The use of liver grafts from non-heart-beating donors is one of the most effective strategies for increasing the availability of organs for transplantation.1 However, its utility is limited due to the impact on the quality of the organ of the period of warm ischemia after cardiac arrest.
Ex vivo normothermic machine perfusion (NMP) can be considered a useful tool for assessing the viability of marginal organs before liver transplantation and thereby assisting in the decision-making process. The NMP method is able to evaluate post-reperfusion injury, without compromising the situation of a recipient in critical condition.
The international multi-center prospective study COPE-WP2 (in which our hospital participated) compared the effect of NMP and classic cold preservation on the prevention of preservation injury and graft dysfunction.2 The liver grafts used in this study were from brain-dead donors or type 3 non-heart-beating donors. With the experience acquired, we can confirm that the use of NMP is feasible and can improve organ quality by ostensibly reducing cold ischemia time, which is limited to bench surgery. This fact explains why NMP is especially attractive in grafts that are more vulnerable to injury caused by cold ischemia, such as type 2 non-heart-beating donation (NHBD-T2).
Although NHBD-T2 are especially important to generate liver grafts,3 their use is limited by the inferior post-transplantation results compared to those obtained with conventional donors.4–7 This determines the partial acceptance of liver grafts from NHBD-T2. In an experimental model, the use of normothermic regional perfusion (NRP) in association with NMP has been shown to be key in improved graft viability and post-transplant outcomes.8 Based on these results, our hospital has initiated a NRP+NMP protocol for NHBD-T2 grafts.9 The initial phase of this protocol is to perfuse grafts that had been discarded because they did not meet the current criteria of our hospital, while establishing trasplantability criteria for these grafts.
In the present study, we report the first case of NMP for a type 2 NHBD liver graft. The donor was a 63-year-old patient with cardiac arrest secondary to acute coronary syndrome. After being intubated and 117min of advanced CPR maneuvers, his death was declared in the emergency department by the chief physician; afterwards, the protocol for possible NHBD-T2 was initiated.
NHBD-T2 criteria and the procedures for cannulation/normothermic regional perfusion have been previously described.10 As the initial levels of transaminases exceeded the criteria considered acceptable at our hospital, the donor organ was discarded for transplantation. However, family members gave their informed consent specifically for our protocol.
The organ procurement surgery followed the steps described in other studies.10 After standard bench surgery, cannulas were inserted in the portal vein, hepatic artery, IVC and bile duct. Preparation of the NMP involved installing the disposable circuit in the machine, loaded with 500ml of colloid and 3 packed red blood cell units, and the preparation of infusion solutions (bile salts, insulin, heparin and prostaglandins). Upon initiating circulation of the perfusion liquid in the circuit, it is automatically oxygenated and warmed to a body temperature of 37°C, which are both necessary steps before the organ is placed in the machine. Once these procedures have been completed, the organ is placed in the sterile compartment of the Organometra® and connected to the machine to be perfused.
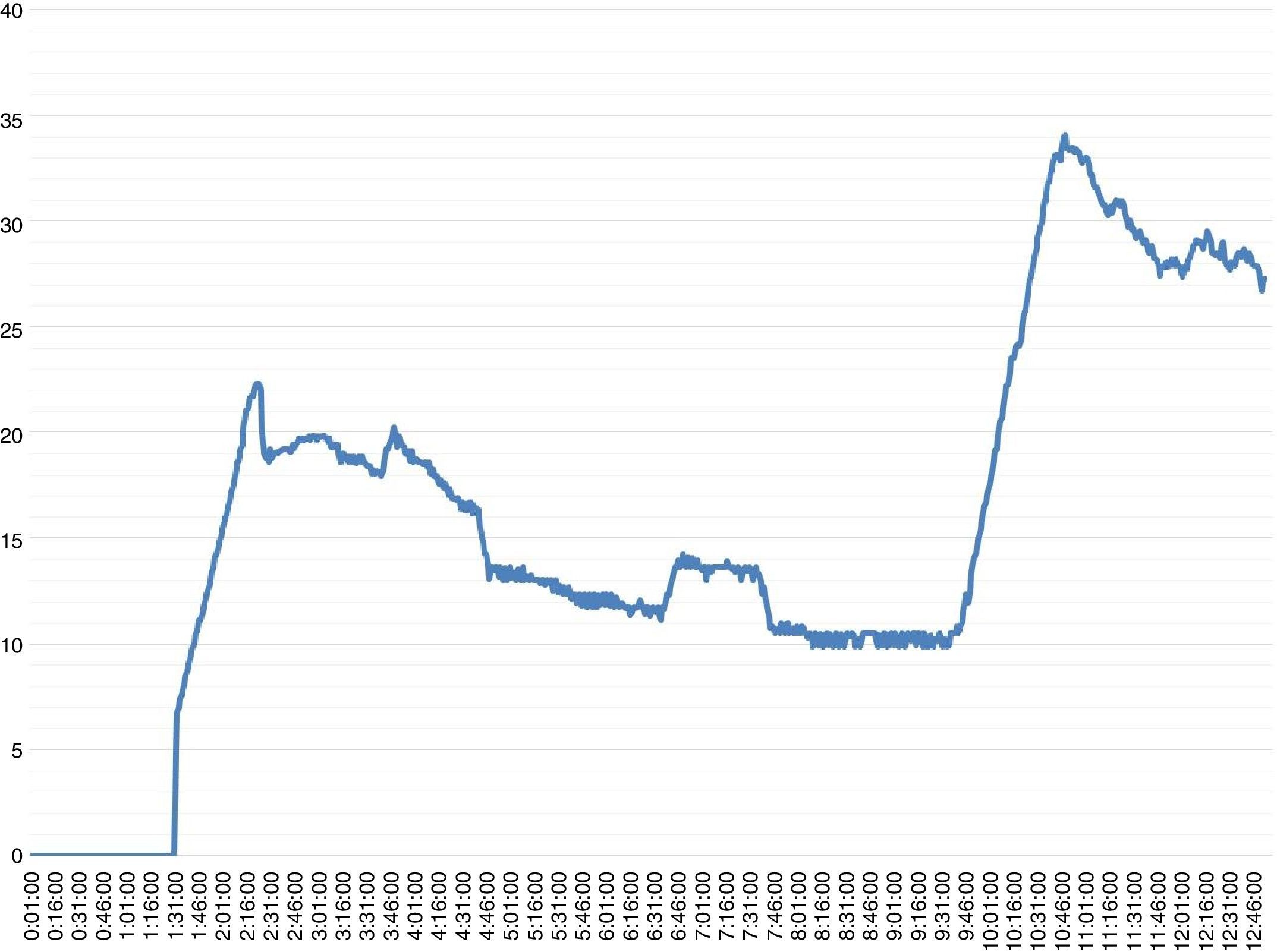
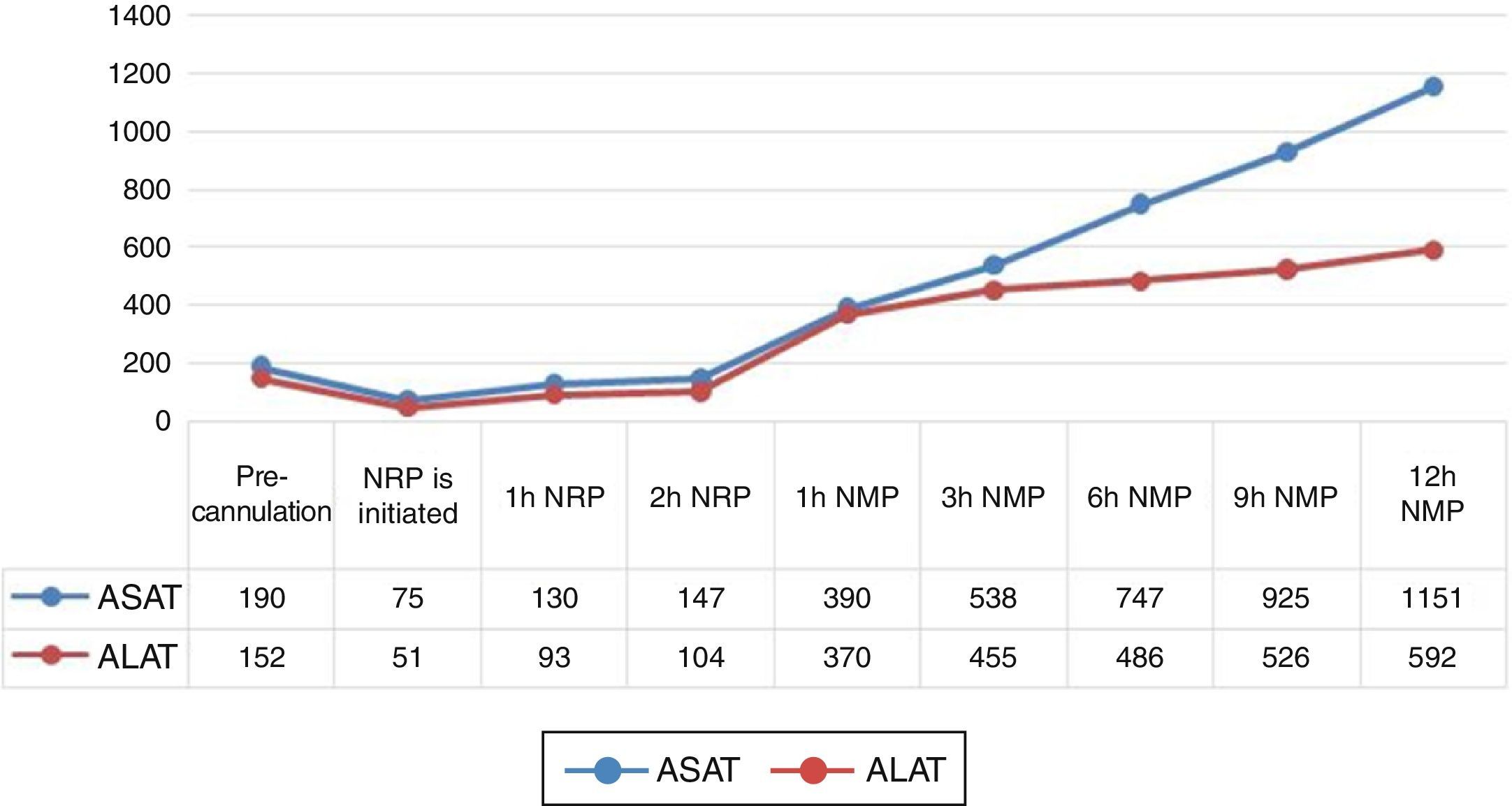
The organ perfusion duration was more than 12h. During NMP, flows through the hepatic artery and portal vein remained stable at 300mL/min and 1200mL/min, respectively, while the bile flow presented an ascending evolution to a maximum of 34mL/h (Fig. 1). The pH remained constant, with no need for correction. As for serum parameters at the end of NMP, the AST and ALT levels were 1151 and 592IU/L (Fig. 2), while the lactate presented a tendency toward improvement. The histologic analysis of the organ at the end of perfusion demonstrated minimal evidence of hepatic necrosis, with isolated foci of sinusoidal dilation and preservation of the periportal spaces.
The results of the hepatic perfusion of this present case shows that, following current criteria for graft acceptance, there may be a percentage of discarded grafts that could be rescued for transplantation. NMP would enable us to determine the intensity of post-reperfusion injury and, at the same time, it would avoid the adverse effects brought on by an additional period of cold ischemia in these grafts. The results obtained by the present study would need to be later validated by transplantation.
FundingThis research has been funded by a Caixa Bank Social Project Fund.
The authors would like to thank the IDIBAPS Biobank Department for the technical support offered.
Please cite this article as: Pavel M-C, Fondevila Campo C, Molina Santos V, Diaz Lorca A, Garcia-Valdecasas Salgado JC. Perfusión normotérmica ex vivo de injerto hepático procedente de donante en asistolia tipo 2. Cir Esp. 2017;95:301–303.