Treatment for anal fistulas in patients with Crohn's disease is still challenging, even for the expert surgeon. The advancement flap technique is characterized by the preservation of the anal sphincter complex.
MethodsA systematic review of the literature, selecting series of patients affected by Crohn's disease and anal fistulas and treated using advancement flap technique was performed. Patients followed during at least 6 months have been included.
ResultsFrom 128 initial studies, 11 studies were selected, including overall 135 patients. Those studies show low-level evidence. Results in a series with follow-up from 8.4 to 82 months, stated a clinical success of 66% and recurrence rate around 30%. However there was an evident heterogeneity of results.
ConclusionThe review concludes that the advancement flap technique to treat anal fistulas in patients with Crohn's disease is an adequate alternative. New studies are necessary to provide higher-level evidence.
La técnica de colgajo de avance endorrectal es una de las alternativas en el tratamiento de la fístula anal en pacientes con enfermedad de Crohn.
MétodosDiseñamos una revisión sistemática de la literatura, seleccionando estudios que incluyeron a pacientes afectos de enfermedad de Crohn y fístula anal tratados mediante esta técnica. De esos estudios solo se seleccionaron los pacientes seguidos durante al menos 6 meses.
ResultadosSe seleccionaron 11 estudios con un total de 135 pacientes. Los resultados, con seguimientos de 8,4 a 82 meses, indicaron una curación del 66% y una tasa de recurrencia de alrededor del 30%. Sin embargo, se observó importante heterogeneidad en los resultados de las series revisadas.
ConclusionesEl colgajo de avance endorrectal es una alternativa adecuada en los pacientes con fístula anal y enfermedad de Crohn. Sin embargo, es necesario desarrollar nuevos estudios que aporten un mayor nivel de evidencia científica.
The surgical management of anal fistulae is a real therapeutic challenge.1 Although most patients present anal fistulae that can be treated with a fistulotomy technique, providing satisfactory results in terms of recurrence and short-term and long-term functional problems (fecal incontinence), there are patients with complex anal fistulae that require techniques to preserve the anal sphincter complex.2 This situation is especially difficult in patients with Crohn's disease. There are different surgical options to reportedly preserve the sphincter complex, such as the endorectal advancement flap and the LIFT technique, or the use of plugs, fibrin sealants and even stem cells.3
Crohn's disease can frequently present perianal involvement, in many cases with the appearance of very complex fistulae4 and a clinical scenario that can become particularly difficult to manage surgically. Once the treatment of the underlying disease has been carried out with an existing drug (for example, anti-TNF), the controversy lies in which type of surgical technique should be used in these patients to treat the anal fistula.5
Among all the technical alternatives, the endorectal advancement flap has been shown to be an appropriate treatment for patients with anal fistulae in this clinical situation.6 However, although there is scientific evidence of its usefulness in cryptoglandular anal fistulae,7 there are still few results about the use of this technique in patients with Crohn's disease.
The objective of this study was to systematically review the literature in order to determine the clinical results published for the surgical treatment of anal fistulae in patients with Crohn's disease using the endorectal advancement flap technique.
MethodsStudy DesignA study protocol was designed to conduct a systematic review of the literature, following standardized methods of analysis and eligibility in accordance with the PRISMA8 and QUORUM9 guidelines, also using the new reporting elements derived associated with PRISMA (harms checklist 2016).10
Search Strategy and Selection CriteriaStudy CharacteristicsThe characteristics and objective of the study were defined using a methodology following the PICO scheme. The definitions of the search terms were inclusive to promote a search for studies that reported clinical results in series of patients with Crohn's disease, in whom the endorectal advancement flap technique had been performed (also called “mucosal flap,” “mucosal-muscle flap” or “total thickness”) to treat primary or recurrent perianal fistulae.
PopulationInclusion CriteriaMESH-type search terms were used, including: patients over 18 years of age, of either sex, with a confirmed diagnosis of Crohn's disease and perianal disease in the form of an anal fistula. The specific search terms were: “anal fistula,” “Crohn's disease” and “advancement flap.” Likewise, an iterative focus by cross-reference was necessary to ensure that all terms in common use were incorporated into the search strategy.
Exclusion CriteriaPatients previously treated with resections of the rectum of any magnitude or etiology were excluded from the published series. Some studies presented results in patients with perianal fistula of different etiology (cryptoglandular origin and Crohn's disease), of which only those of the interest group were included. When these data could not be separated by groups, the study was considered not eligible for inclusion. A minimum population sample was not considered necessary for the eligibility of the study, but a minimum clinical follow-up of 6 months after surgery was required.
Sources of Information (Bibliographic Search)The main authors conducted a detailed search of the literature, including all articles published before March 6, 2017 using the PubMed, Spanish Medical Index, Cochrane Library and Scopus bibliographic databases. The search terms used a sensitive combination of population terms, interventions and keywords.
Variables StudiedThe studies were eligible if they provided extractable data about the clinical benefits of the technique (cure rates). The studies needed to report fistula recurrence data, defined as the clinical reappearance (and in some cases with radiological verification by MRI or endoanal ultrasound) of the lesions during the follow-up period. For the evaluation of the complications derived from the surgical intervention, we contemplated postoperative fecal continence data and the need to perform a stoma during the follow-up of these patients, following similar previous studies.7
Study TypesOur review only included studies with a full text in English or Spanish. Only studies that reported clinical data from patient series were eligible for review, regardless of whether they were descriptive or analytical studies, or with prospective or retrospective data collection. For this reason, literature review articles, editorials, letters and other forms of secondary expert opinion were excluded from the final selection of articles. Only full text studies were eligible. Thus, abstracts, conference proceedings or incomplete documents were also excluded from the search. No restriction was imposed based on the level of scientific evidence. This decision was made with the knowledge that the vast majority of the data would be extracted from case series and not from higher-quality study types.
Study SelectionThe selection was made in an initial stage through the reading of abstracts by the authors. Studies that did not meet the eligibility criteria were excluded. Full text copies in English or Spanish were obtained for all the studies and evaluated by the authors. With the results of the initial search, other references of the selected studies were identified to expand the number of eligible studies, leading to a second search. Two authors carried out searches independently, which were later compared. In the articles in which there was controversy regarding their inclusion, the decision was made as a consensus.
Evaluation of the Methodological QualityThe methodological quality of all included studies was assessed by the authors and classified according to Oxford CEBM 200910 scientific level of evidence definitions. The following rules were applied, accepting that distinguishing between study designs can be problematic when it comes to observational studies.11
Surgical TechniqueWe focused on identifying studies of patients with Crohn's disease and perianal fistula who underwent surgery with the endorectal advancement flap technique. In order not to lose relevant information, we also included studies of patients operated on with this surgical technique in combination with some other type of variation in the technical procedure or added medical therapy related to their perianal disease.
The flap or endorectal advancement flap technique involves closing the internal orifice and covering it with an endorectal mucosal/submucosal flap of the rectal/anal wall, affixed with sutures. In addition to the thickness used (mucosal flap or mucosal-muscle flap), there are several technical variations that may include different suture types (absorbable vs non-absorbable) as well as the possible completion of a fistulectomy of the tract from the external orifice to the sphincter complex.12,13
Statistical AnalysisThe variables registered were described with appropriate descriptive statistics (absolute numbers or percentages, mean or medians, ranges or standard deviation). The synthesis of quantitative data was analyzed by results, using Excel for Windows® and SPSS® program 21.0.
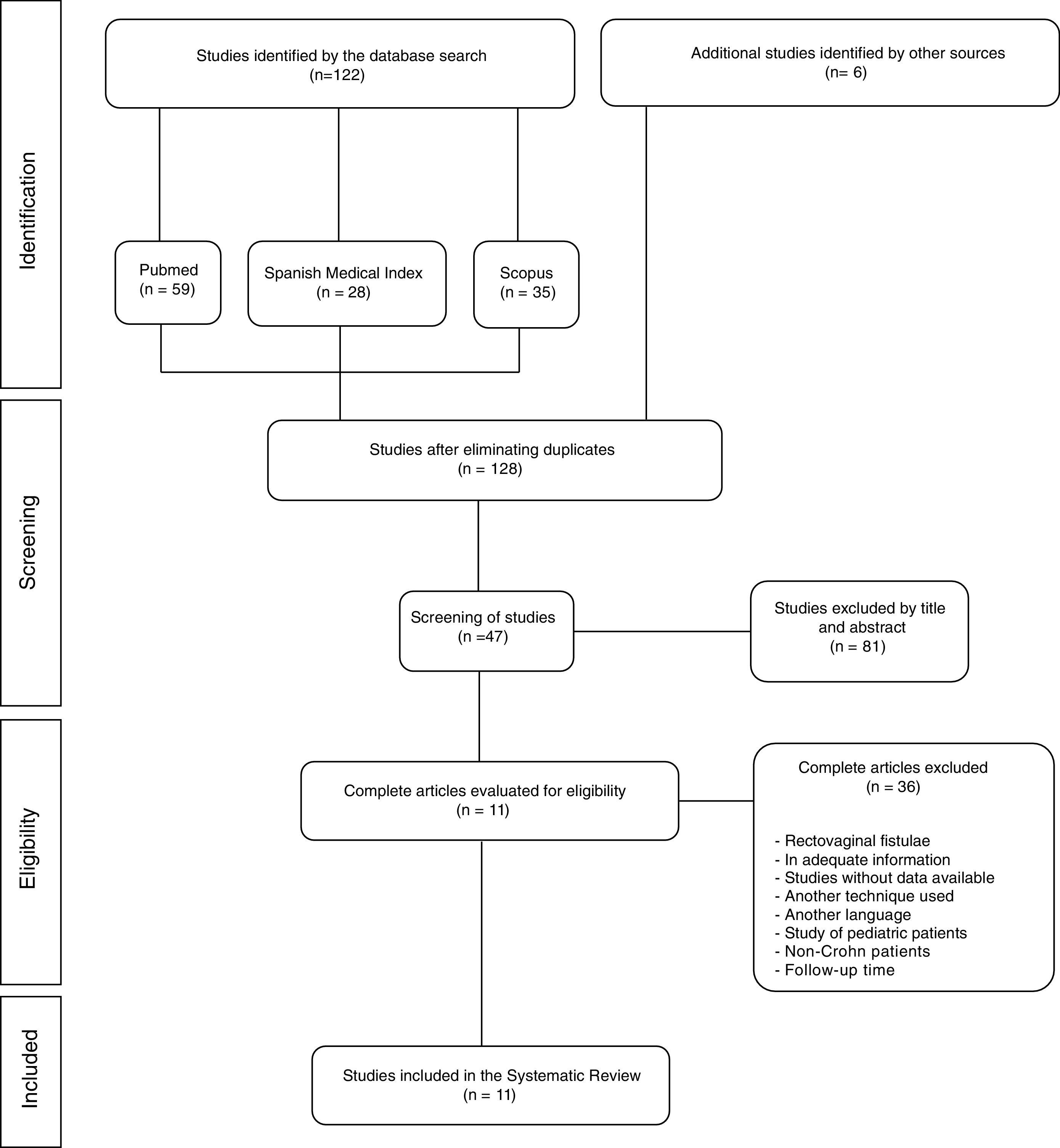
ResultsSelected StudiesThe initial search identified 122 potentially relevant studies (59 in PubMed, 28 in the Spanish Medical Index and 35 in Scopus). Six articles were excluded because they were duplicates, but 6 additional articles were identified by cross-references. Out of the 128 that were eligible, 81 were excluded because the title and abstract did not meet the established inclusion criteria.
Out of the 47 remaining articles selected for the review and for which full texts were obtained, another 36 were excluded because many reported rectovaginal fistula data (n=12), did not present clinical information of interest for the review (n=10) or simply did not show data in order to perform the analysis designed (n=6). Other articles were also excluded in this phase because they treated pediatric patients (n=1), patients without Crohn's disease (n=1) and one due to a short follow-up period of only 3 months. Finally, articles written in a language other than Spanish or English were discarded (n=2) along with studies that referred to another surgical technique (n=3). Therefore, a total of 11 studies were included in the final selection, as shown in the flow chart of Fig. 1.
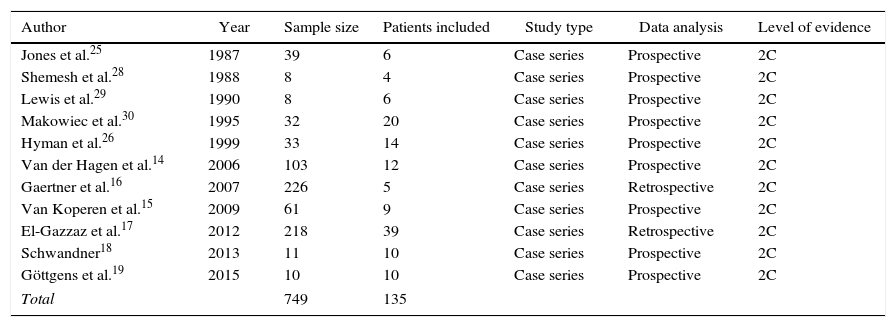
Characteristics of the StudiesThe detailed characteristics of the studies included in the review are shown in Table 1. Eleven studies were selected that were published between 1987 and 2015, which reported clinical data of a total of 749 patients. Five of these studies were from the United States, 3 from the Netherlands and the remainder from Italy, Germany and the United Kingdom (Fig. 2).
Characteristics of the Studies Included in the Systematic Review.
| Author | Year | Sample size | Patients included | Study type | Data analysis | Level of evidence |
|---|---|---|---|---|---|---|
| Jones et al.25 | 1987 | 39 | 6 | Case series | Prospective | 2C |
| Shemesh et al.28 | 1988 | 8 | 4 | Case series | Prospective | 2C |
| Lewis et al.29 | 1990 | 8 | 6 | Case series | Prospective | 2C |
| Makowiec et al.30 | 1995 | 32 | 20 | Case series | Prospective | 2C |
| Hyman et al.26 | 1999 | 33 | 14 | Case series | Prospective | 2C |
| Van der Hagen et al.14 | 2006 | 103 | 12 | Case series | Prospective | 2C |
| Gaertner et al.16 | 2007 | 226 | 5 | Case series | Retrospective | 2C |
| Van Koperen et al.15 | 2009 | 61 | 9 | Case series | Prospective | 2C |
| El-Gazzaz et al.17 | 2012 | 218 | 39 | Case series | Retrospective | 2C |
| Schwandner18 | 2013 | 11 | 10 | Case series | Prospective | 2C |
| Göttgens et al.19 | 2015 | 10 | 10 | Case series | Prospective | 2C |
| Total | 749 | 135 | ||||
Out of the 749 patients described, 135 patients met the inclusion criteria and the rest were excluded as they were patients with fistulae of cryptoglandular origin or non-anal fistulae (rectovaginal, rectourethral).
All the studies were case series. The majority had prospective data collection, except for 2 that were retrospective with a 2C level of scientific evidence, as shown in Table 1.
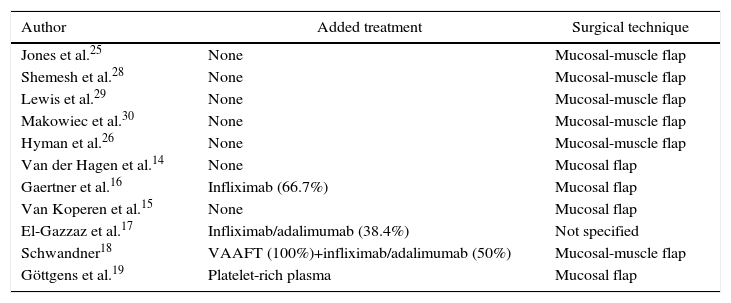
Surgical TechniqueThe studies by Van der Hagen et al.14 and Van Koperen et al.15 evaluated the use of endorectal advancement flaps as a surgical treatment for perianal fistulae involving the upper 2/3 of the anal sphincter and fistulotomy for the lower third, so we collected the data pertaining to the variables of interest.
Two studies (Gaertner et al.16 and El-Gazzaz et al.17) evaluated patients treated with biological therapy (anti-TNF), in addition to the surgical option, and compared them with patients treated with surgery alone. Among the surgical interventions performed were treatments with seton drainage, fistulotomy, fibrin glue, collagen plug, perineal repair and advancement flap. Both studies were retrospective.
The study by Schwandner et al.18 made the diagnosis with the help of video-assisted anal fistula treatment (VAAFT) prior to the completion of the advancement flap and, in some of their patients, biological therapy. Göttgens et al.19 combined the advancement flap treatment with instillation of platelet-rich plasma through the fistulous tract.
As there was some variation in the technical aspects, Table 2 specifies what the technique involved or the treatment added to the surgery and its correlation with the clinical results obtained.
Details of the Surgical Technique and the Treatment in Each Series Published.
| Author | Added treatment | Surgical technique |
|---|---|---|
| Jones et al.25 | None | Mucosal-muscle flap |
| Shemesh et al.28 | None | Mucosal-muscle flap |
| Lewis et al.29 | None | Mucosal-muscle flap |
| Makowiec et al.30 | None | Mucosal-muscle flap |
| Hyman et al.26 | None | Mucosal-muscle flap |
| Van der Hagen et al.14 | None | Mucosal flap |
| Gaertner et al.16 | Infliximab (66.7%) | Mucosal flap |
| Van Koperen et al.15 | None | Mucosal flap |
| El-Gazzaz et al.17 | Infliximab/adalimumab (38.4%) | Not specified |
| Schwandner18 | VAAFT (100%)+infliximab/adalimumab (50%) | Mucosal-muscle flap |
| Göttgens et al.19 | Platelet-rich plasma | Mucosal flap |
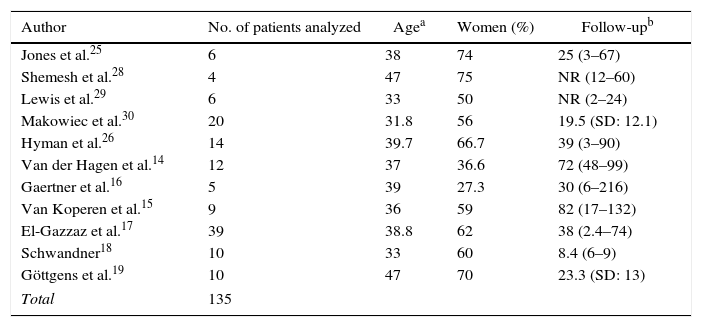
The studies reported limited patient series, with a minimum of 4 and a maximum of 39 patients. Only in 3 studies was the follow-up performed with MRI.14,17,19Table 3 shows the characteristics of age, gender and time of follow-up for each study. Due to the prevalence of Crohn's disease, most of the series were of young patients with an average age ranging between 33 and 47 years. The proportion of women in each study was very variable (from 27.3% to 75%).
Characteristics of the Patients of Each Study Included in the Systematic Review.
| Author | No. of patients analyzed | Agea | Women (%) | Follow-upb |
|---|---|---|---|---|
| Jones et al.25 | 6 | 38 | 74 | 25 (3–67) |
| Shemesh et al.28 | 4 | 47 | 75 | NR (12–60) |
| Lewis et al.29 | 6 | 33 | 50 | NR (2–24) |
| Makowiec et al.30 | 20 | 31.8 | 56 | 19.5 (SD: 12.1) |
| Hyman et al.26 | 14 | 39.7 | 66.7 | 39 (3–90) |
| Van der Hagen et al.14 | 12 | 37 | 36.6 | 72 (48–99) |
| Gaertner et al.16 | 5 | 39 | 27.3 | 30 (6–216) |
| Van Koperen et al.15 | 9 | 36 | 59 | 82 (17–132) |
| El-Gazzaz et al.17 | 39 | 38.8 | 62 | 38 (2.4–74) |
| Schwandner18 | 10 | 33 | 60 | 8.4 (6–9) |
| Göttgens et al.19 | 10 | 47 | 70 | 23.3 (SD: 13) |
| Total | 135 | |||
NR, data not reported.
The follow-up after surgery was also very heterogeneous and ranged from 8.4 to 82 months post-op. Two of the studies included did not report mean follow-up time but instead used time ranges.
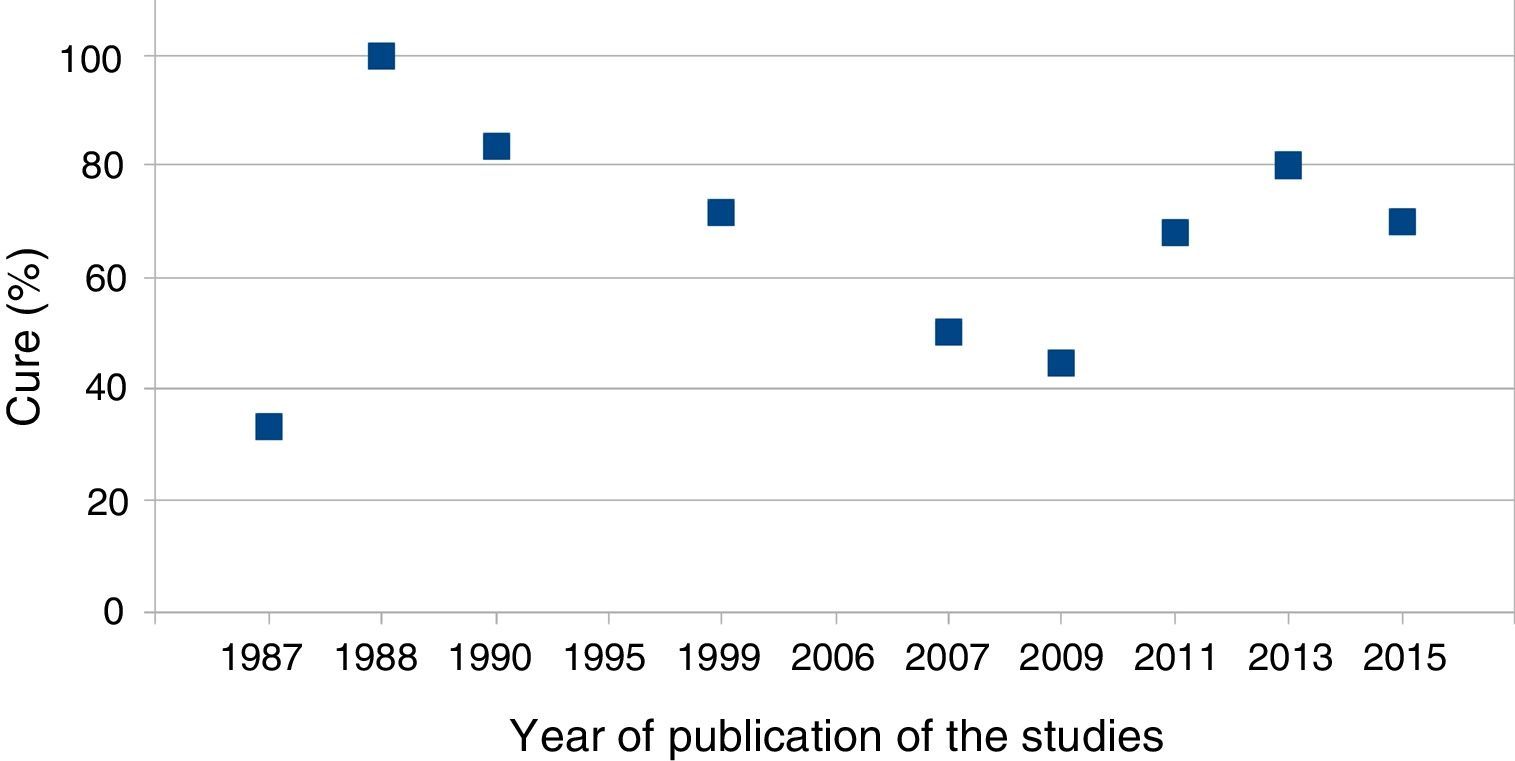
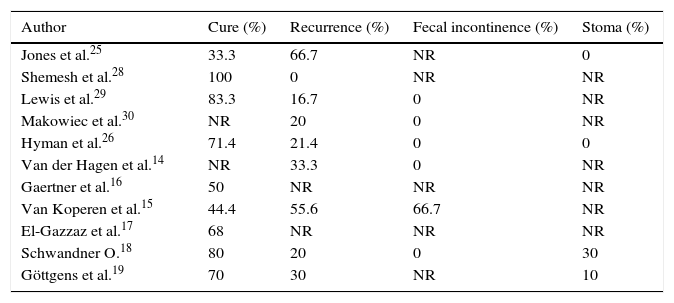
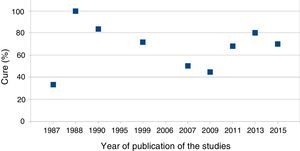
ResultsTable 4 describes the clinical results of the surgery. The cure percentages varied from 33.3% to 100% with a global average of 66.7%. In 2 of the studies, it was not possible to isolate the data of the patients of interest with regards to the cure rate. The postoperative anal fistula recurrence rates ranged from 0% to 66.7%, with a global mean recurrence of 30%.
Clinical Results in all the Patients Included in the Systematic Review.
| Author | Cure (%) | Recurrence (%) | Fecal incontinence (%) | Stoma (%) |
|---|---|---|---|---|
| Jones et al.25 | 33.3 | 66.7 | NR | 0 |
| Shemesh et al.28 | 100 | 0 | NR | NR |
| Lewis et al.29 | 83.3 | 16.7 | 0 | NR |
| Makowiec et al.30 | NR | 20 | 0 | NR |
| Hyman et al.26 | 71.4 | 21.4 | 0 | 0 |
| Van der Hagen et al.14 | NR | 33.3 | 0 | NR |
| Gaertner et al.16 | 50 | NR | NR | NR |
| Van Koperen et al.15 | 44.4 | 55.6 | 66.7 | NR |
| El-Gazzaz et al.17 | 68 | NR | NR | NR |
| Schwandner O.18 | 80 | 20 | 0 | 30 |
| Göttgens et al.19 | 70 | 30 | NR | 10 |
NR, data not reported.
Not all studies reported data on fecal continence or the need for a stoma during follow-up. The study by Van Koperen et al.15 reported 66.7% fecal incontinence and is the study with the longest mean clinical follow-up. Five of the studies analyzed reported 0% postoperative fecal incontinence. In the 4 studies that described the creation of a stoma in patients with poor clinical evolution, this situation was necessary in 0%, 10% and 30% of cases.
DiscussionSystematic reviews of the literature provide relevant clinical information, especially in those aspects of surgery in which it is very difficult to adequately conduct studies with a large number of patients. The surgical management of anal fistula in patients with Crohn's disease is an example. This was the reason for designing this systematic review of the literature, including the articles published during the last 30 years in Spanish and English about the clinical results of the advancement flap surgical technique in these patients. The result allowed us to select 11 articles and conclude that the results for cure are around 65%.
To our knowledge, this is the first systematic review of the literature that analyzes this therapeutic alternative only in patients with Crohn's disease and, although the strict selection criteria have allowed us to obtain valuable information, the study has certain limitations. The clinical series obtained are very heterogeneous (in number of patients and technique variations), with studies that provide a low level of scientific evidence. We therefore could not use meta-analysis techniques because the data were not very solid. Thus, the conclusions and the information analyzed have limited value in certain aspects. However, this review allows us to affirm, without forgetting its limitations, that this surgical technique should be considered an alternative in patients with Crohn's disease.
Interestingly, the published articles provide different technical aspects in addition to the advancement flap, such as the adjuvant use of treatments or associated maneuvers (for example, VAAFT18). However, there is little consensus as to the need or not of mechanical preparation of the colon or the use of antibiotics. Although these maneuvers are less controversial in cryptoglandular fistulae,2 in the context of Crohn's disease, which is still medically controlled, it is a different situation.
The analysis of complications after surgery for anal fistula of cryptoglandular origin, especially the appearance of postoperative fecal incontinence, has been fundamental in recent years.20,21 For this reason, we were interested in adding this secondary objective, especially in patients with Crohn's disease, since although the disease is controlled with medical treatment, the history of previous surgeries can cause altered bowel rhythm in the form of diarrhea and, therefore, a theoretical higher risk of incontinence.22 However, this datum was present in only 3 series and with very different data.
As a result indicator, we wanted to analyze (similar to other series) the need for creating a stoma in the evolution of complex anal fistulae, especially in patients with Crohn's disease. However, this datum acquires a different relevance in the clinical scenario of revision due to the presence of the disease.23,24 This datum was collected in 4 series: in 2 the stoma was not necessary in any case,25,26 while in the others it was necessary in 10%19 and in 30%,18 respectively.
During the completion of this review study, we found that there is little adequate literature on the treatment of perianal fistula using the advancement flap technique in patients with Crohn's disease, and the studies provide a low level of evidence (2C). For this reason, multicenter prospective and randomized studies should be designed to compare endorectal advancement flap with the other surgical techniques described (for example, LIFT27). In a study of these characteristics, it would be necessary to establish whether patients require medical treatment associated with their Crohn's disease due to the evidence of their effectiveness in the results.5
In conclusion, the results data of the treatment of complex anorectal fistulae in patients with Crohn's disease with endorectal advancement flap present a low level of evidence. In spite of this, the technique is recognized as a good alternative for the surgical management of anal fistula. It is therefore worth mentioning the need for specialized units to develop multicenter clinical trials that provide high-level evidence on the treatment of complex fistula in patients with Crohn's disease.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Rozalén V, Parés D, Sanchez E, Troya J, Vela S, Pacha MÁ, et al. Resultados del tratamiento quirúrgico de la fístula anal en pacientes con enfermedad de Crohn mediante técnica de colgajo de avance endorrectal: revisión sistemática de la literatura. Cir Esp. 2017;95:558–565.