1. Summary of the clinical history (A-12-09)
We present the case of a male patient at 12 weeks of age at the time of his last admission to the emergency room.
1.1. Family hereditary history
The patient's mother is a healthy 20-year-old with a high school education. The father is 21 years of age, works as a mason, and reports tobacco consumption, alcohol and marijuana use.
1.2. Non-medical personal history
The family is originally from Huixquilucan, Mexico and represents a low-medium socioeconomic status. The patient was fed exclusively breast milk. His psychomotor development was normal. He had vaccines current for age (BCG, hepatitis B, pentavalent, rotavirus, pneumococcus).
1.4. Perinatal and medical history
During pregnancy the mother had a threatened abortion associated with cervicovaginitis for which she received treatment. The baby weighed 2650 g at birth with a length of 47 cm and Apgar score 8/9.
At 8 days of life the patient had a neonatal sepsis with a pneumonic focus (management is unknown). Left lung agenesis was diagnosed and the patient was referred to the Hospital Infantil de Mexico Federico Gómez. At 7 weeks of life, direct laryngoscopy was done and tracheal stenosis of 50% caliber was found. The right bronchus was of normal caliber and the left ended in a blind pouch. The following day the patient was brought to the emergency department because of fever, pallor and cough. He had difficulty breathing and systemic hypoperfusion. Mechanical ventilation was initiated via an endotracheal cannula with crystalloids and inotropic infusion. Mediastinitis was suspected because of the history of endoscopy and coverage with antibiotics was initiated with clindamycin, cefepime and amikacin. Echocardiogram did not identify cardiac malformations, but a pulmonary pressure of 48 mmHg was recorded for which sildenafil was begun at a dose of 1.5 mg/kg/day. This regime was continued as an outpatient upon discharge 1 week later.
The patient presented to the emergency department at 12 weeks of age due to respiratory difficulty, pallor and progressive hyporexia associated with irritability. On admission he was found to be unconscious, flaccid, without respiratory effort. There was no heart beat and the patient had a temperature of 32°C and weight of 3100 g. Resuscitation maneuvers were begun: 10 cycles of external chest compressions, six doses of adrenaline and two doses of sodium bicarbonate, one bolus of crystalloids and infusion of adrenaline. After 6 min of resuscitation he recovered cardiac rhythm and infusions of dobutamine and milrinone were added.
He was admitted on an emergency basis to intensive care therapy where a hemoglobin of 7.6 g/dl, 30,400 leucocytes/mm3, 652,000 platelets/mm3, clotting times above the maximum, elevation of liver enzymes and metabolic acidosis of 6.77 with 9.6 lactate were documented. The patient was managed with mechanical ventilation, cefotaxime, oseltamivir, platelet and plasma transfusions, and inotropic infusions and permissive hypothermia. Echocardiogram showed an ejection fraction of 48%. He remained with Glasgow coma scale of 4/15 with mydriatic pupils, areflexic, with absent vestibulo-cochlear and corneal reflexes. Electroencephalogram showed low voltage delta activity without reactivity and with severe dysfunction. The patient died 3 days after his admission.
2. Case presentation (Dr. Iván Rivas Rivera)
We are discussing the case of a male patient, 2 months of age, referred to a second-level hospital, who at 8 days of life presented a picture of neonatal sepsis with a pneumonic focus where the lack of a left lung was noted. Absence of the left lung can be diagnosed as pulmonary agenesis when there is absence of lung tissue and of bronchial structures, arteries and vein, or pulmonary aplasia where there is a rudimentary bronchial growth of a few centimeters in diameter, without pulmonary tissue, due to a change in the development during the fourth to fifth weeks of gestation. Both malformations occur more frequently on the left side.
Congenital airway abnormalities are rare diseases. The incidence of tracheal stenosis is∼1/60,000 births, representing 0.3 to 1% of all cases of laryngotracheal stenosis. Symptoms include biphasic stridor, cough, shortness of breath, cyanosis, and recurrent respiratory infections, which depends on the length, location and severity of the stenosis. Our patient had a great majority of these symptoms at some time during his life.
As part of this patient's workup, structural cardiac disorders were ruled out, which frequently accompany congenital airway malformations. Four days after his last admission, the patient presented because of abundant secretions, pallor and cyanosis. Although the discharge summary did not specify the physical examination at that time, based on the history and the events that subsequently occurred, it is possible that he then presented with a new picture of pulmonary infections because, as was mentioned previously, the anatomic variations of the airway predispose the patient for the appearance of infectious processes of the lungs.
During his last admission the patient was without vital signs, for which he required advanced resuscitation maneuvers. Unlike the adult population, the main cause of cardiac arrest in children is respiratory failure. Only 3.5% of pediatric patients admitted to an emergency room with a cardiac arrest survive to be discharged. Neurological prognosis is very poor because∼70% will suffer brain death.1
During the period after resuscitation the patient was described as having data of systemic inflammatory response based on the presence of leukocytes of 30,400 with neutrophilia, hypothermia of 32ºC with a probable pulmonary focus, as well as data of renal compromise with serum creatinine levels of 0.8 mg/dl and potassium 6.6 mEq/l.
Empiric treatment was initiated with cefotaxime and oseltamivir according to the treatment guidelines for pediatric patients with community-acquired pneumonias published in 2011 by the American Association of Infectious Diseases (AAID). They recommend empirical antimicrobial treatment in seriously ill patients with a third-generation cephalosporin plus oseltamivir if there is a high incidence of infection due to influenza virus.
Neuroprotective measures were initiated including permissive hypothermia. From 2006, pediatric resuscitation guidelines include hypothermia between 32°C and 34°C for 12 to 24 h for patients who continue in a state of coma after advanced resuscitation.2 There is still uncertainty about when and for how long permissive hypotherapy should be continued to achieve the best possible neurological prognosis. Therefore, since 2009 in various hospitals in the U.S. and Canada, a randomized study was conducted entitled "Therapeutic hypothermia to improve survival following cardiac arrest in pediatric patients," the results of which will be published in 2015.
Twenty hours after his admission, the patient presented brain death characterized by areflexive mydriatic pupils, negative vestibulo-cochlear and corneal reflexes as well as EEG without activity. He subsequently presented dysautonomia, multiple organ failure, bradycardia, desatura tion, absence of pulses and, finally, was pronounced dead 48 h after his admission.
In short, this is the case of a malnourished infant who had a diagnosis of two major airway malformations. He presented three episodes of lower respiratory tract infection, the latter of which led to cardiac arrest.
The final diagnoses are as follows:
* Infant with severe malnutrition
* Left lung aplasia
* Congenital tracheal stenosis
* Community-acquired pneumonia
* Septic shock secondary to pneumonic focus
* Multiple organ failure
* Cerebral death secondary to hypoxia
2.1. Imaging findings (Dr. Ana Gabriel Hernández)
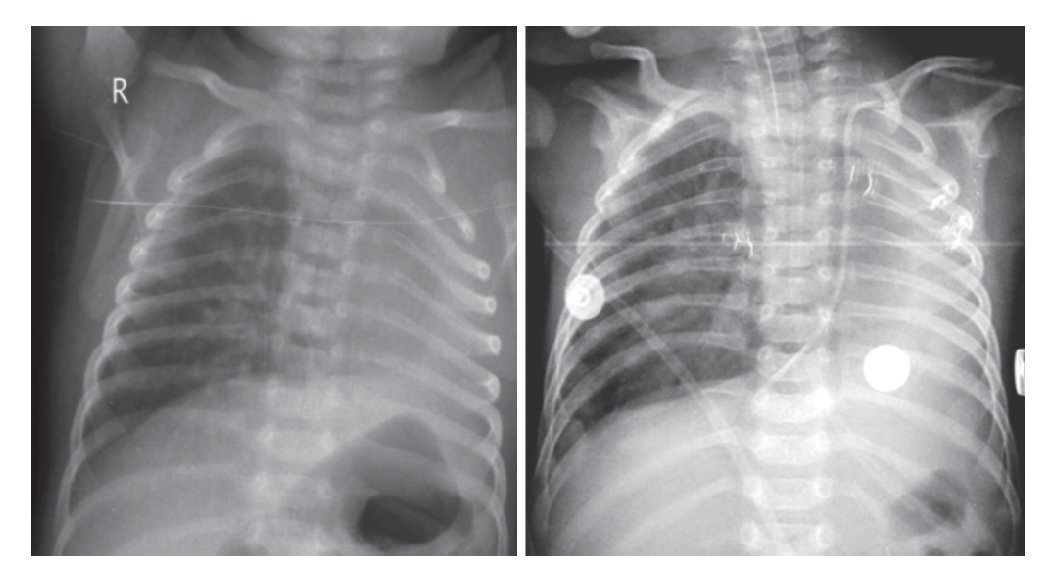
Plain films of the chest and abdomen show a radiopacity in the left hemithorax and overdistention of the right lung with herniation towards the left side. There was right parahilar reticular infiltrate, which evolved to nodular reticulum. A decrease in the intercostal spaces is appreciated with elevation of the diaphragm in the area of the opacity (Fig. 1).
Figure 1 Plain films of the chest and abdomen where radiopacity is seen in the left hemithorax and over distention of the right lung with herniation into the left side.
2.2. Bronchoscopy findings (Dr. Gustavo Teyssier Morales)
There was a decrease in the caliber of the trachea two rings below the subglottic region until just before the carina, which only allowed the passage of a 2.9 mm fiberoptic bronchoscope. The tracheal rings were complete and the left bronchus ended in a blind cul-de-sac; therefore, diagnosis of congenital tracheal stenosis and pulmonary aplasia was made.
2.3. Anatomic pathological findings (Dr. María de Lourdes Cabrera Muñoz)
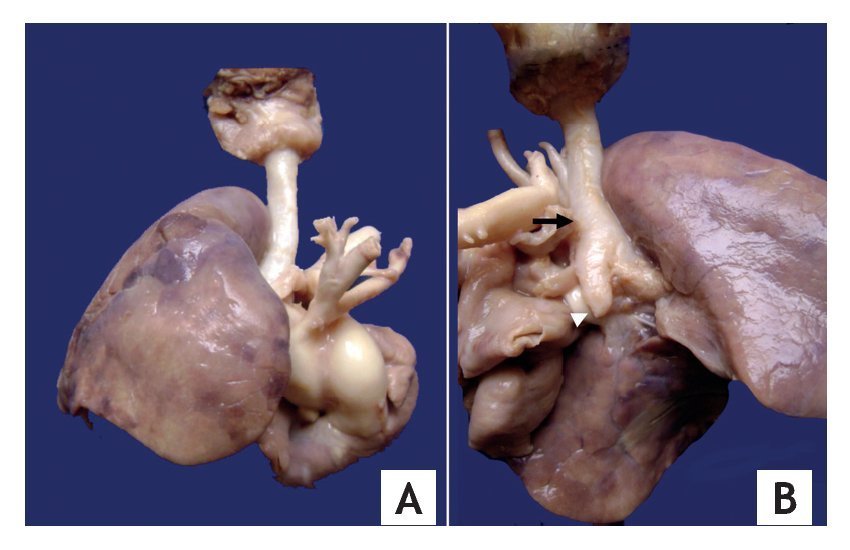
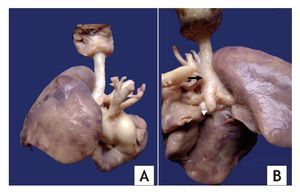
Pulmonary aplasia is a rare congenital malformation and may be associated with malformations of the airways and other organs, among which are tracheal and renal malformations. The autopsy showed a patient of apparent age equal to chronological age with right cryptorchidism and without external malformations. Upon opening the chest cavity, there was absence of the left lung. The right lung was increased in size and displaced the heart towards the left, and there was a small left pleural cavity. The trachea showed a permeable lumen and reduction of the diameter of the lumen below the glottis. Two main bronchi originated from the carina, the left one which ended in a cul de sac; the right was elongated and morphologically straight. The right lung showed two lobules (Fig. 2).
Figure 2 (A) Macrophotography showing bilobed right lung and decreased caliber of the trachea. (B) The trachea with absence of the membranous part on its posterior side (arrow). Note the absence of lung tissue and the left bronchus in cul-de-sac (arrowhead).
The terms aplasia, agenesis and pulmonary dysplasia are confusing and have been used in the medical literature in an inconsistent and interchangeable manner. However, the term aplasia is preferred when there is absence of pulmonary tissue and there exists a rudimentary main bronchus, and agenesis when there is absence of pulmonary tissue and of the main bronchus.3 In this case, the findings correspond to a left pulmonary aplasia with left lung pseudoisomerism. It has been reported that 70% of pulmonary aplasias are left-sided and with a prevalence in males. In up to 50% of the cases there are other associated malformations, which include tracheoesophageal fistulas, esophageal atresia, horseshoe kidney, cardiac mal formations and anal atresia, among others.4
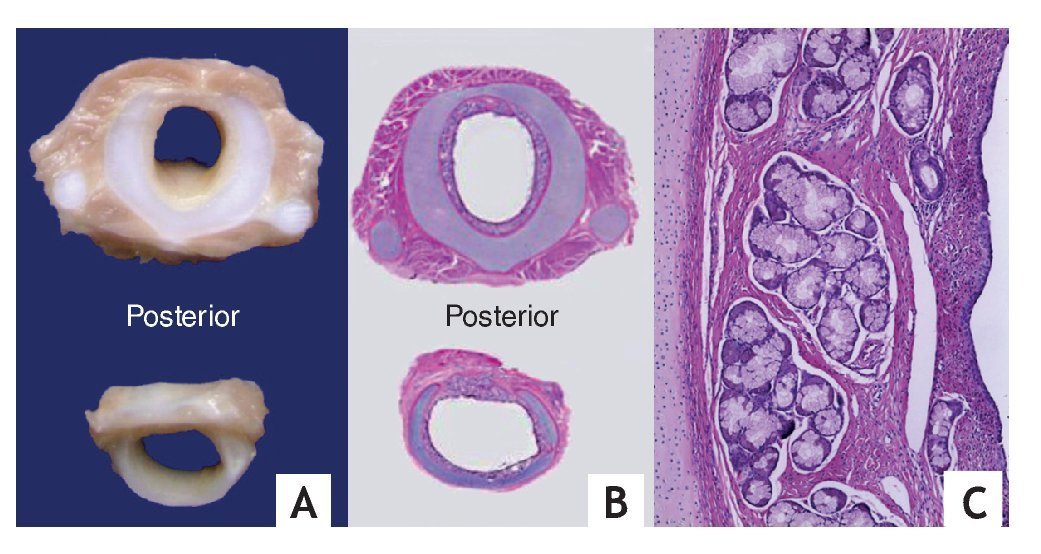
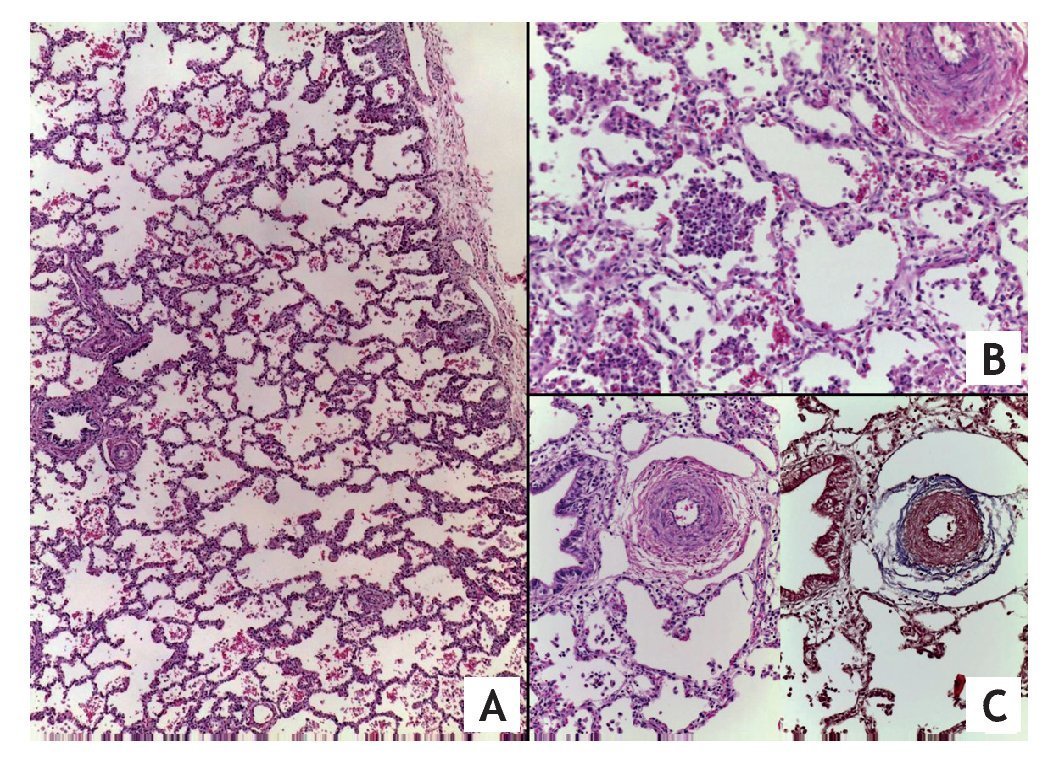
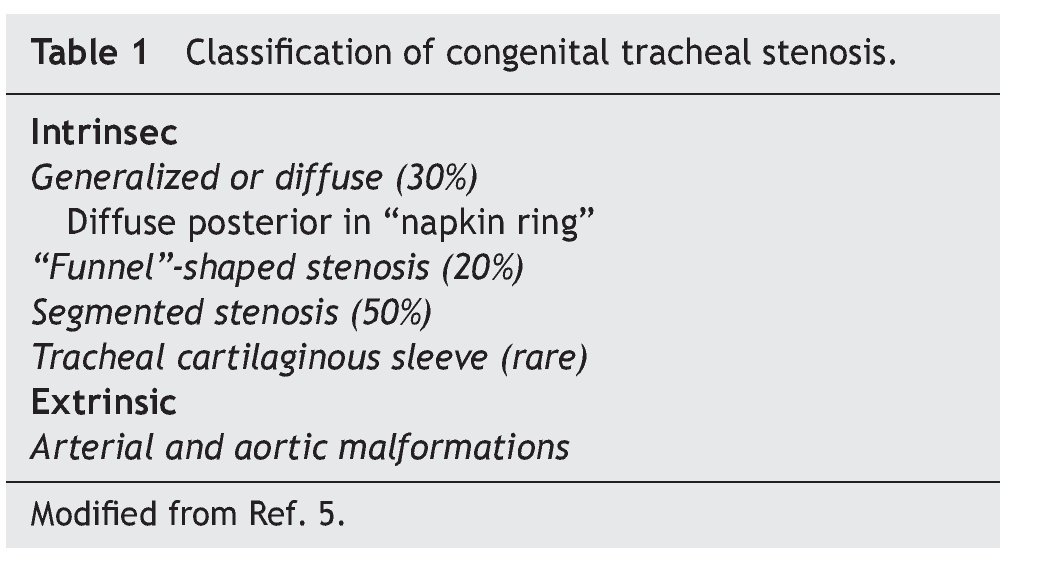
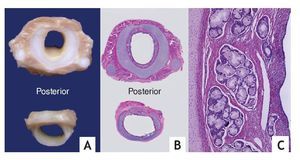
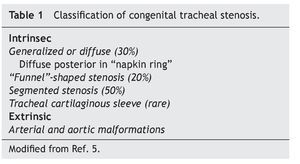
Serial cross-sections of the larynx, trachea and main bronchi showed larynx with edematous mucosa and no other alterations. Reduction of 50% of the tracheal lumen in a long segment was confirmed, from the infraglottic region to the region of the carina. This was in accord with the presence of complete tracheal rings secondary to their posterior fusion in "napkin ring" instead of normal rings seen on the posterior face of the membranous part (Fig. 3). In a microscopic study of the rings, hyaline cartilage with normal histology was seen, which confirms the diagnosis of posterior diffuse congenital tracheal stenosis in accordance with the classification proposed by Landing and Wells (Table 1).5
Figure 3 (A). Cross sections of the trachea at the level of the stenosis showing complete cartilages. (B) Histologically the posterior "napkin ring" fusion is verified. (C) The hyaline cartilage is normal and lymphocyte infiltrate is observed in the mucosa.
The rare combination of tracheal stenosis and unilateral pulmonary aplasia has been recognized to be lethal and patient survival is related with the extent of stenosis and the possibility of having corrective surgery.6 The heart presented dilation of the right cavities. Pulmonary artery trunk was dilated and gave origin to the right pulmonary artery. The left pulmonary artery was not identified and a persistent left superior vena cava was noted. There was atrioventricular and arterial ventricle concordance without other alterations.
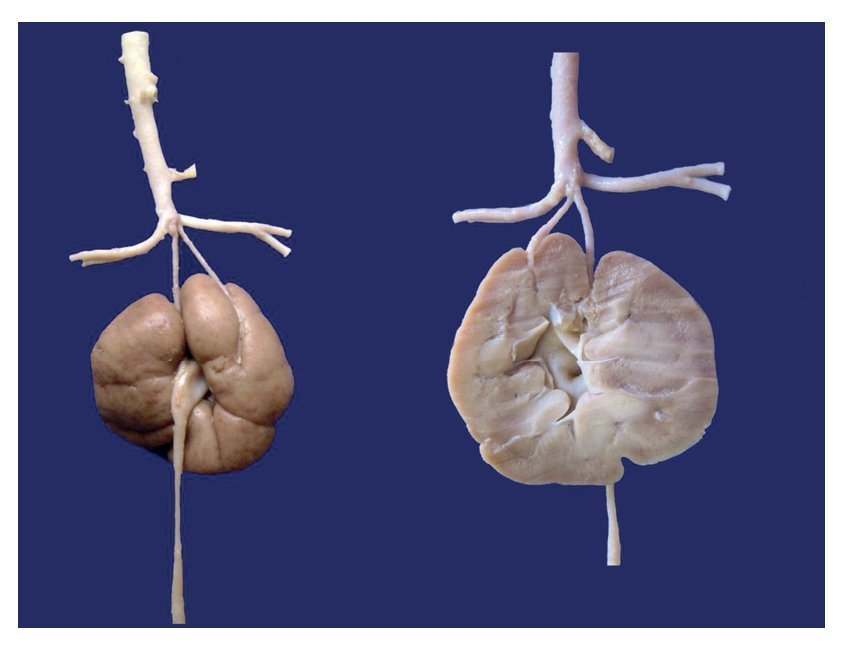
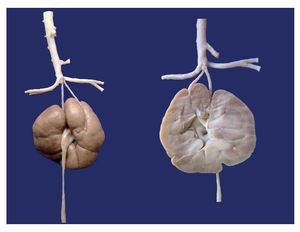
The following congenital malformations were also found in this patient: renal fusion with sole ureter and anomalous origin of the renal arteries of the terminal portion of the aorta (Fig. 4).
Figure 4 Anterior and posterior aspects of the fused kidneys. Ureter originates from the collecting system. The renal arteries originate from the terminal aorta.
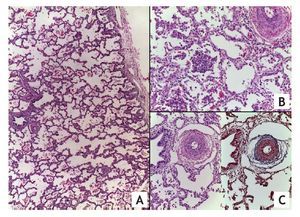
Well-developed parenchyma with areas of infiltrate of multifocal intraalveolar by neutrophils and recent hemorrhage is observed in the histopathological study of the right lung. The arteries and arterioles are of medium caliber. Data from pulmonary vascular disease are characterized by increase of the connective tissue of the adventitia, hyperplasia and hypertrophy of the muscle layer with reduction of the lumen (Fig. 5).7
Figure 5 (A). Well-developed lung parenchyma (HE x20). (B) Area of pneumonia with multiple intra-alveolar polymorphic nuclei. (C) Hyperplasia of the media and increased connective tissue in the adventitia of the arteries secondary to pulmonary vascular disease.
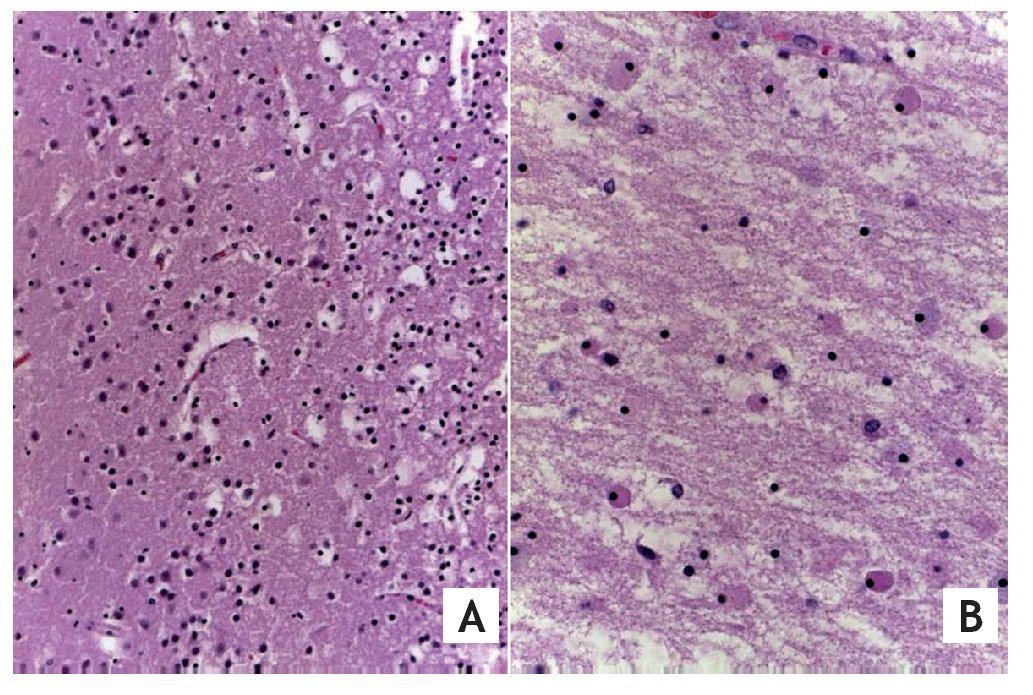
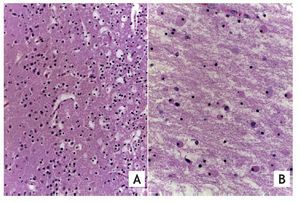
Secondary to the outpatient event of prolonged cardiac arrest, the patient developed ischemic hypoxic encephalopathy with cerebral edema and encephalomalacia (Fig. 6), morphological data of liver shock, myocardium, intestine and acute tubular necrosis. Sepsis diagnosis was made by the presence of acute pneumonia, acute laryngo tracheitis and postmortem cultures positive in blood and intestines for Klebsiella pneumoniae.
Figure 6 (A) Cerebral cortex of the best preserved areas where their layers are still recognized, with data of edema and neuronal necrosis. (B) White matter shows edema, neutrophil fragmentation and necrosis of glial cells (HE x40).
3. Final diagnoses
Left pulmonary aplasia with ipsilateral pulmonary artery agenesis associated with diffuse posterior intrinsic tracheal stenosis (in "napkin ring").
Associated malformations
* Left bronchus in blind pouch
* Left lung pseudoisomerism
— Long right main bronchus
— Right lung with two lobes
* Persistent left superior vena cava
* Anomalous origin of renal arteries of terminal aorta
* Renal fusion with sole ureter
Concomitant alterations
* Grade B pulmonary vascular disease
* Dilatation of the trunk of the pulmonary artery and right cavities
* Acute community-acquired pneumonia
* Sepsis due to Klebsiella pneumoniae
* Status post-unwitnessed cardiac arrest
* Hypoxic/ischemic encephalopathy with severe cerebral edema (600 g vs. 489 g)
* Encephalomalacia
* Morphological data of multivisceral shock
* Right cryptorchidism
3.1. Endoscopy Service (Dr. Gustavo Teyssier Morales)
The age at which these patients should be intervened depends on the severity of the stenosis and on the symptoms presented by the patient. It is preferable that children have several months of life and be of adequate weight, studies have been completed and that other congenital malformations have been ruled out, mainly cardiac malformations. Patients should have computerized axial tomography with reconstructions that allows us to plan for the most appropriate surgical technique due its nature as a high-risk surgery.
The recommended surgery is a slide tracheoplasty, which is done through a sternotomy and with extracorporeal circulation. Five of these surgeries have been carried out in the Thoracic Surgery Service to date. Four of the patients are found to be at home and in good condition. The other patient died due to sepsis. The youngest patient operated on was 1 month of age. These children are seen weekly to monitor their progress. In case there is increased respiratory difficulty or problems with feeding, they are scheduled for surgery as quickly as possible.
In analyzing this case, it is believed that the patient did not have a very critical airway. However, it was not taken into account that he also had pulmonary aplasia; therefore, he should have been re-assessed prior to the studies being completed and prior to operation. Unfortunately, it was not possible due to the lung infection.
3.2. Cardiology Service (Dr. Julio Erdmenger Orellana)
According to the last consensus done in Panama (2011), pulmonary hypertension in a pediatric patient is divided into ten categories in accordance with the etiology. This case is found within the first category, which encompasses the agenesis or pulmonary malformations originating in utero. Due to having only one pulmonary artery that manages the total pulmonary output, it causes an increase in pressure.8 Sildenafil is a selective pulmonary dilator and has been used for heart diseases with elevated pulmonary pressure; however, it should not be indicated in congenital heart diseases that cause a pulmonary hyperflow and whose management is surgical. In this case its use was highly questionable because there are no studies to support its use. It was used as a rescue method, with a proposed oral dose of 1-5 mg/kg/day every 8 to 12 h.
Diagnosis of pulmonary hypertension is made using echocardiogram. Normal pressure is 25 mmHg at rest, between 25 to 40 mmHg is considered to be mild hyper-tension, 40 to 60 mmHg as moderate hypertension, and >60 mmHg as severe hypertension.9
3.3. Neonatology Service (Dr. Mónica Villa Guillén)
Sildenafil has been used in neonates with acute pulmonary hypertension when there is no nitric oxide available or it has not worked properly. This drug has not been approved by the U.S. FDA for this age group. The latest study showed that its use increased mortality; therefore, it should only be used in individual patients and with strict monitoring.10
3.4. Department of Evaluation and Drug Assessment (Dr. Luis Jasso Gutiérrez)
There is a recommendation from the FDA published this year on the prohibition of the use of sildenafil in neonates based on a long-term follow-up study with these patients that showed an increase in mortality.11 Another possibility is to form a consensus among the different services of the hospital who use the drug in order to determine whether or not it should be used and in which cases.
3.5. Urology Service (Dr. Mario Díaz Pardo)
There are two ways to arrive at the diagnosis of these malformations. The most common is the presence of repeated urinary tract infections or as a radiological finding. The vast majority of patients are asymptomatic throughout their lifetime.
3.6. Emergency Department (Dr. Víctor Olivar López)
When and for how long the resuscitation maneuvers should be performed in a patient who arrives with cardiorespiratory arrest is a problem that has been exposed in different forums, mainly in regard to ethics. When a patient arrives at the emergency room with an unwitnessed cardiac arrest, we know that opportunities for survival are very low, but it is difficult to know if—and for which patients—resuscitation should be carried out. Those who should definitely not be resuscitated are those who have been dead for several hours.
Body temperature is one of the important pieces of data. This patient had a temperature of 32ºC, which would indicate death. However, he had no rigor mortis or lividity. It was taken into consideration that because he came from Huixquilucan, cardiac arrest occurred en route to the hospital. Therefore, there were indications that he should be resuscitated. As to the time, the American Heart Association recommends carrying out resuscitation for 15 min. In this case the resuscitation lasted 20 min so the prognosis was very poor. The recommendation would be that a patient with severe respiratory failure should be moved to the closest emergency room so that once stabilized, transfer can be accomplished.12
This was a very interesting and uncommon case of a patient with multiple congenital malformations—one of them of the airway. The first, a pulmonary aplasia alone would have allowed him to live a normal life with certain restrictions for strenuous physical activity. However, the second, a diffuse congenital tracheal stenosis, limited his ventilation and favored pulmonary infections for which some type of surgical intervention would have been required to increase the caliber. Due to the infections presented by the patient, it did not allow for a complete study and caused his death.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 18 February 2014;
accepted 25 February 2014
* Corresponding author.
E-mail: cabreramalu@aol.com (M.L. Cabrera Muñoz).