Nasal vestibular stenosis is not only an esthetic, but also a functional problem for the patient.1 It is caused by disruption of the nasal vestibular lining with secondary proliferation of granulation and fibrous tissue.1,2 Various causes account for the development of nasal vestibular stenosis, including trauma, infection, and iatrogenic injury to the vestibular skin. Although a number of techniques have been described for repairing vestibular stenosis,2–4 correction may be difficult because of the tendency to wound contracture and recurrence. Herein, we describe a rare clinical presentation of nasal vestibular stenosis after maxillofacial surgery, which was successfully treated with endoscopic lysis of synechiae, release of vestibular scarring, and nasal stenting. This study was approved by the institutional review board of Pusan National University Hospital.
Case reportA 18 year-old man presented with epistaxis and multiple facial lacerations, following a falling on a sharp edge of a staircase at a drunken state. Facial computed tomography (CT) scans showed multiple fractures at the right infraorbital rim, right orbital floor, and both nasal bones with nasal septum. The patient underwent open reduction and internal fixation of infraorbital rim fracture through subciliary incision, correction of right blowout fracture, closed reduction of nasal bone fracture and primary closure of facial laceration in the plastic surgery department.
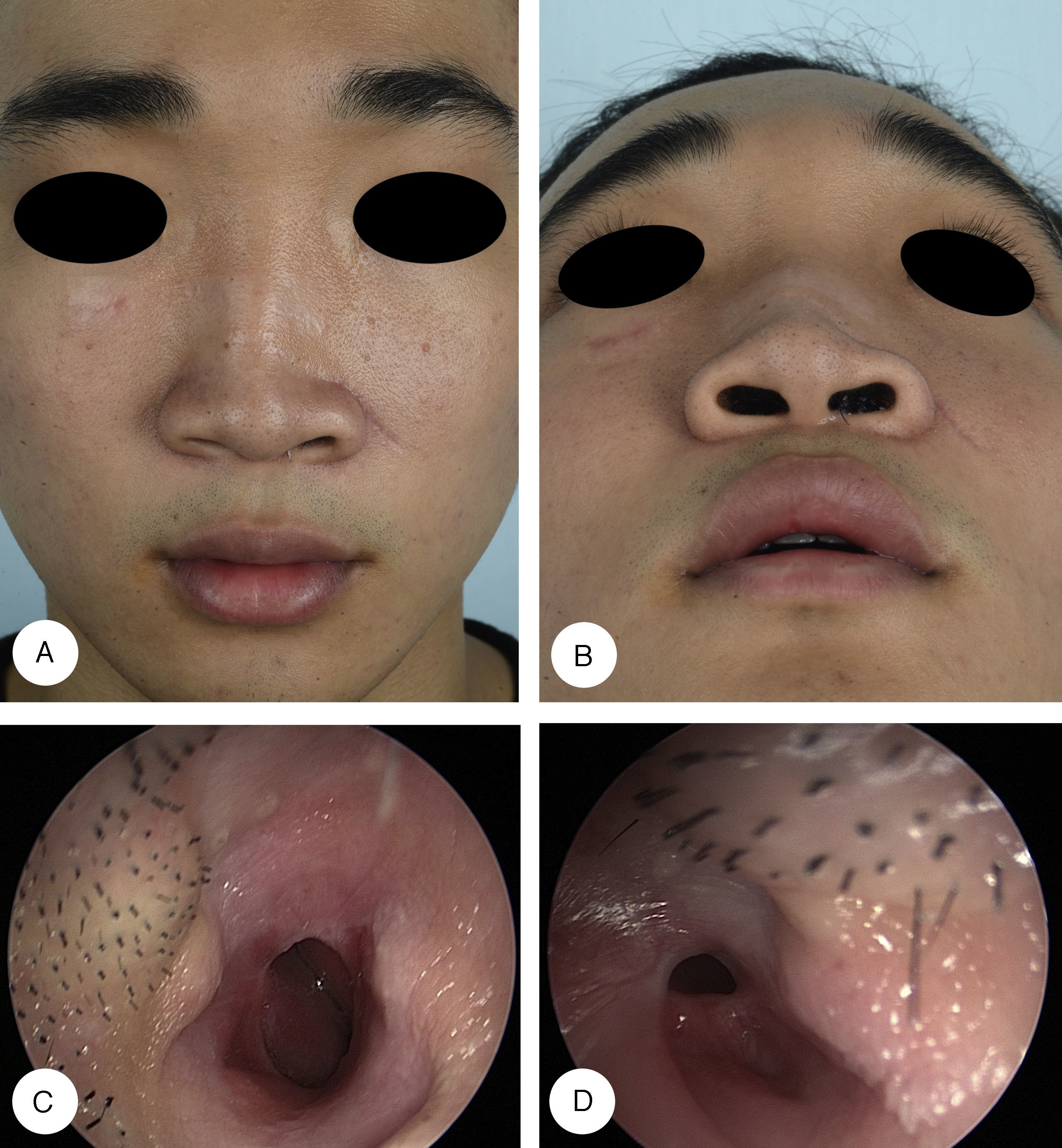
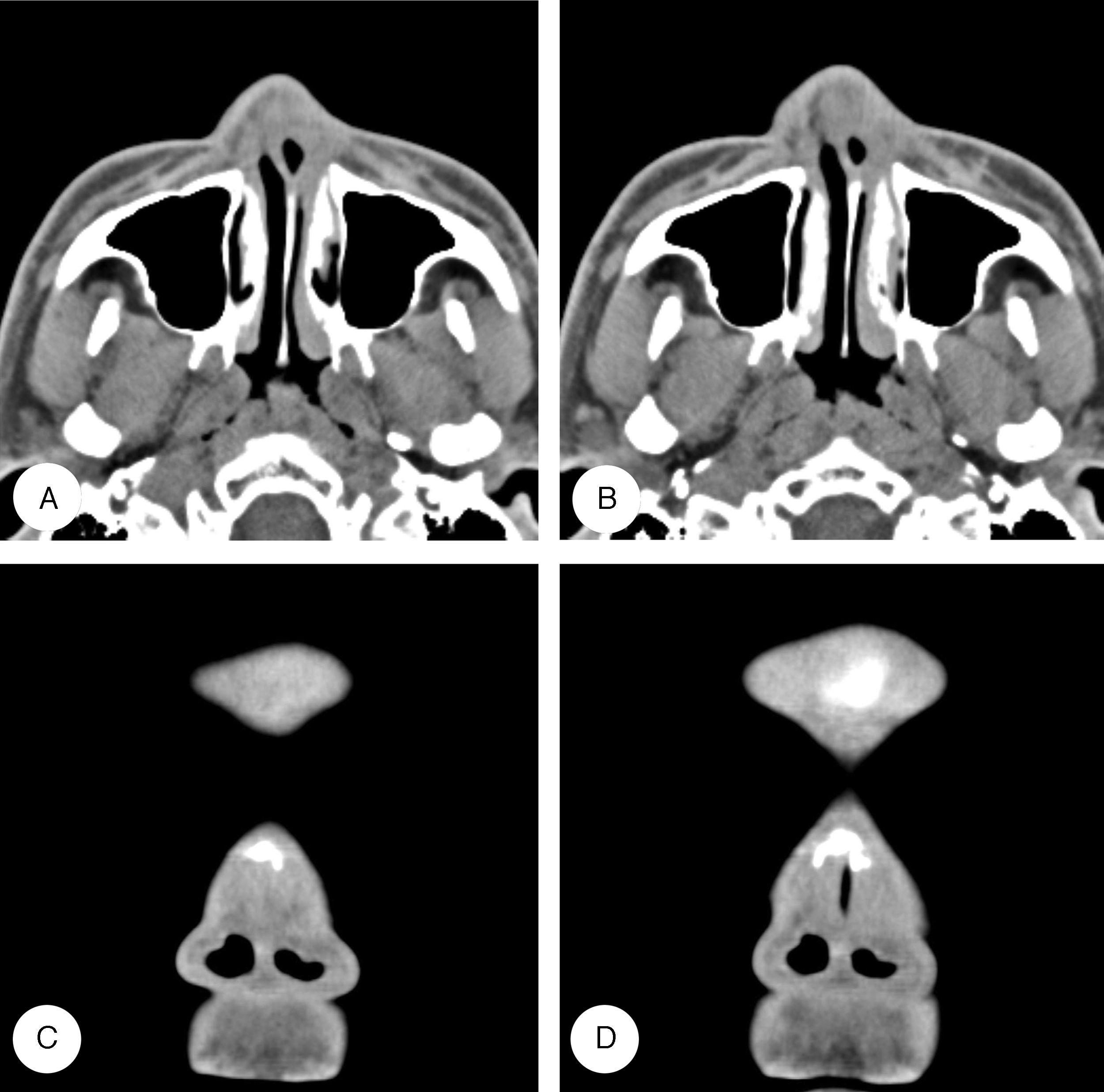
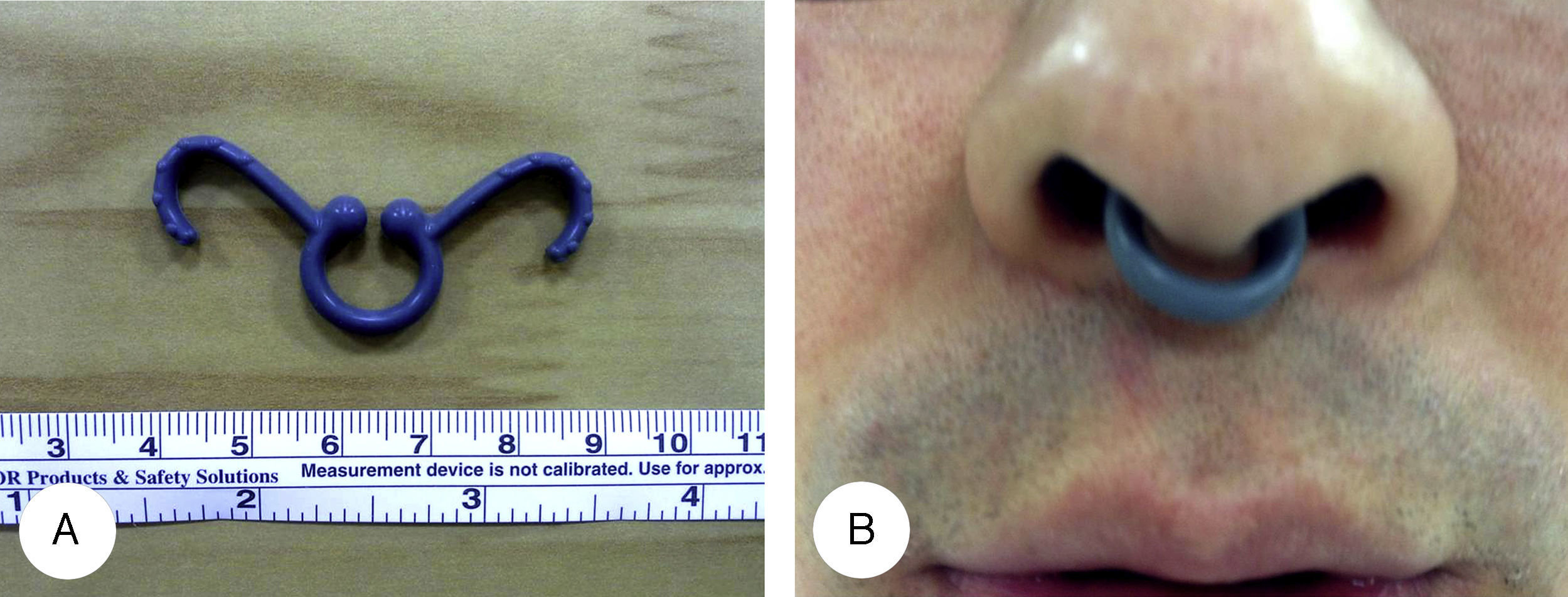
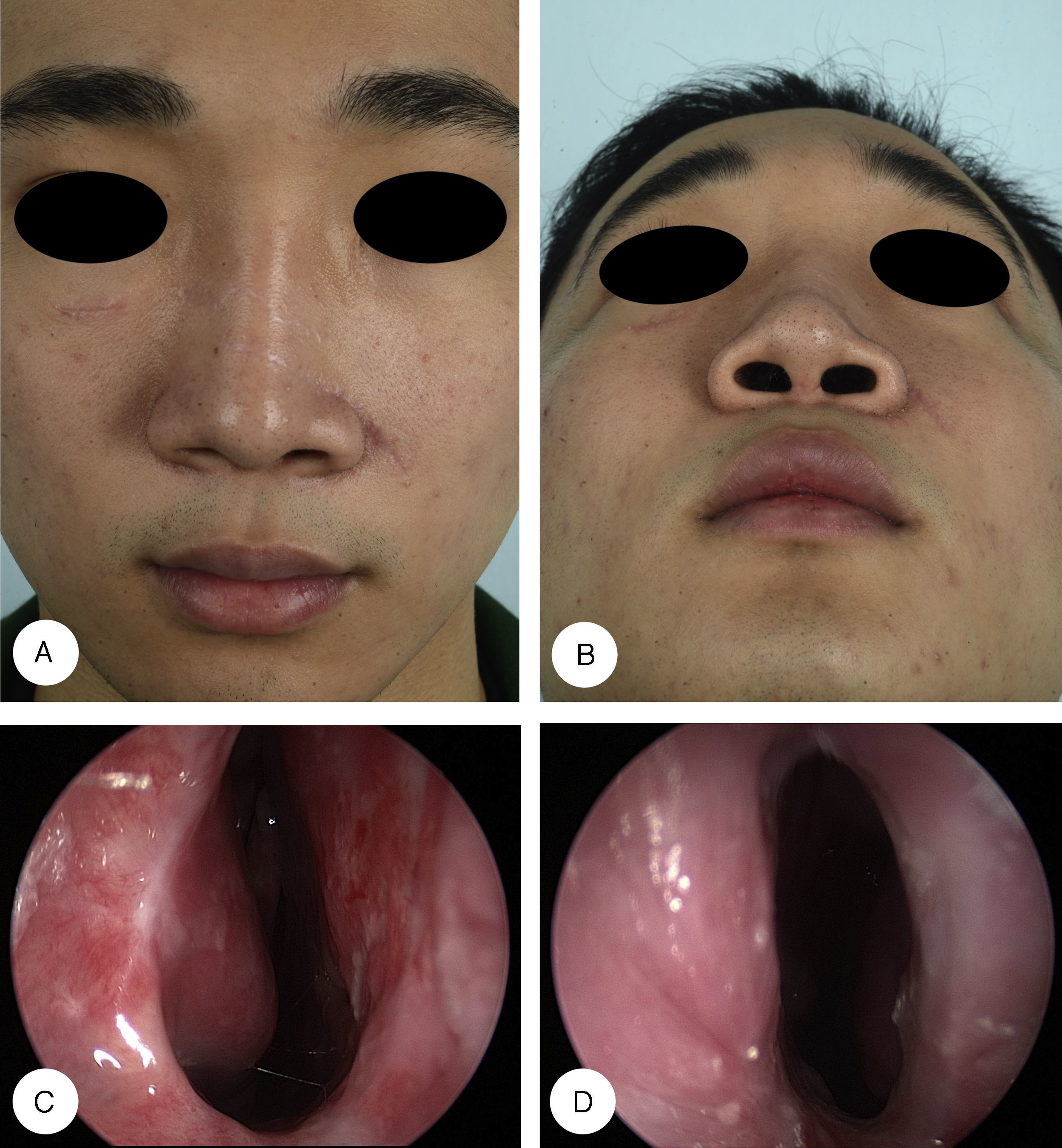
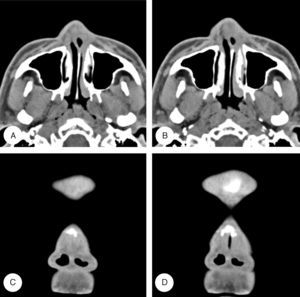
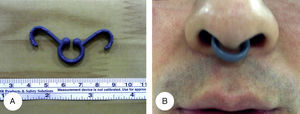
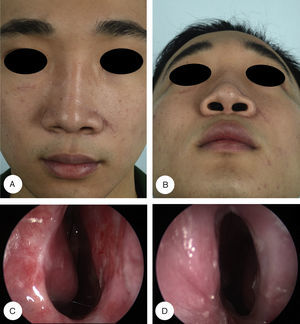
Three months later, he was referred to the otorhinolaryngology department because of a gradually progressive, bilateral nasal obstruction. Physical examination revealed adhesions within the nasal vestibule obscuring about 70% and 90% of the right and left nasal cavities, respectively, and causing a cosmetic deformity from collapse of the left nasal alar cartilage (Fig. 1). Preoperative CT scan confirmed the diagnosis of nasal vestibular stenosis and nasal septum deviation to left side (Fig. 2). The patient was taken up for surgical correction under general anesthesia. After lysis of the vestibular adhesions using a knife and microdebrider, the nasal ala returned to the normal anatomic position. An endoscopic examination revealed additional synechia between the anterior aspect of inferior turbinates and nasal septum on both sides. The intranasal synechia were lysed with endoscopic assistance, and septorhinoplasty was also performed. A silastic sheet was placed in both nasal cavities preventing apposition of the two raw surfaces as a stent, and secured to the nasal septum with a 4–0 silk suture. Furthermore, an additional wing-shaped stent was applied to create a tunnel between the lateral nasal wall and the nasal septum (Fig. 3). Three weeks later, the nasal stent and silastic sheet were removed. The patient remained asymptomatic during the six-month follow-up, with an excellent cosmetic outcome and without recurrence of synechia (Fig. 4).
Preoperative profiles and endoscopic findings. Frontal (A) and basal (B) views show linear scars in the nasal dorsum and collapse of the left nasal alar cartilage. Nasal endoscopy shows vestibular stenosis obscuring about 70% and 90% of the right (C) and left (D) nasal vestibule, respectively.
Nasal vestibular stenosis is an uncommon but debilitating cause of nasal obstruction.1 It may show all degrees of narrowing, from slight stenosis to complete atresia, and occur unilaterally or bilaterally.5 Nasal vestibular stenosis usually begins in the upper and lateral aspects of the nasal vestibule because of the lack of support of the alae compared with the more rigid septal and lower lateral cartilages. Although the inciting event in nasal vestibular stenosis is injury to the vestibular lining, partial or circumferential scarring within the vestibule contributes additional contractive forces that tend to obliterate the cephalic and lateral portions of the vestibule and distort the flaccid alar wing.2 In addition to tissue loss and scar contracture, the constant negative pressure generated by inspiratory forces on the nostril further adds to the tendency for the injured vestibule to contract.6 Our case showed that iatrogenic adhesions after maxillofacial reconstructive surgery typically involve the nasal vestibule and anterior aspect of the inferior turbinate.
The diagnosis of vestibular stenosis is clinical.1 Patients complain of constant unilateral or bilateral nasal obstruction. Physical examination confirms an area of stenosis in the vestibule. Associated nasal valve collapse may also be seen on some occasions. Furthermore, adhesions may extend throughout the nasal cavity. Therefore, following release of the nasal vestibular stenosis, endoscopic examinations of the entire nasal cavity should be performed to rule out intranasal synechia.4 A CT may be helpful to assess the thickness of atretic segment and any other associated abnormality of nasal cavity and sinuses.1 In our case, nasal septum deviation and additional synechia were identified between the anterior aspect of inferior turbinate and nasal septum on both sides.
Although various techniques have been described for the repair of nasal vestibular stenosis, treatment of this deformity can be difficult because of the tendency to wound contracture and frequent relapse. Previous surgical treatment modalities have focused on lysis of adhesions with skin grafting, mucosal grafting or local flap to cover the resultant tissue defect.2,3,5 However, these techniques may be difficult due to the small size of the nasal vestibule and the limited availability of donor tissue for rotation. Furthermore, additional intranasal incisions can lead to further scarring. Therefore, recent studies support management by endoscopic lysis, mitomycin application, and stenting by different tubing.4,7 Nasal stents may be used to keep raw surface apart, prevent contractions and closing of the nasal airway by granulations. In the present case, endoscopic lysis of adhesions with postoperative stenting was performed successfully, and the patient remained asymptomatic after more than six months of follow-up. Because a wing-shaped stent has the inherent spring effect, a gentle pressure was applied to the lateral nasal wall and septum, thus creating a tunnel in between. Moreover, the stent placement is technically simpler and it provides support to the external and internal nasal valves.
ConclusionAlthough iatrogenic nasal vestibular stenosis is a rare complication following maxillofacial reconstructive surgery, otolaryngologists must take great care to avoid this potential complication because it is a very difficult functional problem to treat. However, this can be successfully corrected with endoscopic lysis of synechiae and nasal stenting.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Yoon BW, Kim DW, Choi SJ, Cho KS. Iatrogenic nasal vestibular stenosis after maxillofacial reconstructive surgery. Braz J Otorhinolaryngol. 2018;84:126–30.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.