Non-melanoma skin cancer includes basal cell carcinoma and squamous cell carcinoma (SCC). Basal cell carcinoma is the most common and least aggressive but in a low percentage of cases, despite appropriate wide surgical margins, it can be aggressive, producing local invasion, recurrences and distance metastasis. SCC has a more aggressive behaviour invading first the skin, the lymph nodes and less frequently produces distance metastasis.
ObjectiveTo identify the characteristics of recurrent SCC and frequency of new SCC after conventional surgical and primary closure or closure delayed until a histological reporting of tumour-free surgical margins, in order to achieve a better surgical option, in our Mexican population.
Materials and methodWe reviewed clinical records from the last 10 years, and included those with a diagnosis of SCC.
ResultsOne hundred and fourteen tumours in 103 patients were included. The mean new tumour diagnosis was 32.2 per year; there were 46.6% men and 53.4% women. Age range 19–91, with mean 71.94 years (SD=13.34). The evolution time was from 1 to 112 months (mean=12 months, SD=2.65). The most affected site was the cheek. In addition, an invasive tumour was reported in 54% in the histopathological study. At 10-year follow-up we found a second SCC in 14 patients and only 4 recurrences, between the 1st and 4th year and 3 were treated with delayed closure until margins were tumour-free.
ConclusionIn this study we demonstrated that delayed closure technique is easy and adaptable in our population in the treatment of SCC, achieving good results with very low recurrences at 10-year follow-up.
El carcinoma de piel no melanoma basocelular y el carcinoma epidermoide o espinocelular (CEC) son tumores frecuentes. El carcinoma basocelular es el cáncer más frecuente y el menos agresivo; en algunas ocasiones, a pesar del tratamiento quirúrgico con márgenes amplios, un porcentaje bajo tiene comportamiento agresivo, como invasión local extensa, recurrencias y metástasis. El CEC tiene un comportamiento más agresivo, primero en piel, después en ganglios linfáticos y, raramente, con metástasis a otros órganos.
ObjetivoIdentificar las características de los CEC recurrentes y la frecuencia de aparición de nuevos tumores, tras el tratamiento quirúrgico con cirugía convencional y cierre diferido de herida hasta obtener el resultado histológico libre de tumor (transoperatorio tardío), esto con la finalidad de tener mejores opciones de tratamiento en la población mexicana.
Material y métodoSe revisaron los expedientes de 10 años y se incluyeron aquellos que tenían diagnóstico de CEC.
ResultadosSe incluyeron 114 tumores en 103 pacientes. Utilizando un análisis descriptivo, se encontró que la media de diagnóstico de casos nuevos por año fue 32,2. Pacientes masculinos 48 (46,6%) y 55 (53,4%) femeninos. La edad diagnóstica fue entre 19 y 91 años (media=71,94; DE=13,34) con un tiempo de evolución de 1 a 112 meses (media=12 meses; DE=2,65). El más frecuente es en la mejilla y la variedad histológica invasiva se da en el 54%. En 14 pacientes se encontró un segundo CEC. Solo tuvimos 4 recurrencias, que aparecieron entre el primer y el cuarto año de seguimiento, y 3de estos fueron tratados con cirugía con transoperatorio tardío.
ConclusiónEste estudio demostró que la técnica de cirugía con transoperatorio tardío es adaptable para el tratamiento de CEC con buenos resultados y bajo porcentaje de recurrencia en un seguimiento a 10 años.
Non-melanoma skin cancer includes basal cell carcinoma and squamous cell carcinoma. Basal cell carcinoma (BCC) is the most common skin cancer; it is the least aggressive and generally has a good prognosis. A very low percentage of BCC behave aggressively with extensive local invasion, recurrences and metastases, despite extensive surgical treatment. However, squamous cell carcinoma (SCC) behaves more aggressively.
In general, a very small proportion of non melanoma skin cancers can behave aggressively, with extensive local invasion, multiple recurrences and occasionally, metastases, even after extensive surgery,1 and they have major functional, physical and social impact on the patient.2
Statistics on white populations show an increase in incidence of 10% per year,3 predominating in males, at a ratio of 1.3–1.9:1. Predominance in females between the sixth and eighth decades of life has been observed in Mexico. When it presents in children, it is generally associated with a genodermatosis such as xeroderma pigmentosum, with a recurrence risk of up to 18%.4–6 However, it should be stressed that the age of presentation is changing and there is currently a greater incidence in young people,5 especially females and smokers.7
The largest series of squamous cell carcinoma, conducted in Mexico, describes this tumour as more common in women, with an average age of 71, and predominating in the face. In this study the average size of the lesion was 3cm and most had ulceration.6
There can be many treatment methods for squamous cell carcinoma; however, surgery is the treatment of choice. For low-grade tumours a surgical safety margin of between 4mm and 6mm is recommended and primary closure or reconstruction with flap or graft. The surgical specimen is sent to the pathology department and if positive in the margins or bed, the patient should be reoperated using a conventional procedure, micrographic Mohs micrographic surgery (MMS), or receive radiotherapy. For high-grade tumours, MMS is the standard of care or, if this technique is not available, resection with a margin of 1cm. Tumours that are not candidates for surgery are sent directly for radiotherapy.9
Because MMS was not available in our environment due to its high cost, when this technique was required, we excised the tumours with the margins indicated according to whether the grade was high or low. If primary closure was not feasible, the surgical defect was left open until the margins had been confirmed by histopathology: which we termed delayed closure. We used this technique because occasionally a flap would be required to close the surgical defect and re-excision would be more difficult if positive surgical margins had been found.
ObjectiveTo identify the characteristics of squamous cell carcinoma, its recurrence and the frequency of onset of new tumours, in our cases, and to identify those treated surgically with direct closure or closure delayed until receiving a tumour-free margin report (delayed closure), and thus determines optimal treatment behaviours.
Material and methodThe clinical records of patients diagnosed with squamous cell carcinoma who attended the dermatological surgery department of the Hospital General Dr. Manuel Gea González in a period of 10 days. The following variables were obtained from these patients: sex, age, time of onset, topography, morphology, histological characteristics, time between primary excision and recurrence, type of surgical treatment and follow-up time. We used descriptive statistics.
ResultsOne hundred and fourteen tumours were studied, from 103 patients with a diagnosis of squamous cell carcinoma. Of the total number of patients, 48 (46.6%) were male and 55 (53.4%) female. The age of diagnosis was between 19 and 91 years (mean=71.94; SD=13.34) with an onset time from 1 to 112 months (mean=12 months; SD=2.65).
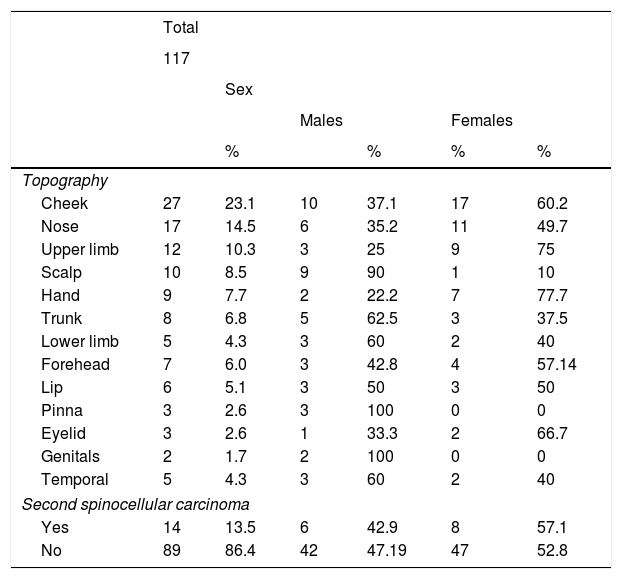
The most common site was the cheek (Fig. 1), with a histological variety of invasive SCC (54%), followed by SCC in situ. Table 1 shows the demographic characteristics of the case series (Fig. 1).
General characteristics of squamous cell carcinoma in the sample studied.
| Total | ||||||
|---|---|---|---|---|---|---|
| 117 | ||||||
| Sex | ||||||
| Males | Females | |||||
| % | % | % | % | |||
| Topography | ||||||
| Cheek | 27 | 23.1 | 10 | 37.1 | 17 | 60.2 |
| Nose | 17 | 14.5 | 6 | 35.2 | 11 | 49.7 |
| Upper limb | 12 | 10.3 | 3 | 25 | 9 | 75 |
| Scalp | 10 | 8.5 | 9 | 90 | 1 | 10 |
| Hand | 9 | 7.7 | 2 | 22.2 | 7 | 77.7 |
| Trunk | 8 | 6.8 | 5 | 62.5 | 3 | 37.5 |
| Lower limb | 5 | 4.3 | 3 | 60 | 2 | 40 |
| Forehead | 7 | 6.0 | 3 | 42.8 | 4 | 57.14 |
| Lip | 6 | 5.1 | 3 | 50 | 3 | 50 |
| Pinna | 3 | 2.6 | 3 | 100 | 0 | 0 |
| Eyelid | 3 | 2.6 | 1 | 33.3 | 2 | 66.7 |
| Genitals | 2 | 1.7 | 2 | 100 | 0 | 0 |
| Temporal | 5 | 4.3 | 3 | 60 | 2 | 40 |
| Second spinocellular carcinoma | ||||||
| Yes | 14 | 13.5 | 6 | 42.9 | 8 | 57.1 |
| No | 89 | 86.4 | 42 | 47.19 | 47 | 52.8 |
Due to their topography, differentiation, invasion and size, 50% of the tumours in the series were included in the high-risk category.
Of the 103 patients with SCC, 14 had a second primary tumour (maximum 3). Of these, 6 (42.9%) were male and 8 (57.1%) female. There were no significant differences in the likelihood of developing a second SCC between the males and the females.
Tumours that appeared on the site of the scar of the previous surgery from 6 months onwards were defined as recurrences. There were only 4 recurrences (2.2%) that appeared between 1 and 4 years (mean 2.12 years; SD=1.31 years) after the primary tumour. With regard to topography, size and histology, no statistically significant differences were found in the recurrence rate. Of the 4 recurring tumours, 3 were treated with delayed closure, which showed no statistically significant association, since there were too few cases to show a tendency.
Of the 114 tumours, 30 (32.5%) were reconstructed with delayed closure until the margins were confirmed tumour-free and 79 (67.5%) had primary closure; we could not find the data in the clinical records of 5 cases.
The average margin in the tumours studied was 7.2mm, with a minimum of 3mm and a maximum of 5cm (SD=0.473). Tumours in situ had the smallest margins and infiltrating tumours had the largest.
DiscussionMost cutaneous squamous cell carcinomas are benign and can be cured with conventional surgery. However, high-risk squamous cell carcinoma has been identified that can metastasise in up to 5% and present local recurrence from 3% to 8%. High-risk spinocellular tumours measure more than 2cm, present on the face, are histologically invasive if thicker than 2mm with a Clark level greater than iv, involve perineural invasion and are poorly differentiated.7 Moreover, these tumours have greater recurrence rates after surgical removal.
In situ squamous cell carcinoma is limited to the epidermis and is the precursor to invasive squamous cell carcinoma, which must be treated aggressively and accurately to prevent its progression and worsen the patient's prognosis.8 Immunosuppression is a variable of poor prognosis in these types of tumours, since the condition and the use of immunosuppressant drugs increase the risk of squamous cell carcinoma by 65 times that of the normal population.8
There are many studies on the effectiveness of MMS and the low incidence of recurrence, some with insufficient evidence to compare effectiveness and the different treatments used for SCC. This prompted Dr Chren to analyse 2 university sites with a population of 1253 patients and 1585 tumours treated with different methods, including excision and MMS. She concluded that the recurrence rate of SCC with MMS was 2.1% and 3.5% after simple excision.10
It must be stressed that in our study, despite having tumours with high-risk factors for recurrence, a recurrence rate of 2.2% was found, similar to that of Mohs surgery, using delayed closure until confirmation of tumour-free margins (Figs. 1 and 2). This finding is important, since it offers us the opportunity to provide optimal treatment for cutaneous squamous cell carcinoma at lower cost and in areas that lack the infrastructure to perform the aforementioned surgical technique.
We must emphasise that one of the cases that recurred was an in situ squamous cell carcinoma, which was treated with the surgical margin indicated in the clinical guidelines. This leads us to the conclusion that it is likely that, rather than a recurrence, this was a new cancer in an area of field cancerisation with extensive photodamage. The other 3 tumours that recurred were invasive and of an aggressive histological type, which is a very important risk factor for recurrence and metastasis.
We must suspect recurrence if a skin lesion appears on the scar or an area nearby; it can present as an erythemato-squamous plaque or a tumour ranging from millimetres to centimetres in size.
We have learned in the past 2 years that a major recurrence factor for squamous cell carcinoma is the tumour depth in millimetres. Because this is a ten-year retrospective study, we do not have this data for all the tumours we studied, since in previous years this feature was not routinely assessed.11
ConclusionThis study demonstrated that the delayed closure technique is economical and can be adapted to other hospitals, and contributes towards the low recurrence rate of cutaneous squamous cell carcinoma lesions, with results that are comparable to those of MMS.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Domínguez-Cherit J, Rodríguez-Gutiérrez G, Narváez Rosales V, Toussaint Caire S, Fonte Avalos V. Características del carcinoma epidermoide cutáneo y riesgo para el desarrollo de recidivas con cirugía convencional y cirugía con transoperatorio tardío. Cir Cir. 2017;85:499–503.