Popliteal aneurysms are the most frequent (70%–85%)1 bilateral (50%) aneurysms associated with abdominal aortic aneurysm (30%–50%).2 Surgical indication depends on their diameter (larger than 2cm), signs of atheroembolism or symptoms of external compression.3 Their natural progression is not well defined, but it has been estimated that 41% of patients with conservative treatment will develop complications in 3–5 years.4 These complications include embolisation, rupture, or limb amputation due to acute thrombosis. Open surgery involving exclusion or venous bypass is the treatment of choice.5,6 In the absence of a vein or in “hostile” legs,7 intravascular repair is an option that has been growing in popularity in recent years. We present a new technical option for the intravascular treatment of popliteal aneurysms.
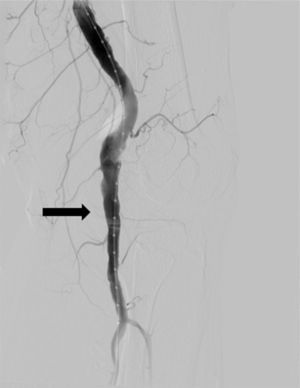
Our patient is a 64-year-old male who was seen in our office for varicose veins of the lower extremities. Physical examination was normal, except for the presence of ectactic popliteal pulses predominantly on the left side. Doppler ultrasound showed diameters of 20mm for the right popliteal artery and 25mm for the left. Computed tomography (CT) angiography detected a right aneurysm of 20mm with adequate anatomy, which we decided to exclude by means of a Viabahn® 9mm×100mm endoprosthesis (WL Gore & Associates, Flagstaff, USA). In the left lower extremity (LLE), the aneurysm surpassed the medial joint line with proximal and distal anchoring areas that were too large (10mm and 9mm, respectively) to use a conventional coated stent (Fig. 1). For these reasons, we decided to use 2 iliac extensions of Anaconda® endoprostheses (12mm×100mm proximal and 11mm×80mm distal, by Vascutek Ltd., Inchinnan, Renfrewshire, Scotland).
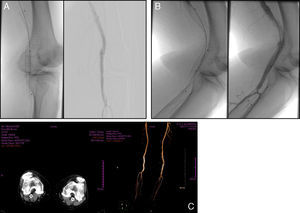
Both procedures were performed in the operating room with epidural anaesthesia. By controlling the common femoral artery and with systemic heparin (100U/kg), we proceeded with antegrade puncture using an angled-tip 0.035 hydrophilic guide wire. In the right lower limb, with a 9F introducer sheath and over a 0.035 rigid guide, the Viabahn 9mm×100mm stent was released with excellent results. Scope time was 8min. In the LLE, a 14F introducer was used and, after the placement of the rigid guide, the 11mm×80mm distal branch was released first under fluoroscopic guidance. Then, the proximal 12×100 piece was inserted, telescoped and overlapped by 2cm. Scope time was 17min and the results were excellent (Fig. 2A and B). During the 24 months of follow-up, the patient has been asymptomatic, both stents are permeable, and the popliteal aneurysms have disappeared (Fig. 2C).
There are no specific endoprostheses used for this condition. The devices used have been hand-made coated stents and coated stents for tracheobronchial disease or branch endoprostheses, initially designed for abdominal aortic aneurysm. Viabahn® stents (WL Gore & Associates, Flagstaff, USA) are often used, providing primary and secondary permeability and limb saving rates that are very close to open surgery8 as long as the anchoring areas are adequate, as in the right extremity in our patient. In the left extremity of our patient, the anchoring areas had too large of a diameter to use a conventional coated stent (10mm and 9mm, respectively); moreover, the aneurysm surpassed the medial joint line. We therefore decided to use 2 iliac branches of Anaconda® prostheses (Vascutek Ltd., Inchinnan, Renfrewshire, Scotland) that were telescoped and overlapped by 2cm (proximal 12×100 and distal 11×80). This technique provided excellent morphological results, even though the use of this device for this entity is not included in the manufacturer's instructions.
The Anaconda iliac branches seem ideal for treating popliteal aneurysms due to their low profile, precise release, flexibility and kink-resistance because of their exoskeleton. They are comprised of independent nitinol rings, as described by Cinà et al.9 in their series of 14 popliteal aneurysms treated with this device.
In the reviewed literature, exclusion and venous bypass are choice treatments, although older population age and increasing comorbidities make intravascular treatment a safe, feasible option, while always considering aspects such as: favourable anatomy, associated stenoses and distal outflow (which is occasionally reduced due to embolisation).9
In our case, venous bypass was not possible due to the large varicose veins and cutaneous trophic changes, which increased the probability of surgical wound and graft infection, as well as the risk for amputation of the extremity. In the LLE, there was additional difficulty due to the unfavourable anatomy for conventional coated stents.
This is the first case in the Spanish literature and the second case worldwide of intravascular popliteal aneurysm exclusion using the iliac branch of an Anaconda endoprosthesis. This option seems to be safe, reliable and long-lasting when the anatomy does not present adequate morphology for conventional stents, although clinical trials and long-term follow-ups are necessary.
FundingNone was received.
Conflict of InterestsNone declared.
Please cite this article as: Leiva Hernando L, Arroyo Bielsa A. Ramas iliacas de endoprótesis aórticas: otra alternativa duradera para el tratamiento de los aneurismas poplíteos. Cir Esp. 2015;93:e123–e125.