Eosinophilic cholecystitis is a rare entity that is diagnosed by histopathology based on the special characteristics of the inflammatory infiltrate of the gallbladder wall.1,2 Clinically, it does not present any specific symptoms or signs compared with other types of acute cholecystitis. As for the possible causes, there is no consensus, although multiple etiopathogenic hypotheses have been proposed.3–6
We present the case of a 40-year-old female patient with no known allergies to medication or prior medical history. She was studied in the outpatient clinic due to repeated episodes of biliary colic that were moderate in intensity and did not require hospitalization. Complementary tests only revealed hypercholesterolemia and moderate hypertriglyceridemia. Abdominal ultrasound confirmed the presence of cholelithiasis. With this diagnosis, the patient underwent scheduled laparoscopic cholecystectomy, with an uneventful recovery.
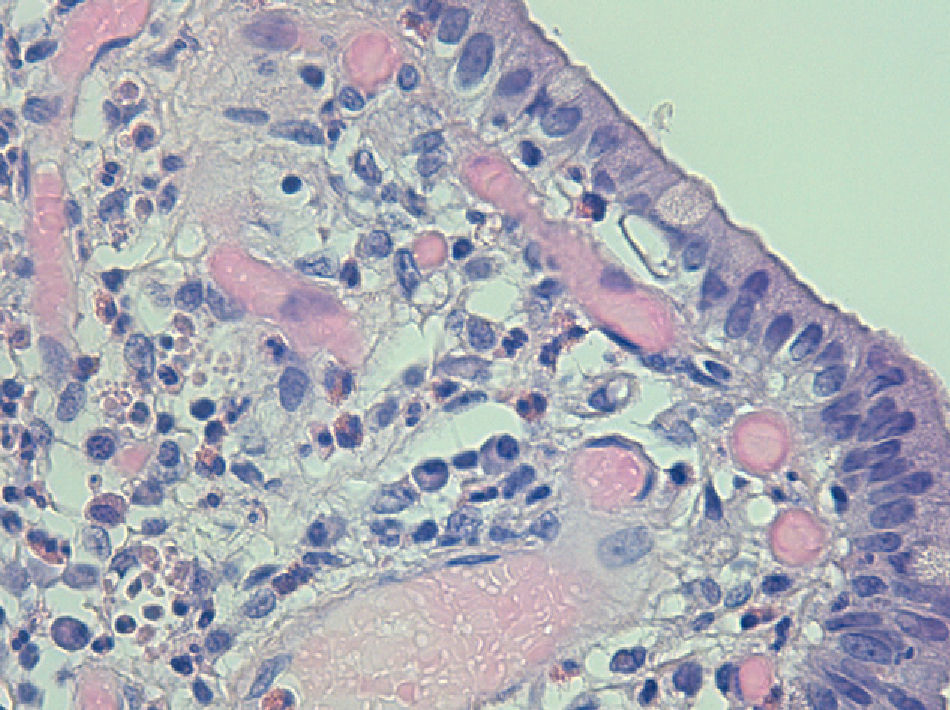
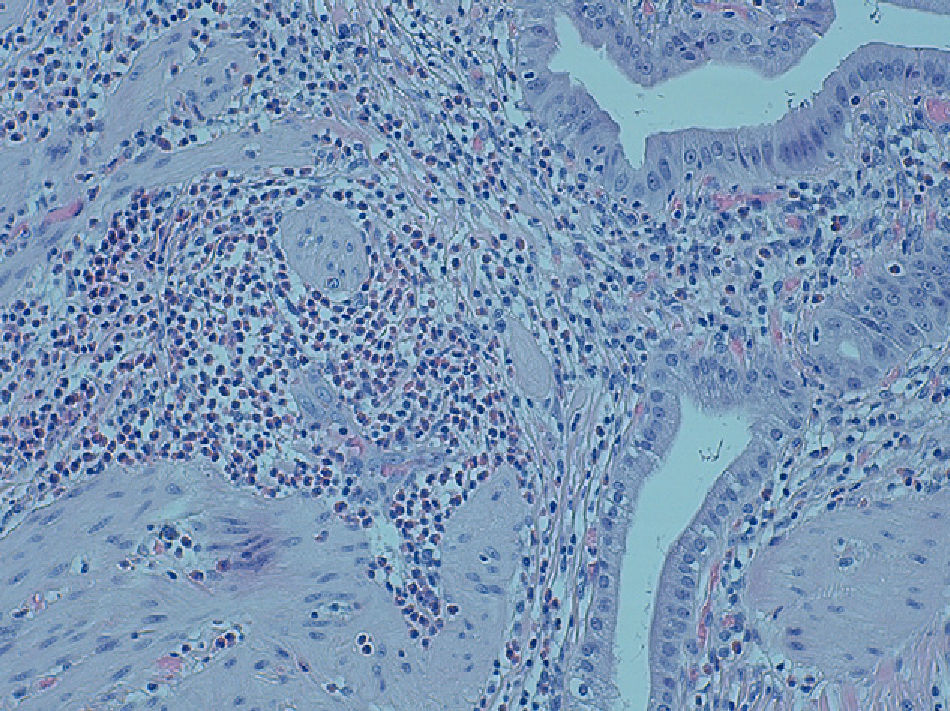
The pathology diagnosis after the analysis of the surgical specimen was eosinophilic cholecystitis (Figs. 1 and 2).
Neither in previous analyses nor in later controls were there any signs of hypereosinophilic syndrome. When we questioned the patient again, she denied close contact with animals or any consumption of medicinal plants or herbal shop products, all of which have been associated with the finding of eosinophilic cholecystitis. Nine months after surgery, the patient continues to be asymptomatic.
Eosinophilic cholecystitis is an entity that was reported for the first time in 1949; the diagnosis is histopathologic and requires the presence of an inflammatory infiltrate of the gallbladder wall with a predominance of eosinophils above 90%.1 There are cases in which this predominance is not as striking; these are known as lymphoeosinophilic cholecystitis.2
The frequency described in series of cholecystectomies ranges between 0.5% and 6.4%,2 although in most studies it does not surpass 1%,7,8 and therefore its finding is considered exceptional. In our own series of 450 cholecystectomies in the period of one year, the only case found is this case that we report, representing an incidence of 0.2%.
The physiopathological mechanism has not been clarified due to the infrequency of this disease. It has been postulated that the variability of the infiltration of the gallbladder wall by different populations of inflammatory cells could be related with the time transpired from the onset of symptoms and the cholecystectomy. This hypothesis was ruled out in the study published by Dabbs,2 which did not demonstrate a significant relationship between the pattern of gallbladder inflammatory infiltrate and the time of surgery. Given the relationship with isolated cases of hypereosinophilic syndromes and other syndromes with affected patches of the digestive tract, mediated by eosinophilic infiltration of the tissues, some type of chemotaxis by the organs has been proposed, although this mechanism has not been clearly characterized.4 Currently, the most widely accepted theory is the triggering of an idiosyncratic allergic reaction against an antigen present in the bile.2,3,5,6
Based on the possible relationship with an allergen or with the possibility that the symptoms of cholecystitis develop as part of a more extensive syndrome, some authors propose conservative management, withdrawing the triggering agent and administering anti-inflammatory treatment.
In general, it is understandable that eosinophilic cholecystitis should not be considered an entity per se because clinically it presents as cholecystitis without specific symptoms, signs or laboratory data, and it should be considered a histologic finding after cholecystectomy. It is necessary to discover the relationship that may exist with other types of hypereosinophilic syndromes or eosinophilic gastroenteritis with a prognosis and management other than cholecystectomy, and when given the persistence of digestive symptoms in patients with this finding, other underlying diseases should be ruled out.9,10
Please cite this article as: Cerdán Santacruz C, Martín Antona E, Martín García-Almenta E, Díez Valladares L, Torres García AJ. Colecistitis eosinofílica tras colecistectomía electiva por colelitiasis. Cir Esp. 2013;91:460–461.