemoral thrombectomy (14 cases), aorto-bifemoral by-pass (8 cases), axilo uni/bifemoral by-pass (5 cases) and aortoiliac and renal tromboendarterectomy (2 cases). Morbidity included: renal failure (14 cases), mesenteric ischaemia (4 cases), cardiac complications (7 cases), respiratory complications (5 cases) and loss of extremity (2 cases). The in-hospital mortality was 21% (EM 0%, TR 21%). The estimated survival at 1.3 and 5 years was 60, 50 and 44% respectively. Age (P=.032), arterial hypertension (P=.039) and aetiology of the AAO (P=.039) were related to mortality.
ConclusionsAcute aortic occlusion is a medical emergency with high mortality rates. Acute renal failure is the most common postoperative complication.
La oclusión aórtica aguda (OAA) es una patología infrecuente con una alta morbimortalidad. El objetivo del estudio fue describir los resultados del tratamiento quirúrgico de la oclusión aórtica aguda y factores de riesgo de mortalidad.
MétodosSe revisaron retrospectivamente las historias clínicas de 29 pacientes diagnosticados e intervenidos por OAA durante 28 años. Se recogieron las variables edad, sexo, tabaco, diabetes, insuficiencia renal crónica, insuficiencia cardiaca, fibrilación auricular, hipertensión arterial, síntomas, diagnóstico y tratamiento, mortalidad a 30 días y supervivencia a largo plazo. Se analizó mediante análisis univariante que factores se relacionaban con la mortalidad.
ResultadosSe incluyeron 29 (18 varones), con una media de 66,2 años. La etiología fue: embolia (EM) en 11 casos y trombosis (TR) en 18 casos. Los procedimientos quirúrgicos realizados incluyeron trombectomía transfemoral bilateral (14 casos), by-pass aorto bifemoral (8 casos), by-pass axilo uni/bifemoral (5 casos) y tromboendarterectomía aortoiliaca y renal (2 casos). La morbilidad incluyó: insuficiencia renal (14 casos), isquemia mesentérica (4 casos), complicaciones cardiacas (7 casos), complicaciones respiratorias (5 casos) y pérdida de la extremidad (2 casos). La mortalidad hospitalaria fue del 21% (EM 0%, TR 21%). La supervivencia estimada a 1, 3 y 5 años fue del 60, 50 y 44% respectivamente. La edad (p = 0,032), la hipertensión arterial (p = 0,039) y la etiología de la OAA (P=,039) se relacionaron con la mortalidad.
ConclusionesLa oclusión aguda de aorta abdominal constituye una urgencia médica con elevada mortalidad. siendo la insuficiencia renal aguda la complicación más frecuente en el postoperatorio.
Acute aortic occlusion (AAO) is a rare pathology.1–6 Its actual incidence is unknown, but some authors report percentages of 1%–4%; the incidence of acute occlusion of the abdominal aorta secondary to thrombosis of an infrarenal abdominal aortic aneurysm is around 2%.3 This is associated with a high mortality rate of almost 100% in some series.1–3 It is caused by 4 basic mecanisms: embolism, in situ thrombosis, trauma or dissection.1–12 Currently, the most frequent of all is the thrombotic origin, be it in atherosclerotic patients, patients with an aneurysm or those with a hypercoagulability disorder. The diagnosis is delayed in many patients due to the frequent association with paraplegia,1–4,6 which worsens prognosis. Although trauma can be a cause, there are only isolated case reports.1,5 The objective of this study was to describe our experience in the treatment of acute aortic occlusion in a vascular surgery and angiology unit and to analyse mortality risk factors.
Patients and MethodsWe retrospectively reviewed the medical files of all patients who had been diagnosed and treated for acute occlusion of the abdominal aorta at the Hospital Universitario de Gran Canaria Dr. Negrín from 1981 to 2009. Variables collected were age, sex, tobacco habit, diabetes, kidney failure, ischaemic heart disease, atrial fibrillation, arterial hypertension, symptoms, ischaemia time, diagnosis, treatment, mortality within 30 days and long-term survival.
Statistical AnalysisThe statistical analysis was performed with SPSS 15.0 software (SPSS Inc., Chicago, IL, USA). The Fisher, Student's t and Kolmogorov–Smirnov tests were used. For the survival analysis, the Kaplan–Meier method was utilised. A univariate analysis determined which factors correlated with mortality. Patients with previous aortic surgery were excluded.
ResultsClinical CharacteristicsThe series included 29 patients (18 males and 11 females) with a mean age of 66 (range 31–91). None of the patients presented occlusion due to trauma or abdominal aortic dissection.
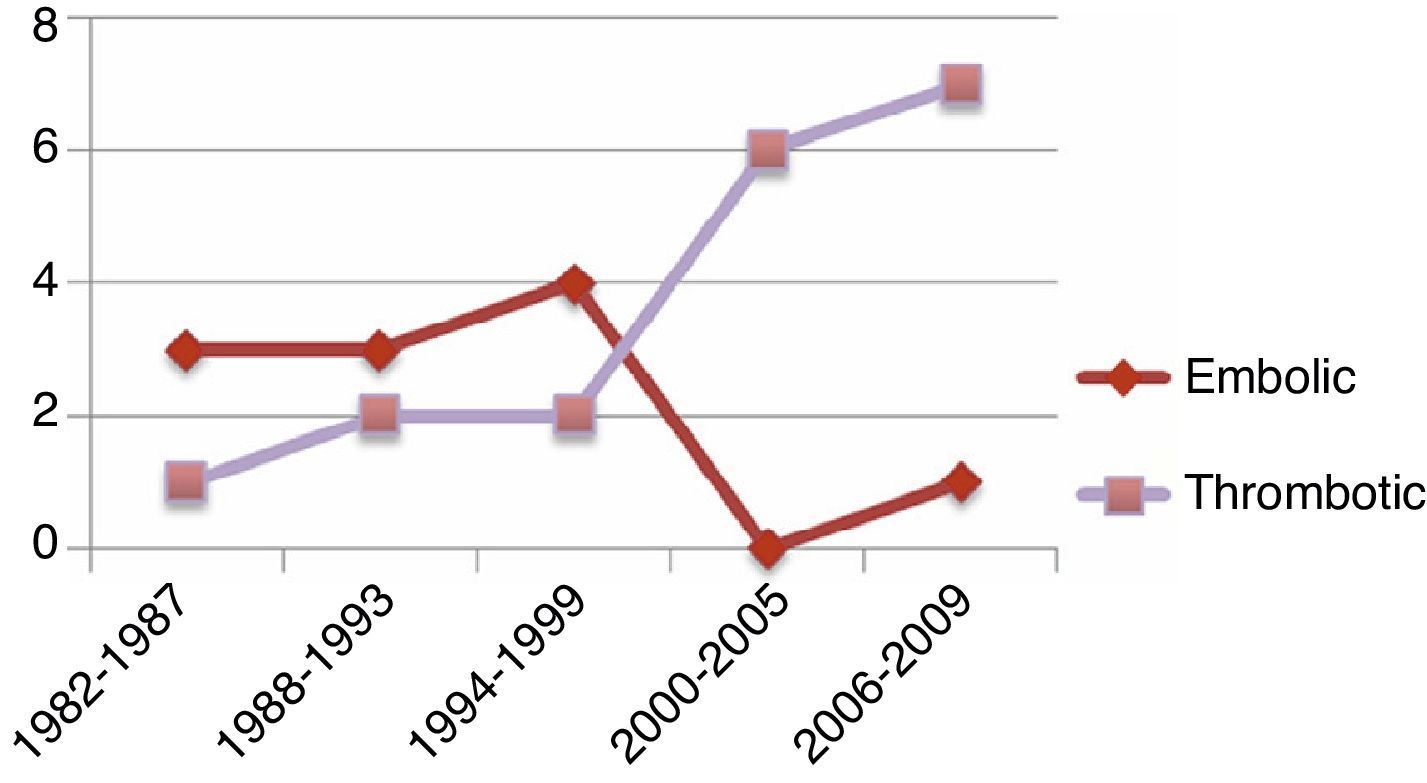
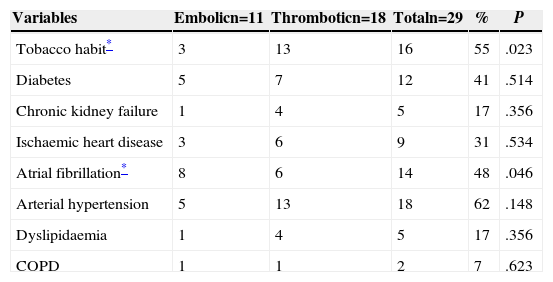
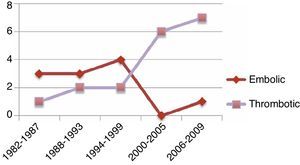
The group with embolism-related AAO was comprised of 4 males and 7 females, with a mean age of 63 (range 31–80). The 31-year-old was HIV-positive, addicted to IV drugs, and his aortic occlusion was secondary to endocarditis due to Candida Albicans (C. albicans). The most frequent underlying heart disease in this group was atrial fibrillation, followed by ischaemic heart disease. The other group with acute aortic thrombosis included 14 males and 4 females, with a mean age of 68 (range 39–91). Five male patients in this group had had previous abdominal aortic aneurysm. Three patients presented suprarenal aortic occlusion. In the patients with acute thrombosis of the abdominal aorta, we found a statistically significant difference favouring male sex (P=.033) and tobacco habit (P=.023); meanwhile, statistical significance was reached for the presence of atrial fibrillation in the patients with embolism-related aortic occlusion (P=.048) (Table 1) (Figs. 1 and 2).
Associated Cardiovascular and Respiratory Risk Factors.
| Variables | Embolicn=11 | Thromboticn=18 | Totaln=29 | % | P |
|---|---|---|---|---|---|
| Tobacco habit* | 3 | 13 | 16 | 55 | .023 |
| Diabetes | 5 | 7 | 12 | 41 | .514 |
| Chronic kidney failure | 1 | 4 | 5 | 17 | .356 |
| Ischaemic heart disease | 3 | 6 | 9 | 31 | .534 |
| Atrial fibrillation* | 8 | 6 | 14 | 48 | .046 |
| Arterial hypertension | 5 | 13 | 18 | 62 | .148 |
| Dyslipidaemia | 1 | 4 | 5 | 17 | .356 |
| COPD | 1 | 1 | 2 | 7 | .623 |
X2 alpha: 0.05; COPD: chronic obstructive pulmonary disease.
Symptoms data collected included the presence or absence of sensorimotor alterations, pain in the lower extremities and/or abdominal pain. No statistically significant differences were found between the two groups. Symptoms, when present, were bilateral, and in some patients one extremity predominated over the other. Sensory alterations were experienced by 83% of patients, followed by pain in the lower extremities in 76%, altered mobility in 73% and abdominal pain in 14%.
Only one patient had had less than 6h of ischaemia at the time of surgery. In 10 patients, less than 24h had transpired, and 18 patients had more than 24h of ischaemia, 10 of which had surgery in the following 24h. The remaining 8 patients had ischaemia times of more than 48h.
Imaging Studies and TreatmentTwenty-three patients underwent arteriography, 4 patients had computed tomography (CT) and 4 patients from the embolic group were not studied with imaging techniques.
In the series, 14 patients were treated by means of embolectomy or bilateral transfemoral thrombectomy (11 embolic group/3 thrombotic group). Four patients underwent axillobifemoral bypass due to previous abdominal surgery, history of heart disease and advanced age. In the remaining patient, axillo-unifemoral bypass was used due to supracondylar amputation with no femoral pulse that had been previously identified. Aortobifemoral bypass was performed in 8 patients, and the 2 remaining underwent aortoiliac and renal thromboendarterectomy.
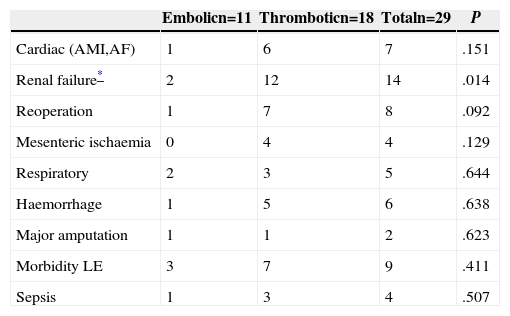
MorbidityThe incidence of complications in the groups with embolism-related aortic occlusion was lower than in the thrombosis group, 3 patients had acute myocardial infarction in the postoperative period, 2 patients debuted with atrial fibrillation; one episode of heart failure was registered as well as one angina.
Acute kidney failure (at varying degrees) was the most frequent complication, and 10 patients required transitory dialysis, which was statistically significant in favour of the thrombotic origin group versus the embolic origin group (P=.014).
Eight patients were reoperated on: 3 due to haemorrhage, 3 for acute ischaemia of the lower extremities and 2 due to mesenteric ischaemia. There were 2 pneumonias, one COPD re-exacerbation, one acute respiratory distress and one pneumothorax. The morbidity of the lower limbs included fasciotomy and plexopathy, as well as one patient with lymphorrhagia and inguinal wound dehiscence in the thrombotic group (Table 2).
Postoperative Morbidity.
| Embolicn=11 | Thromboticn=18 | Totaln=29 | P | |
|---|---|---|---|---|
| Cardiac (AMI,AF) | 1 | 6 | 7 | .151 |
| Renal failure* | 2 | 12 | 14 | .014 |
| Reoperation | 1 | 7 | 8 | .092 |
| Mesenteric ischaemia | 0 | 4 | 4 | .129 |
| Respiratory | 2 | 3 | 5 | .644 |
| Haemorrhage | 1 | 5 | 6 | .638 |
| Major amputation | 1 | 1 | 2 | .623 |
| Morbidity LE | 3 | 7 | 9 | .411 |
| Sepsis | 1 | 3 | 4 | .507 |
AMI: acute myocardial infarction; AF: atrial fibrillation; LE: lower extremities.
Mortality in the first 30 days was 21%. Six patients in the in situ aortic thrombosis group died during the postoperative period, while none did in the embolic AAO group, a statistically significant difference (P=.039). Four patients with axillobifemoral bypass died: 2 due to multiple organ failure, one hypovolemic shock and another secondary to acute myocardial infarction. One patient from the aortobifemoral bypass group died due to acute myocardial infarction plus multiple organ failure, and another patient died due to hypovolemic shock after aortoiliac and renal thromboendarterectomy.
Risk factors were analysed for associations with hospital mortality. No statistically significant relationship was found between mortality and ischaemia time, which was categorised in 3 groups: less than 6h, between 6 and 24h and more than 24h (P=.865). A statistically significant association was found with age, HTN and thrombotic aetiology (P=.032, .039 and .039, respectively) (Table 3).
Thirty-Day Mortality.
| Variables | 30-day mortality (%) | P |
|---|---|---|
| Age* | .032 | |
| Sex (male/female) | 62/38 | .592 |
| Tobacco habit | 55 | .565 |
| Diabetes mellitus | 41 | .513 |
| Chronic kidney disease | 17 | .269 |
| Ischaemic heart disease | 31 | .257 |
| Atrial fibrillation | 48 | .291 |
| Arterial hypertension* | 62 | .039 |
| Aneurysm | 17 | .731 |
| COPD | 7 | .623 |
| Aetiology* (embolism/thrombosis) | 38/62 | .039 |
| Renal morbidity | 48 | .070 |
| Cardiac morbidity | 24 | .455 |
| LE morbidity | 35 | .302 |
COPD: chronic obstructive pulmonary disease; LE: lower extremities; X2 alpha: 0.05.
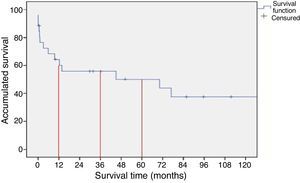
After surgery, the 30-day mortality rate was 21%; by the end of the first year, accumulated mortality reached 40%. Survival rates after 1, 3 and 5 years were 60, 50 and 44%, respectively (Fig. 1).
DiscussionInitial published series reported that embolism-related AAO was the most frequently observed type.2–4,6 Even though the presentation of our patients coincided with preceding series, in the last decade this tendency has changed and currently in our series thrombus-related AAO is more frequent (Fig. 2). We believe that this is explained by the discovery and continuous use of anticoagulants in patients with cardiac arrhythmias in the 1990s, the decline in rheumatic valvular heart disease due to the use of prophylactic antibiotics, and the improvements in antiplatelet drugs with the advent of clopidogrel in July 1998. In conjunction with the lower mortality rates after an acute coronary event, there has been a global increase in the survival rate of atheromatous patients related to cardiovascular mortality. This, over time, could result in an increase of thrombotic aetiology as a cause of acute occlusion of the abdominal aorta.
Most patients arrive at the Emergency Department with varying degrees of ischaemia of the lower extremities, characterised by affected sensitivity and/or mobility, accompanied by the absence of bilateral femoral pulse. Nonetheless, in our series, as in the case of other reviewed series, diagnosis was delayed in many patients due to the inadequate clinical approach that many authors attribute to the neurological deficit that is often present.1–4,6 Abdominal AAO should be considered in the differential diagnosis of all patients with sudden-onset neurologic deficit affecting the lower extremities.1
The diagnosis of abdominal AAO is made with proper physical examination and imaging tests to evaluate the location, distribution and extension of the occlusion in order to plan a treatment strategy.1–10 In all the series we have reviewed, there is a small number of patients in whom the cause of acute aortic thrombosis is the presence of an abdominal aortic aneurysm, generally smaller than 5cm.1,3 Our series includes 5 patients, 3 of which were treated with aortobifemoral bypass and 2 of which underwent axillobifemoral bypass. Only one of these 5 died, due to acute myocardial infarction after aortobifemoral graft. In comparison, the other series have 2 or fewer cases of AAO due to thrombosis of an aneurysm.1,3,4
In addition, 3 patients presented suprarenal thrombosis of the aorta, one of whom died from multiple organ failure. The other series do not include any similar cases, and in the literature there are only reports of isolated cases.7
Diagnosis with imaging tests, including CT, arteriography and ultrasound, has evolved with technological advances. In the past, patients were diagnosed by means of aortogram, and during surgery it was not uncommon to find a thrombosed infrarenal aneurysm causing the AAO. Today, CT plays a fundamental diagnostic role as it is available in practically all hospitals, is not time-consuming, is not technician-dependent, and helps plan the treatment strategy while establishing the area of the arterial occlusion and providing information about the characteristics of the region to be revascularised (arterial diameter, presence of plaque and characteristics), anatomical variations (horseshoe kidney, vena cava agenesis), or the diagnosis of neoplasms, free fluid or other alterations.
Ultrasound is a diagnostic imaging test available at all hospitals. In expert hands, it provides much information about the possible aetiology and location of the occlusion. However, it has limitations as it is technician-dependent and patients have generally not fasted, or are obese, present an accumulation of gases, or do not tolerate decubitus. We therefore prefer not to lose time and usually order a CT.
After CT or arteriography, the aetiological origin should be identified: embolic (patients with no history of peripheral artery disease, young patients and/or underlying arrhythmia) or thrombotic (elderly patients, with ischaemic heart disease, or dehydrated patients, underlying neoplasm, etc.). If an embolic origin is suspected, the indication is clear: bilateral transfemoral embolectomy. But, if a thrombotic origin is suspected, the classical indications include aortobifemoral and axillobifemoral bypass.1,3,4,6 In most series, there is a group of patients with initial bilateral transfemoral thrombectomy with good results. Evidence of this is seen in our series, with 3 transfemoral thrombectomies; this can be explained by analysing the causes of death in our series, where 4 patients had undergone axillobifemoral and the remaining 2 direct aortic access.
In cases of thrombosis, some authors prefer direct aortic access, while others only perform axillobifemoral bypass.1–3
Therefore, the question is whether to perform an initial transfemoral thrombectomy in all patients, or at least the patients with greater baseline morbidity, in whom there is no concomitant aneurysm. If this is not possible, an axillobifemoral bypass would be indicated. Even though the permeability is inferior, it is the best option in those patients with serious underlying cardiopathy, advanced age or previous abdominal surgery. Another option is aortobifemoral graft; while it is aggressive surgery that not all patients are able to withstand, it has a high rate of permeability.1
None of the patients of our series received fibrinolysis as part of their treatment, although in the literature there are reports of cases treated satisfactorily, especially for patients with healthy arteries, absence of embolic cause or aneurysm.9,10
Preparation prior to the procedure includes anticoagulation, hydration and monitoring in a critical care unit. Anticoagulation avoids the propagation of the thrombus and the thrombosis of the vascular bed. This is fundamental in patients coming from hospitals where there is no vascular surgeon who therefore need to be transferred to a reference hospital, but it could be avoided in patients who are to be treated with direct aortic access and the operating room is available. All patients should undergo transthoracic or transoesophageal echocardiogram in order to rule out a cardiac origin of the occlusion.3 If the patient has been operated on without previous imaging studies, abdominal ultrasound or CT should be done in patients with thrombectomy or bilateral transfemoral embolectomy in order to rule out the presence of an aneurysm. If one were detected, elective surgical treatment should be contemplated once the acute event has been resolved.
In the postoperative period, patients with embolic AAO should be administered anticoagulants to prevent the formation of thrombi that could later migrate to any region of the arterial tree and cause acute ischaemia in the extremities, supra-aortic trunks or visceral arteries. If the cause of the embolism is endocarditis, we should remember that low molecular weight heparins are contraindicated, so unfractionated heparin should be used. Patients with thrombosis of the terminal aorta should receive anticoagulants if a bilateral transfemoral thrombectomy was performed and they present lesions in the untreated terminal aorta or iliac arteries or if the hypercoagulability state or cause of the thrombosis have not been corrected.3,4,11,12
In the series by Surowiec et al., as in our series, mortality was 21% (5 embolectomies/2 thrombectomies) with a mean age of 71 and an age range from 62 to 78.3
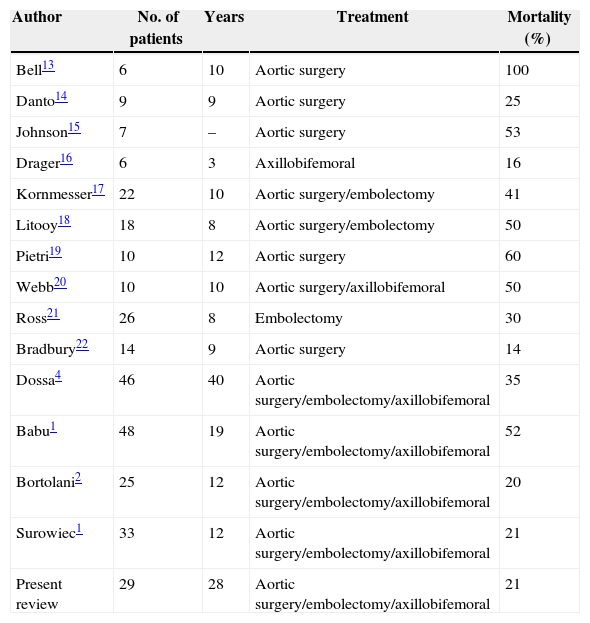
In our series, there were 6 deaths out of the 29 patients, all of which were in the thrombotic group, with a mean age of 77 and an age range from 66 to 90. If we compare this with series published to date, we see that the mortality rate of our series concurs with the best published series (Table 4).
Type of Surgical Procedure and Mortality in Previously Published Series.
| Author | No. of patients | Years | Treatment | Mortality (%) |
|---|---|---|---|---|
| Bell13 | 6 | 10 | Aortic surgery | 100 |
| Danto14 | 9 | 9 | Aortic surgery | 25 |
| Johnson15 | 7 | – | Aortic surgery | 53 |
| Drager16 | 6 | 3 | Axillobifemoral | 16 |
| Kornmesser17 | 22 | 10 | Aortic surgery/embolectomy | 41 |
| Litooy18 | 18 | 8 | Aortic surgery/embolectomy | 50 |
| Pietri19 | 10 | 12 | Aortic surgery | 60 |
| Webb20 | 10 | 10 | Aortic surgery/axillobifemoral | 50 |
| Ross21 | 26 | 8 | Embolectomy | 30 |
| Bradbury22 | 14 | 9 | Aortic surgery | 14 |
| Dossa4 | 46 | 40 | Aortic surgery/embolectomy/axillobifemoral | 35 |
| Babu1 | 48 | 19 | Aortic surgery/embolectomy/axillobifemoral | 52 |
| Bortolani2 | 25 | 12 | Aortic surgery/embolectomy/axillobifemoral | 20 |
| Surowiec1 | 33 | 12 | Aortic surgery/embolectomy/axillobifemoral | 21 |
| Present review | 29 | 28 | Aortic surgery/embolectomy/axillobifemoral | 21 |
Adapted from Babu et al.1
The amputation rate of our series was 7%, including one patient with embolic AAO and another patient with acute aortic thrombosis. In three previous series, the need for amputation varied between 6% and 16%.1,3,4
After surgery, all patients should be monitored in an intensive care unit. From the start, renal function management should be aggressive because of the deteriorated renal function of these patients and the predictable consequences that occur during revascularisation. These include acidosis, hyperkalaemia, arrhythmias and renal failure due to the release of superoxide and hydroxyl radicals from the revascularised tissue as after several hours of ischaemia.1
In the 21st century, abdominal AAO is still a medical emergency with a high mortality rate. Even so, our series had a mortality rate that was lower than expected and acute kidney failure was the most frequent postoperative complication.
CT is currently the test of choice for preoperative diagnosis and establishing the therapeutic strategy.
This review confirms that, except in thrombosed aneurysms, bilateral transfemoral thrombectomy should be the initial surgical technique for all patients.
Conflict of InterestsThe authors declare no conflict of interests.
Please cite this article as: de Varona Frolov SR, Acosta Silva MP, Volo Pérez G, Fiuza Pérez MD. Resultados del tratamiento quirúrgico de la oclusión aguda de aorta abdominal. Cir Esp. 2015;93:573–579.