Hepatocellular carcinoma (HCC) is the most common primary liver cancer; with a worldwide incidence of more than 500000 cases per year, it is the third most common cause of cancer death.1 Although imaging tests in patients at risk of HCC have provided diagnoses in more initial stages, long-term survival rates continue to be unsatisfactory due to local and distant recurrence. HCC is a tumor with metastatic potential that is most frequently located in the lungs (60%–70%), lymph node chains (30%–40%), bones (15%–20%) and adrenal glands (8.8%–19.6%).2–4 The treatment of HCC metastases varies from resection (with a mean survival of 21.4 months) to non-surgical methods such as chemoembolization, percutaneous ethanol injection, radiotherapy, and systemic chemotherapy (with an average survival of 11.1–13.6 months).5,6
Adrenal hemorrhage is a rare complication. A narrative review by Marti et al. demonstrated that the most frequent cause of adrenal hemorrhage was pheochromocytoma (48%), followed by metastasis (20%) and adenoma (17%).7 The hemorrhagic complication of HCC metastases in this region is anecdotal, with very few cases published in the literature.7,8 Tumor growth rate, neovascularization, and tissue fragility are most likely responsible for hemorrhages secondary to HCC metastases.9
We present the case of a 63-year-old man who came to the emergency room for abdominal pain located in the left hypochondrium radiating toward the back in association with syncope. The patient reported lumbar trauma that same day due to an accidental fall. His medical history included thalassemia intermedia, liver cirrhosis secondary to hemochromatosis and atrial fibrillation. The patient had been cholecystectomized and splenectomized.
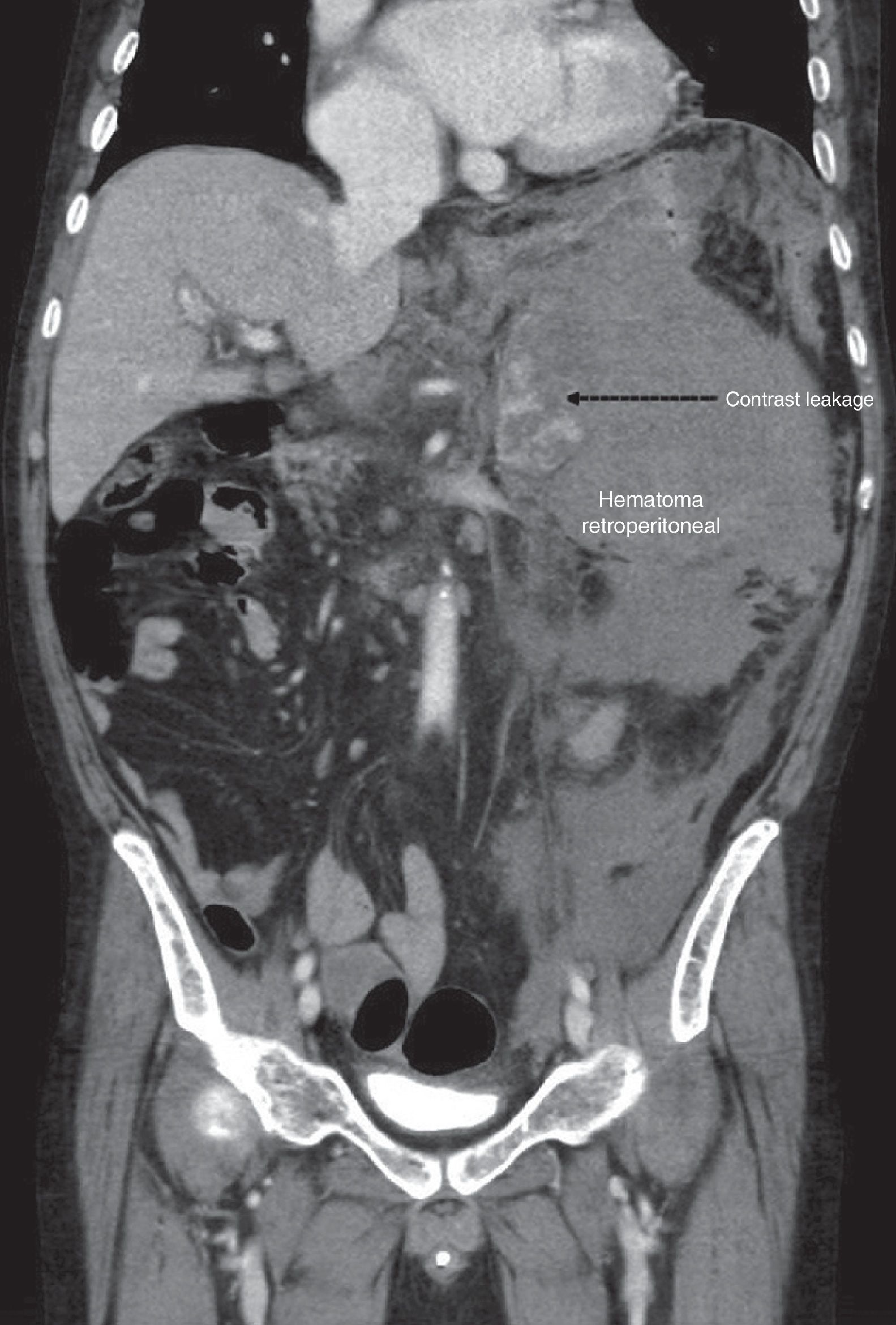
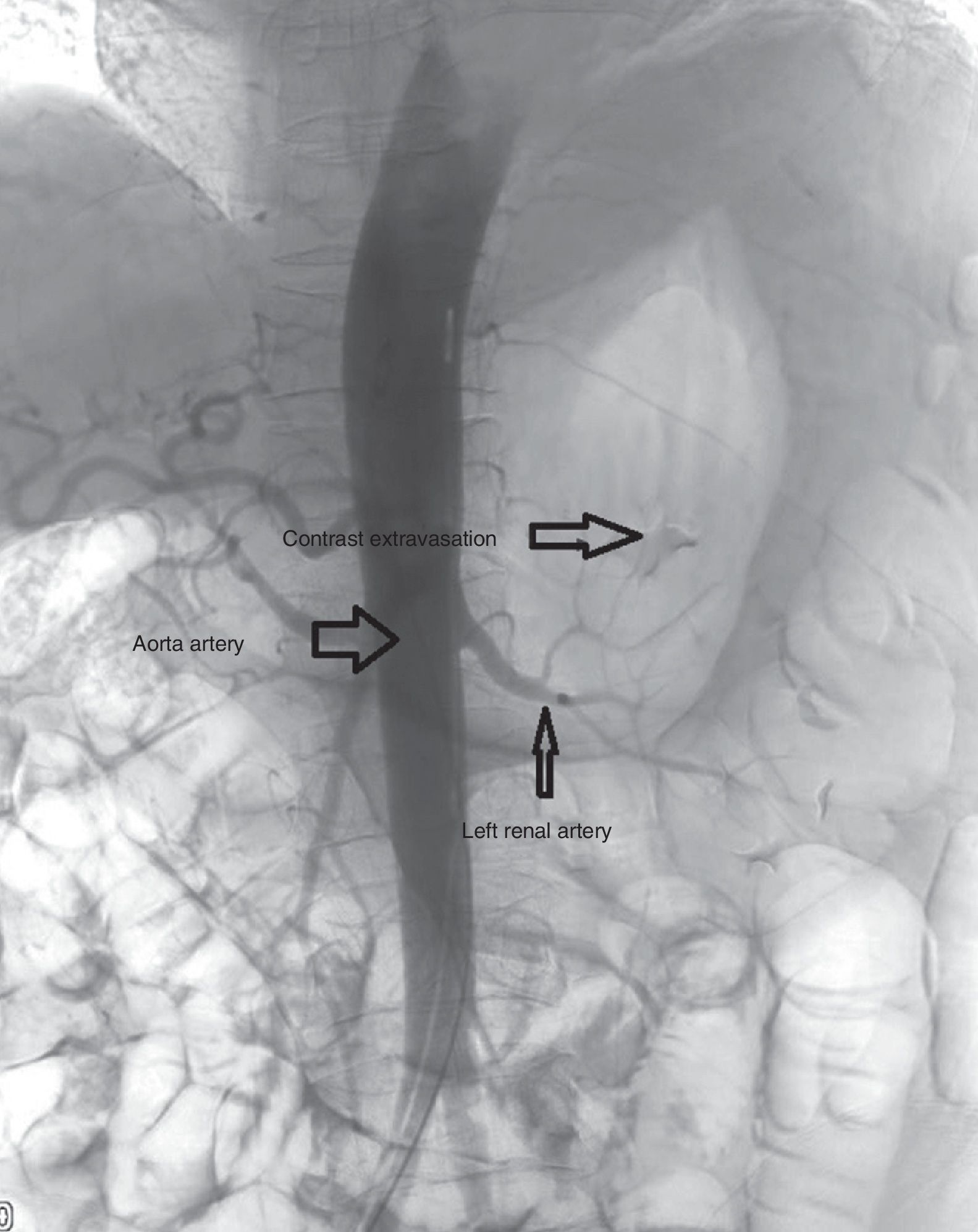
Upon arrival at the emergency room, the patient presented tachycardia and abdominal guarding. Lab work-up showed: hemoglobin 5.3mg/dL, hematocrit 16.8%, and a Quick index of 47%. Given the suspicion of acute abdomen, a computed tomography (CT) scan of the abdomen was performed, which revealed a left retroperitoneal hematoma measuring 15×10×17cm that encompassed the left adrenal gland, showed signs of active hemorrhage (Fig. 1) and displaced the pancreas and left kidney. Other findings were signs of chronic hepatopathy related to hemochromatosis and a hypodense focal lesion measuring 2.8cm in segment VIII, which possibly correlated with a focus of HCC (hypervascularization in arterial phase with early venous washout). After stabilization of the patient, arteriography was performed, where the left adrenal artery was located originating in the lateral wall of the aorta, immediately cranial to the ostium of the ipsilateral renal artery. An arterial plexus with contrast extravasation was identified, however, due to the caliber of the vessels, catheterization, and subsequent embolization were impossible (Fig. 2). Given this situation, we decided to operate with a midline laparotomy approach, observing an adrenal gland burst, which was possibly tumor-related, as well as active arterial hemorrhage, which was controlled by vascular ligatures. The gland and tumor tissue were completely resected. The patient progressed favorably, with no postoperative complications. The pathology study detected multiple fragments of brownish hematologic tissue, some of which were necrotic in appearance and classified as adrenal gland fragments invaded by an HCC. In the immunohistochemistry study, the tumor cells expressed hepatocyte and alpha-fetoprotein. The early recovery facilitated radical treatment of the HCC using radiofrequency. Currently, after more than 18 months of follow-up, the patient is free of disease.
The adrenal glands are the fourth most frequent place where HCC metastases settle. Although the treatment of choice is usually surgical, less aggressive techniques, such as radiofrequency or embolization, can be used in certain cases.6
The diagnosis of HCC metastases can be made by elevated alpha-fetoprotein levels, the appearance of new symptoms, or incidentally with imaging tests. Its diagnosis secondary to complications, such as hemorrhage as in our case, is less common. Spontaneous adrenal hemorrhage is very rare and occurs in pathological glands, especially malignant tumors, which, due to their fragile structure, cause massive bleeding that does not spontaneously subside. Retroperitoneal hemorrhage is usually seen in the context of a polytrauma patient, and it is in this type of patients that there is more management experience. Regarding retroperitoneal hemorrhage secondary to suprarenal masses, Martí et al. have described a treatment algorithm where embolization is the gold-standard technique.7 However, as Sakamoto states, emergency embolization of the adrenal glands is very difficult due to the 3 arteries that normally vascularize them.10
Adrenal rupture is rare and, when it occurs, the presence of a space-occupying lesion as an intermediate cause after trauma should be considered.
Embolization is the treatment of choice, although surgical treatment has been proven effective, and in turn serves as a treatment for adrenal metastases of HCC with good oncological results.
Please cite this article as: Silvestre-Rodríguez J, Alonso-Gómez J, Sanchez-Lauro MM, Cruz-Benavides F, Marchena-Gómez J. Estallido postraumático de metástasis suprarrenal por hepatocarcinoma. Cir Esp. 2018;96:125–127.