A 13-year-old female adolescent with abdominal pain syndrome, presenting with intolerance to the oral route, weight loss, and an abdominal mass.
1.1HistoryThirty-two-year-old mother, with secondary education, saleswoman, obese, who denies any drug abuse. Father who is apparently healthy and living outside of the family nucleus. A three-year-old sister, apparently healthy. A family history of diabetes mellitus on the mother side.
Born and living in Mexico City in a rented house with all basic urbanization commodities. Relevant zoonosis denied; with adequate hygiene and daily change of clothes and bathing.
She started eating a normal diet at one year of age. Currently, the patient refers a complete and balanced nutrition.
PSYCHOMOTOR DEVELOPMENT. Without any alterations for her age.
IMMUNIZATIONS. Referred as complete, without showing a vaccination schedule format.
The patient was the product of a first pregnancy with poor prenatal control. The mother denied folic acid or iron supplementation. Obstetric ultrasound performed at the fourth month of pregnancy. She was born through vaginal delivery at 40 weeks of gestation without any complications, breathing and crying at birth, weighing 2800g, with unknown length, and a 9/9 Apgar score. Discharged without any complications.
She referred penicillin allergy, and a history of traumatic amputation of the fourth finger on her right hand at the age of 3, and consequently a surgical history of a graft insertion at the site. She also reported a history of multiple fractures of her thoracic limbs when she was 6 years old and at different times.
She presented to a hospital with ascites and was hospitalized for eight days. A paracentesis was performed and the ascites fluid analysis reported a negative acid-fast stain and a carcinoembryonic antigen (CAE) of 7.71 IU.
She was referred to the Hospital Infantil de México Federico Gomez (HIMFG) for a diagnostic protocol of the abdominal mass.
1.2Final illnessShe presented with a 9-month history of insidious abdominal pain, which was progressive and of a colicky quality, localized to the mesogastrium which irradiated to the back, managed as a urinary tract infection and gastritis without any improvement. She lost approximately 8kg in one month.
She presented with intermittent vomiting episodes of scarce quantity, preceded with nausea and arching, and of gastro-alimentary content in a two-month period. A week before admission, she presented bilious vomit. These symptoms were accompanied by two months of intermittent diarrhea, with liquid depositions of scarce quantity, presenting up to three times a day, alternating with constipation.
A week before the admission, she had an episode of fever (39° C) with a duration of less than two hours.
The patient referred an increase abdominal girth of approximately 10cm a week before her admission.
Clinical examination of the patient revealed the following: a female patient with a weight of 62kg, height of 161cm, heart rate of 100 bpm, respiratory rate of 29rpm, blood pressure of 100/63mmHg, 36.5° C of temperature, and an abdominal girth of 96cm. She appeared younger than her chronological age, active, oriented, cooperative, with an adequate state of hydration, with paleness, normocephalic, without any bony indentations or exostosis. Spontaneous eye opening, pupils equal, reactive to light and normal accommodation. Adequate position of the ears, patent auditory canals, normal tympanic membranes. Permeable nares, without any secretions, with a full integrity of the septum, wide nasal bridge, and the oral mucosa adequately hydrated. Cylindrical neck without any adenopathy, centrally located movable trachea, symmetric thorax with a normodynamic precordium, rhythmic cardiac sounds with normal tone and intensity, without any murmurs, polypneic, with vesicular breath sounds without any abnormal sounds. Soft depressible abdomen, with tenderness to superficial and deep palpation, without signs of peritonitis, normal peristalsis, palpable liver 2cm below the costal margin, and a positive fluid wave test. Normal external genitalia, rectal examination not performed, limb hypotrophy.
Laboratory tests: Complete blood count: hemoglobin of 14.4g/dl, hematocrit of 43.3%, leukocytes of 7.8 x 103/μl, platelet count of 200 x 103/μl. Blood chemistry: creatinine of 0.6mg/dl, sodium of 141 mEq/l, potassium of 5 mEq/l, chloride of 103 mEq/l, total bilirubin of 0.86mg/dl, conjugate bilirubin of 0.37mg/dl; unconjugated bilirubin of 0.49mg/dl, total proteins 7.4g/dl, albumin of 3.9g/dl, alanine aminotransferase 26 IU/l, aspartate aminotransferase 15 IU/l, lactate dehydrogenase 156 IU/l, amylase 33 IU/l, lipase of 199 IU/l.
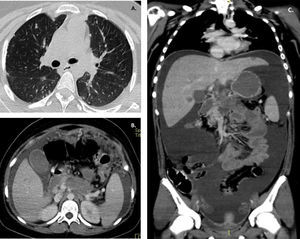
A thoraco-abdominal and pelvic computed tomography with double contrast and a lung window was performed. A lesion in the body and tail of the pancreas was found, suggestive of a neoplastic etiology. Pulmonary and hepatic nodules compatible with secondary deposits, and probable peritoneal implants. Free abdominal fluid, hepatosplenomegaly.
A diagnostic laparoscopy was performed, with the following findings: an abundant reddish brown fluid with a discrete whitish speckling; parietal peritoneum with a cotton-like infiltrate; liver with multiple lesions of ≤1cm, of a hard consistency, and in both lobules; an omentum with cobblestone appearance; all the structures were friable.
She presented with temperature fluctuations during the post-surgical care, with spiking high fevers, and signs of hypoperfusion. A clinical diagnosis of sepsis was integrated with a probable abdominal source. Broad-spectrum antibiotics were started with empiric activity against anaerobic Gram-negative bacilli and Enterococcus sp; piperacillin-tazobactam 300mg/kg/day, IV every eight hours.
In the clinicopathological session, the case was presented as a probable lesion dependent of the pancreas, with extensive infiltration to the peritoneum and liver, and probable infiltration to the bowel wall, the gastric antrum, and evidence of multiple pulmonary lesions.
Endoscopy with a biopsy and an octreotide scintigraphy were suggested to rule-out a pancreatic origin.
A SPECT-CT with somatostatin analogs showed uptake in the gastric antrum, which extended to the pancreas and the mesenteric ganglia, as well as small areas of uptake in the liver, lung and right mediastinal ganglia with a left pleural effusion. Free fluid in the abdominal cavity was found. A diagnosis of a probable gastric neuroendocrine tumor was made without any specification regarding the primary origin of the tumor (pancreatic or gastric).
A peridural catheter was placed by the algology service. She presented hyperkalemia of 6.4 mEq/l, and a pulseless ventricular tachycardia. A single cardiopulmonary resuscitation cycle was given and cardioversion with a dose of 4J/kg; this event lasted two minutes. The patient had a return to spontaneous circulation with sinus rhythm, and post-arrest arterial blood gases showing a metabolic acidosis and hyperlactatemia, with clinical signs of adequate perfusion; an orotracheal intubation was performed.
The patient underwent chemotherapy with doxorrubicin at a dose of 60mg/m2/day, dexrazoxane, cisplatin at a dose of 20mg/m2/day, leucovorin at a dose of 200mg/m2/day, and 5-fluoruracil (5-FU) at a dose of 600mg/m2/day.
The patient had a hemodynamically unstable clinical course, without any vasopressor support, with a decreased urinary output and a tendency to be tachycardic and hypertensive. She had supplementary oxygen support with a reservoir oxygen mask at a dose of 10 l/min, a Silverman score of 2 with minimal intercostal and xiphoid retraction. The abdominal pain persisted and was managed with a morphine infusion through the peridural catheter; additionally, she required morphine boluses. She presented eight episodes of vomiting. She presented bradycardia that progressed to asystole without response to basic resuscitation maneuvers.
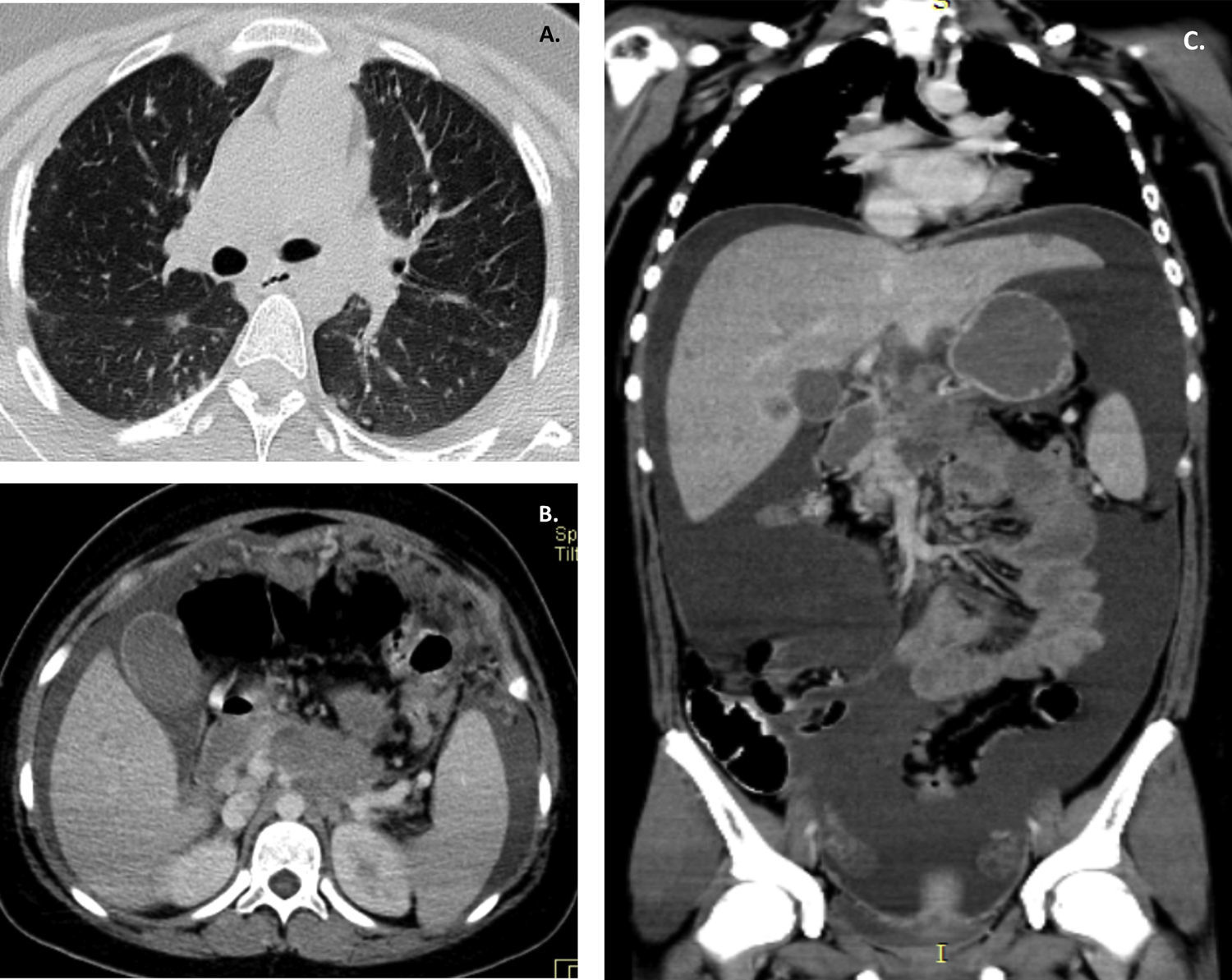
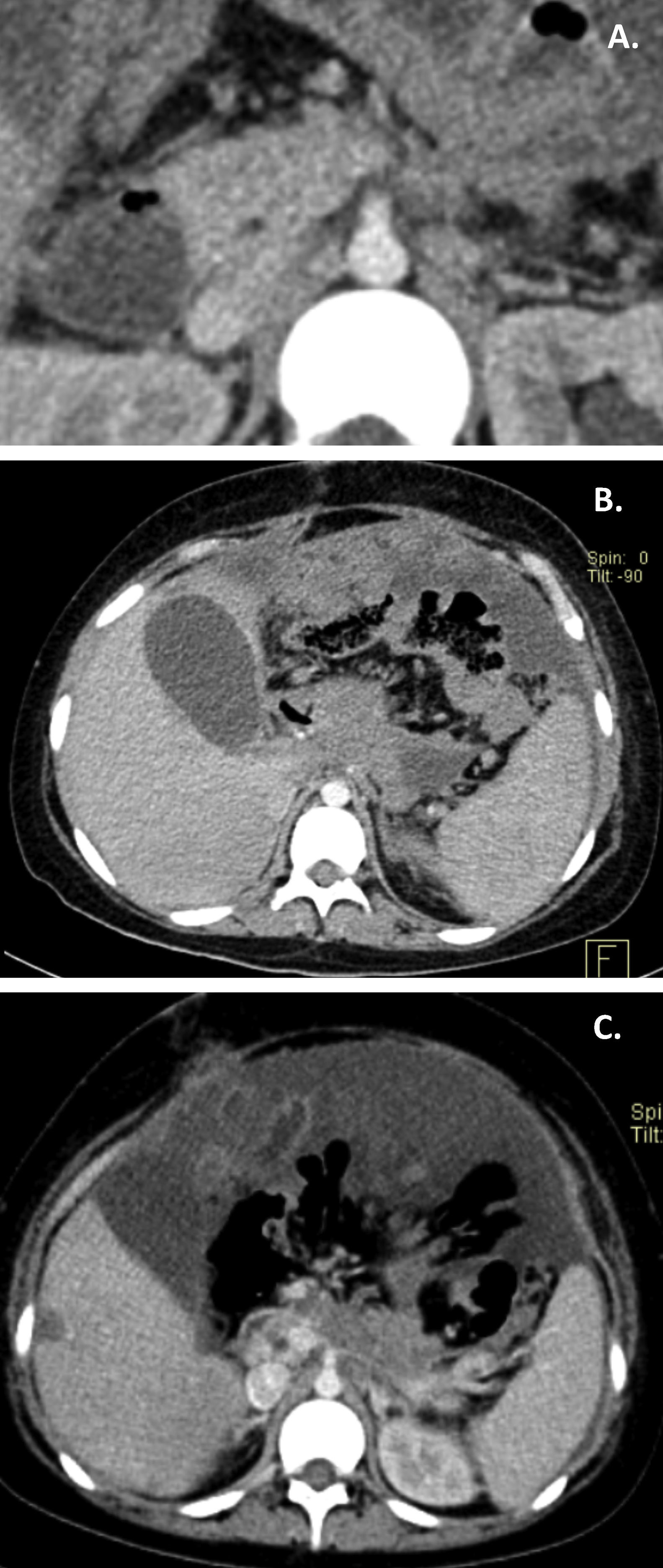
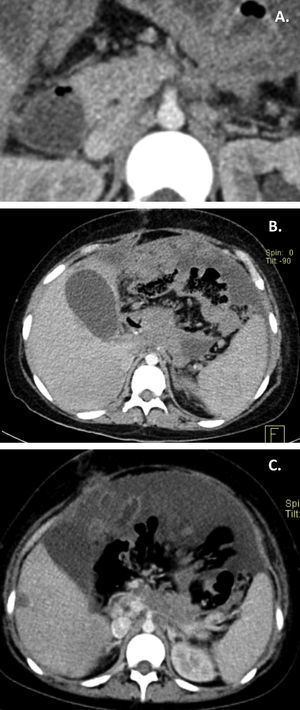
2ImagingRepresentative imaging studies of the lesions are presented. The axial cuts and lung window of the chest CT shows the lungs from the apices to the bases, with multiple nodular subpleural and pulmonary lesions, which are small but visible. Moreover, there is a left laminar pleural effusion (Fig. 1A). At the abdominal level, the intravenous contrast enhanced CT scan showed a lesion of irregular borders in the omental transcavity, partially defined, with loss of interface with the gastric wall, the anterior wall of the pancreas, and duodenum, which made impossible to determine the origin of the lesion (Fig. 1B). Vascular structures could not be adequately observed; the portal vein and the celiac trunk were compromised. Multiple nodular lesions were observed in the greater omentum. In the following CT cuts, multiple nodular lesions in the liver parenchyma with a discrete enhancement after contrast administration were observed (Fig. 1C). A follow-up triphasic CT scan (arterial, venous, and equilibrium phases) was ordered. In the venous phase, multiple nodular lesions adjacent to the pancreas were present (Fig. 2A). A diffuse gastric wall thickening and persistent ascites were noticed (Fig. 2B). In the last CT scan, seven months later, the subpleural lesions had increased in size and number. Notably, there were no observable lesions in the lung parenchyma. The liver lesions persisted (Fig. 2C).
A. Peripheral pulmonary lesions are shown. B. Multiple nodular lesions enhanced with the administration of contrast located to the major omentum and a great quantity of peritoneal fluid are observed. C. This coronal plane shows the extension of the fluid present that provoked the centralization of the intestinal loops.
A. The vascular structures keep their morphology. In both the venous and arterial phases it is observed that the celiac trunk as well as the portal vein are not adequately defined. B. Liver nodular lesions persist. C. The peritoneal nodular lesions have increased and the volume of the ascitic fluid previously observed has decreased.
Considering the three CT scans, a diagnosis of a probable neoplastic lesion in the omental transcavity, probably of gastric or pancreatic origin, with secondary hepatic and peritoneal deposits, ascites, and lung atelectasis was integrated.
3Case presentationThe case of an adolescent patient with an adenocarcinoma of a primary abdominal origin with neuroendocrine differentiation was presented.
The following syndromic diagnosis were integrated:
- •
Chronic abdominal pain, diffuse, generalized, and intense, associated with vomit and diarrhea, with increased abdominal girth
- •
Respiratory distress syndrome supported by tachypnea, associated with progressive respiratory restriction secondary to ascites
- •
Systemic inflammatory response syndrome supported by fever, tachycardia, tachypnea, leukopenia, and thrombocytopenia
- •
Infectious syndrome supported by the previously described information and Enterobacteriaceae infection
- •
Multiple organ dysfunction syndrome with cardiovascular, hematologic, and respiratory systems failure
- •
Hemorrhagic syndrome, with epistaxis and thrombocytopenia
- •
Anemic syndrome characterized by paleness, tachycardia, and hemoglobin levels below normal values by age group
The following nosological diagnoses were integrated:
- •
Adenocarcinoma with lung, liver, and gastric metastasis, probably of pancreatic origin
- •
Peritoneal carcinomatosis
- •
Malignant ascites with ascitic fluid and positive cytology
- •
Abdominal hypertension supported by the increased abdominal girth caused by ascites, with a secondary ventilator restriction
The time of evolution of the disease represents one of the most important prognostic factors for the outcome of this patient. The abdominal pain had a 9-month history; it was not adequately managed from the beginning, which was a factor that determined the prompt referral to a specialist and influenced the final prognosis. The patient was treated for multiple diagnosis, in multiple occasions, without any improvement or any clinical signs of a urinary tract infection or peptic-ulcer disease, for which she was treated, emphasizing that a complete semiology of abdominal pain along with a clinical history represent key elements in the clinical examination of a pediatric patient. When weight loss, diarrhea, vomit, and an increase in abdominal girth manifest, this translates into a more chronic illness and darkens the prognosis.
The clinical examination of a patient with chronic abdominal pain is crucial. It should be detailed and meticulous, with the objective of identifying abdominal tumors. Starting with inspection, abdominal distension can be identified, and with palpation both a palpable mass and ascites can be detected. Moreover, the origin and situation of the tumor can be determined by an indirect manner. If it is movable, an intraperitoneal localization can be inferred. In contrast, retroperitoneal tumors usually do not move, and generally occupy the renal fossa. The principles of the clinical examination in the daily revision of patients should not be forgotten. In this case, with an adequate clinical examination, an abdominal tumor could have been identified, and early abdominal imaging and extension studies would have been ordered, which could have derived in timely treatment.
There are plenty of causes of ascites, among which the hepatic, biliary, cardiac, renal or urinary, gastrointestinal, pancreatic, gynecological, infectious, and even genetic, should be investigated and managed.
In the study of the ascitic fluid, the cellular count of proteins was not specified. An abnormal carcinoembryonic level was reported, although this result is not specific given the variety of diagnoses that could originate this finding.
At the HIMFG, a CT scan study evidenced an intraabdominal tumor with invasion of the retroperitoneum, localized to the head and body of the pancreas, of heterogeneous characteristics, irregular borders, and with a local extension to the gastric antrum. Since the first imaging study, metastatic disease was noted with the presence of nodular lesions in the liver, pleura, lungs, as well as ascitic fluid.
The initial surgical conduct was considered as adequate, with exploratory laparotomy and biopsy for staging. The intraoperative findings confirmed peritoneal carcinomatosis.
It should be noted that tumor markers are usually proteins that have been related to neoplastic processes. These markers can be determined directly from the tumor, peripheral blood, lymph nodes, bone marrow, cerebrospinal fluid, urine, and even feces. Alpha-fetoprotein is synthesized in the yolk sac of the fetus, in the liver early in life and in the digestive tract. Levels decrease to less than 10 ng/ml at 9 months of age. Levels increase with germinal cell tumors, hepatoblastoma and with some hepatocellular carcinomas. Human chorionic gonadotropin is released within the syncytiotrophoblast and its normal levels should be less than 1 ng/ml. Similarly, the levels increase in germinal cell tumors. Finally, carcinoembryonic antigen is a oncofetal glycoprotein normally expressed in mucous cells that increases in adenocarcinomas. However, any benefit in the pediatric population has not been demonstrated; furthermore, it is usually specific of colorectal carcinomas.
Ideally, as a part of the diagnostic approach in this patient, levels of CA19-9 antigen should have been ordered if the clinical suspicion was of a primary pancreatic neoplasm since it is usually very elevated.
The histopathological report described an adenocarcinoma with neuroendocrine differentiation. Peritoneal carcinomatosis caused by a neuroendocrine tumor is very rare, and currently there are not enough data regarding its prevalence and treatment. Up to 80% of patients present with synchronic peritoneal carcinomatosis and liver metastasis at diagnosis. Worldwide, only 47 cases that presented peritoneal carcinomatosis secondary to neuroendocrine tumors have been reported in adults, mostly originating from the midgut.
The diagnostic approach was adequate and well planned, initially with an imaging study, peritoneal fluid, and with extension studies than included endoscopy and somatostatin receptor scintigraphy that revealed gastric antrum, mesentery, and mediastinum compromise.
According to the intraoperative findings, the tumor was classified as a Gilly stage IV, the most advanced stage given the presence of a diffuse tumors of more than 2cm in diameter. The peritoneal carcinomatosis index determines the involvement of the abdominal cavity by peritoneal implants: with a score greater than 20 the disease is considered to be advanced and unresectable; in this particular case, the score was close to this number.
The endoscopic study evidenced extrinsic gastric compression, without infiltration of neoplastic cells to the gastric mucosa. Regarding surgical treatment, it must be directed towards diminishing the comorbidities secondary to intestinal obstruction.
The international consensus indicates what should have been offered in this case: two cycles of chemotherapy, meaning over six weeks. Afterwards, radical surgical treatment with an extended Whipple pancreaticoduodenectomy with antrectomy and debunking surgery, with the intention of resecting all the macroscopically visible peritoneal implants. At this surgical time, intraperitoneal chemotherapy should have been administered in either of two modalities, local or hyperthermic. According to the surgical criteria, a non-anatomic wedge resection of liver nodules should be performed, and a thoracotomy with metastasectomy could be done in a single surgical time or it can be deferred to a second surgical time. Despite combined medical and radical surgical treatment, the survival prognosis barely reaches 30%.
Regarding the carcinoid syndrome, the following symptoms should be considered: chronic abdominal pain, facial flushing and telangiectasia, chronic diarrhea, tachycardia, arterial hypotension, and respiratory distress. Medical treatment is the cornerstone, as it is performed with the administration of somatostatin analogs, which can be administered parenterally in a continuous infusion, and even by intratumoral delivery. This therapy has the objective of diminishing gastrointestinal, enteric, biliary or pancreatic secretions, as well as those of carcinoid tumors.
Finally, medical treatment is directed to alleviating symptoms of intestinal obstruction and includes a low-residue diet, antispasmodics, analgesics, antiemetics, anticholinergics, and somatostatin analogs. In cases of frank occlusion, a nasogastric tube is required for decompression with continuous suction, gastrostomy, and even a jejunostomy if required.
The cornerstone of the oncologic treatment is mitomycin C, platinum derivatives and 5-FU, although the experience is limited in the pediatric population. After the beginning of chemotherapy, the evolution was torpid, although expected, with febrile neutropenia, severe sepsis, and septic shock. Despite having received adequate antibiotic coverage, the status of the patient did not improve.
The final diagnosis and cause of death were the following:
- •
Peritoneal carcinomatosis secondary to a neuroendocrine gastroenteropancreatic adenocarcinoma
- •
Liver, pleura, and lung metastasis
- •
Septic shock
- •
Secondary multiple organ dysfunction
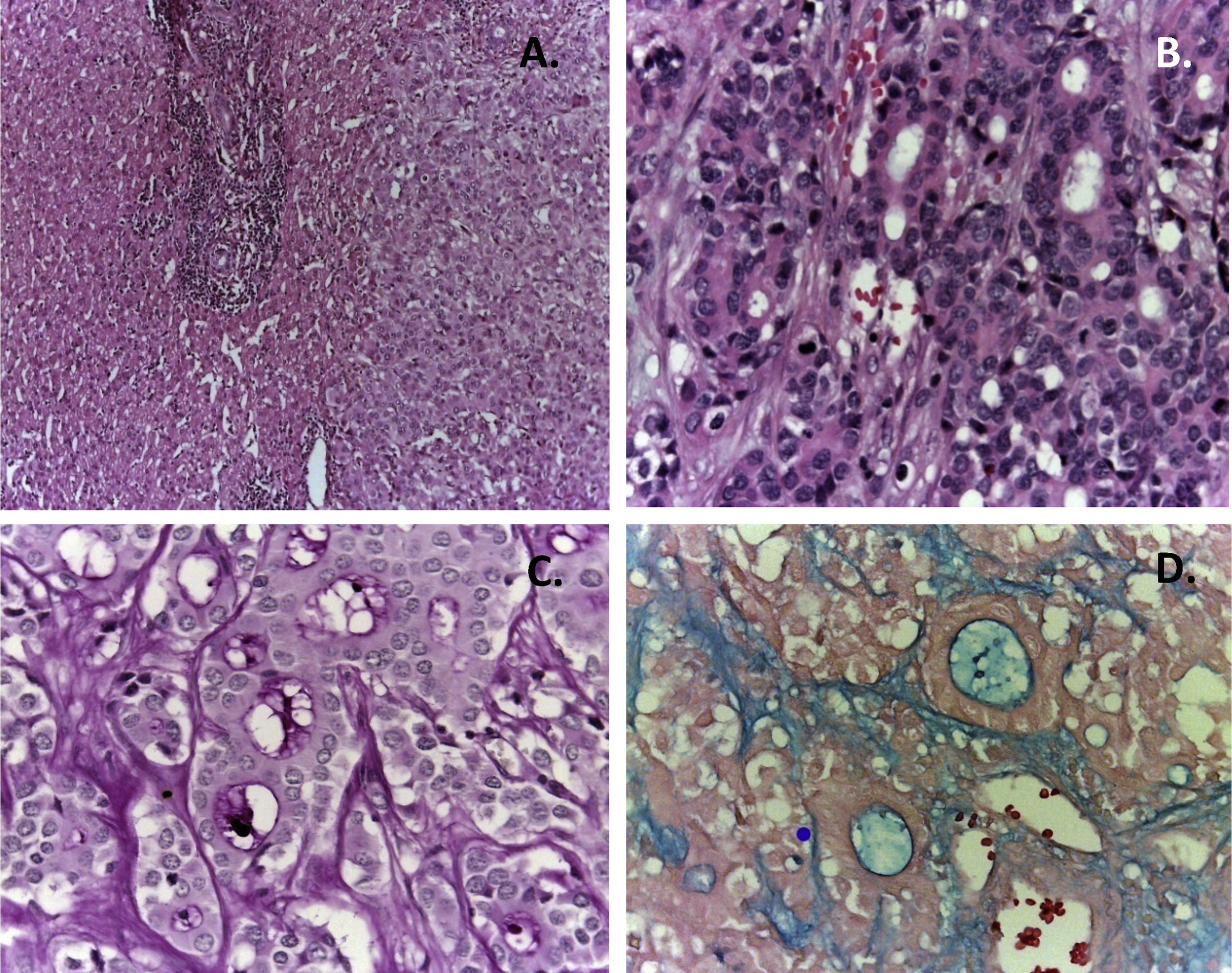
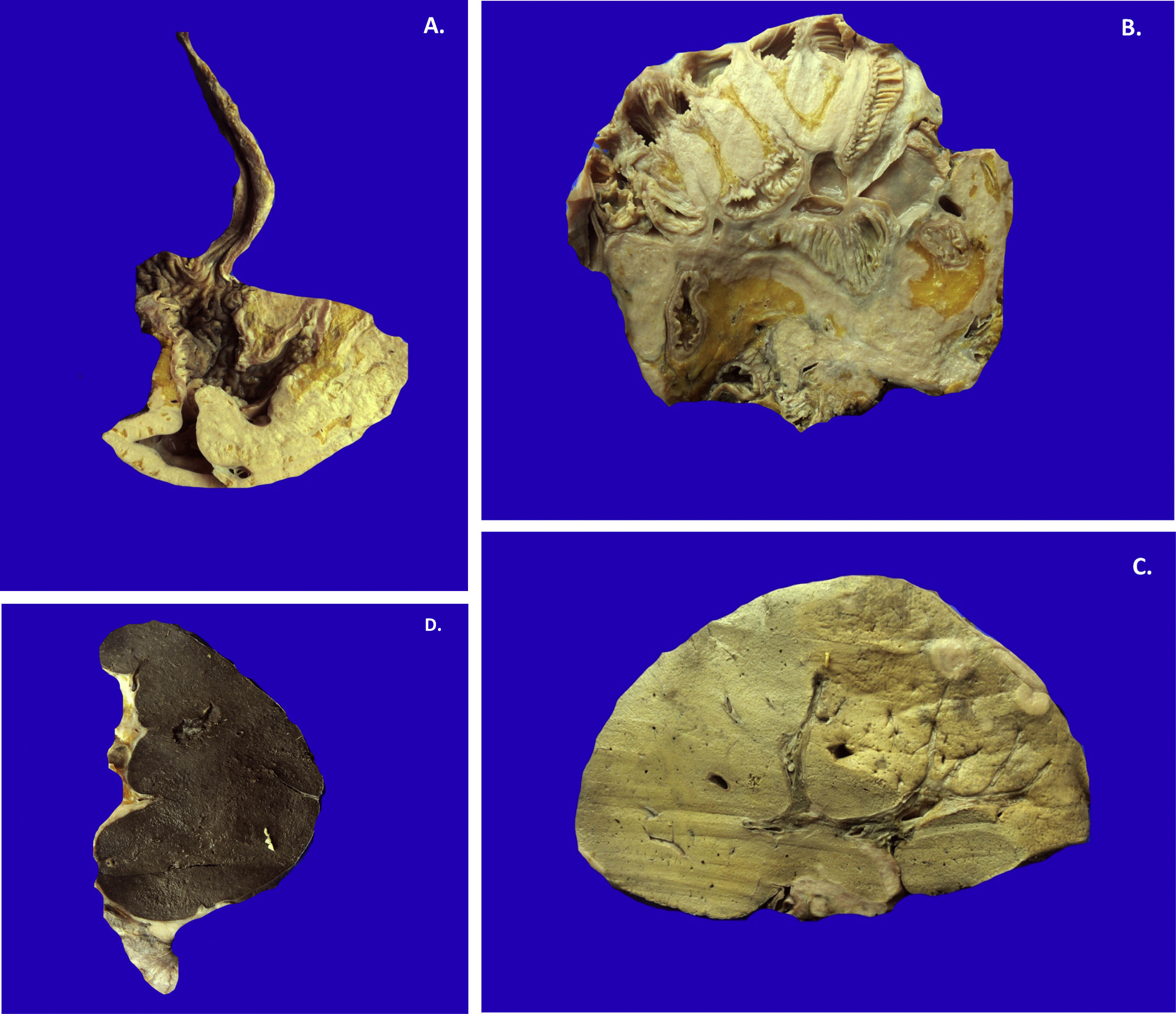
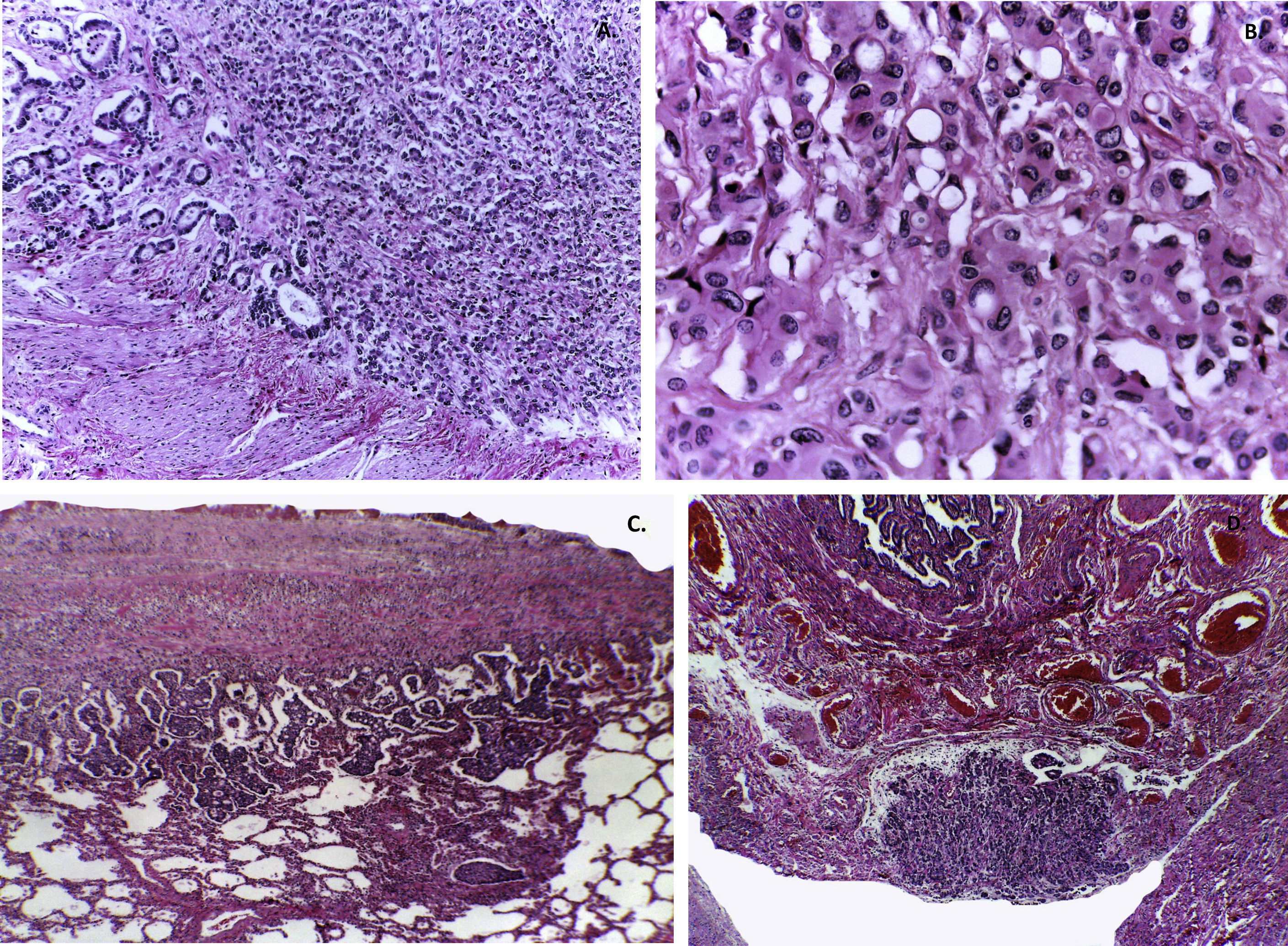
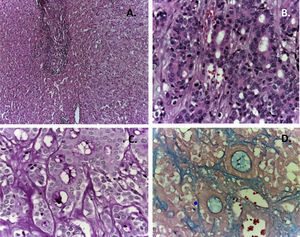
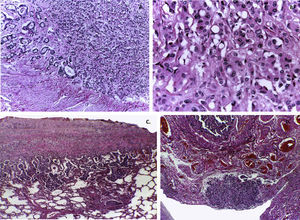
The first contact with the patient was through a sample of ascitic fluid and two biopsies, one of the liver and one of the omentum. In the ascitic fluid, a hemorrhagic background was observed with inflammatory cells and small groups of epithelial cells with and abundant cytoplasm and an apparent nucleolus. The liver biopsy showed a non-neoplastic parenchyma, a portal space with a moderate inflammatory infiltrate that compromised the sinusoids and a neoplasm of epithelial aspect. The tumor presented two morphological patterns: the first, which formed glandular structures of different sizes that produced a basophile material, and the second, an area constituted of monotonous cells that formed nests, which was different to the cells that formed the glandular structures (Fig. 3A and B). Appropriate stains and immunohistochemistry were performed to determine the origin of this neoplasm. With the PAS stain (Schiff's periodic acid stain) the product of the glands was positive (Fig. 3C). The stain characteristics were fixed after diastase administration and resulted positive for alcian blue stain, which translates as the presence of acid mucosubstances (Fig. 3D). With hematoxylin and eosin stain, and special stains, a pancreatic, gastric, or colonic origin was proposed.
Liver biopsy shows a neoplasm with two histological patterns. A. In the first, the morphology shows monotonous cellular nests. B. In the second, the formation of glandular structures is present, revealing an epithelial origin. PAS (C) and alcian blue (D) stains show the presence of acid mucosubstances.
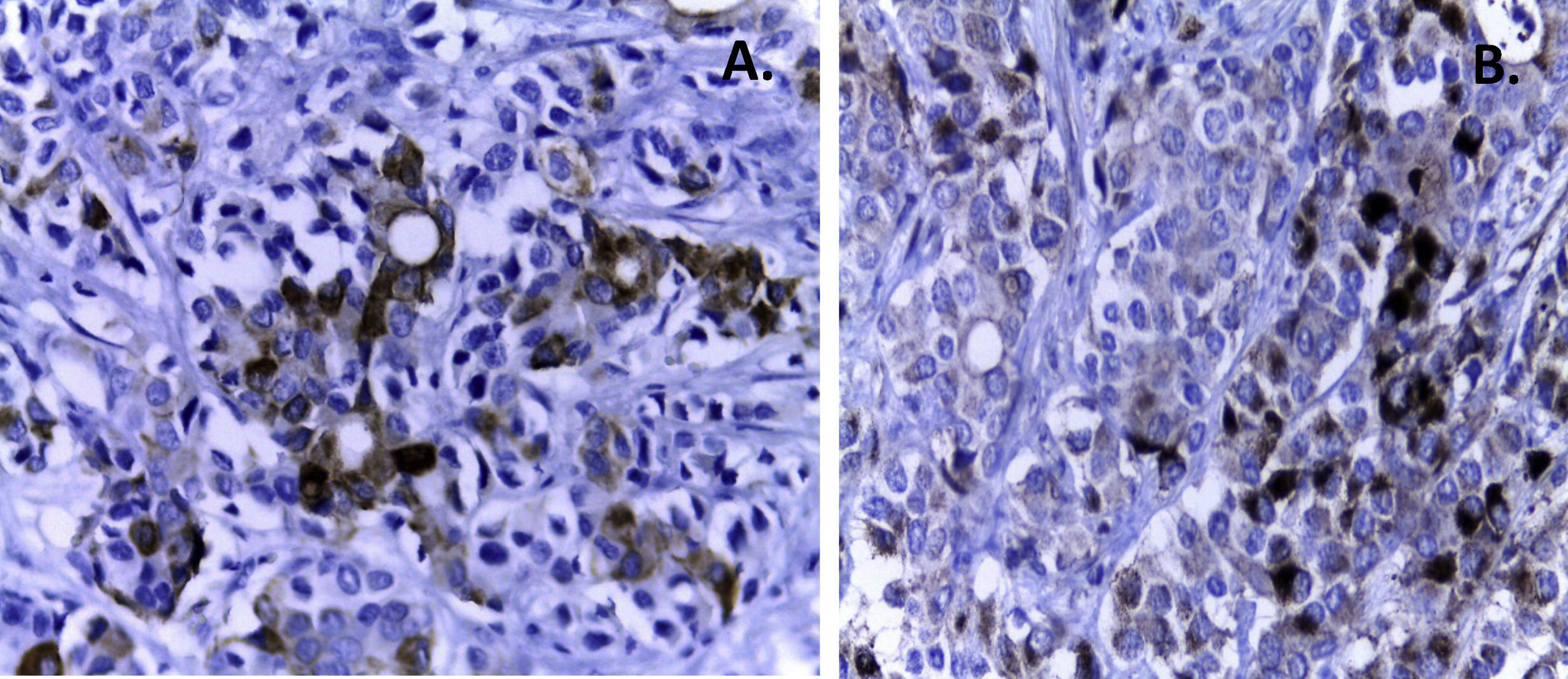
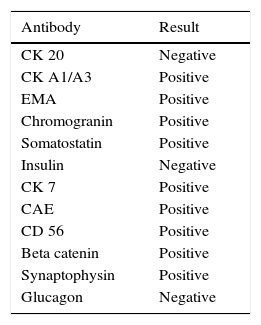
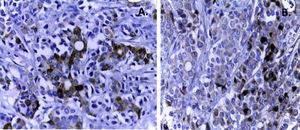
Subsequently, immunohistochemistry was performed. In the epithelial markers panel, carcinoembryonic antigen, epithelial membrane, and cytokeratin tested positive in the glandular structures (Fig. 4A), and negative where the tumor had a neuroendocrine pattern (Fig. 4B). Two of the most relevant antibodies are cytokeratin 7 and beta-catenin, which test positive in primary tumors of the esophagus and negative in primary neoplasm of the colon. Colorectal carcinoma gives a positive result for cytokeratin 20 but negative to cytokeratin 7. Cytokeratin 20 was negative. These results can rule-out the colon as a primary organ. Moreover, cytokeratin 7 is not frequent in tumors of the pancreas. The neuroendocrine markers, chromogranin, synaptophysin and somatostatin, were positive in zones of neuroendocrine appearance and negative in the zone of epithelial appearance with formation of glands (Table 1).
Immunohistochemistry profile.
| Antibody | Result |
|---|---|
| CK 20 | Negative |
| CK A1/A3 | Positive |
| EMA | Positive |
| Chromogranin | Positive |
| Somatostatin | Positive |
| Insulin | Negative |
| CK 7 | Positive |
| CAE | Positive |
| CD 56 | Positive |
| Beta catenin | Positive |
| Synaptophysin | Positive |
| Glucagon | Negative |
DX: adenocarcinoma with neuroendocrine differentiation.
CK, cytokeratin; EMA, endomysial antibody; CAE, carcinoembryonic antigen.
This immunohistochemistry profile suggests a primary pancreatic, gastric or ovary tumor.
The ascitic fluid was positive for neoplastic cells. Subsequently, gastric and esophageal biopsies were received, which tested negative for neoplastic cells.
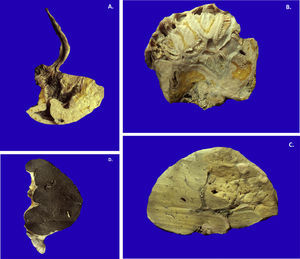
In the necropsy, the neoplasm was confirmed to be a type of gastric cancer (linitis plastica). This tumor infiltrates and thickens the gastric wall but spares the mucosa, which explains the endoscopic appearance of extrinsic compression without an observable tumor (Fig. 5A). This tumor extended through the serosa and compromised the head of the pancreas.
A. Gastric linitis plastica disseminated throughout the wall, sparing the mucosa. B. The extensive lymphatic dissemination and through the serosa led to peritoneal carcinomatosis. Intestinal loops are immersed in the neoplasm. C. Hematogenous dissemination originated multiple liver metastasis. D. The neoplasm infiltrated the splenic capsule, which it appears to be thickened, of a yellow whitish color, and the lymph nodes.
In the gastric neoplasm, two components were observed: the glandular and the neuroendocrine.
Gastric adenocarcinoma is a very uncommon neoplasm before age 20. It represents approximately 1% of all gastric tumors; the most frequent are lymphomas and sarcomas.
Another key element is the presence of the so-called signet-ring cells, where the cytoplasm is observed as a vacuole that displaces the nucleus and gives the cell a ring-like appearance. These cells are found throughout the whole extent of the neoplasm. Signet-ring cells carcinoma have been described in the pancreas, without this appearance.
The neoplasm extended practically to all serosa, compromised the adipose tissue surrounding the stomach, and conditioned peritoneal carcinomatosis. There was a complete compression of the intestinal loops by the neoplasm (Fig. 5B). The tumor presented an extensive dissemination that practically occluded the whole abdomen, which made impossible for any segment to be resected.
There was infiltration of the head of the pancreas. Alterations were not identified in Wirsung's duct, the body, and the tail of the pancreas. Neoplastic cells in the duodenum and the zone where the pancreatic duct drains were also not found.
The liver showed metastasis (Fig. 5C). The spleen also presented with extensive infiltration of the capsule, without affecting the parenchyma (Fig. 5D). Both kidneys were found to be increased in size and weight.
There was an extensive lymphatic dissemination in the lungs which affected the pleura, leading to a desmoplastic reaction and focal invasion to the parenchyma in several zones (Fig. 6). The lungs showed signs of hemorrhage and bacterial proliferation.
A. The gastric wall is infiltrated by a poor differentiated neoplasm. B. The production of mucosubstances is intracellular, which originates the so-called signet-ring cells. Tumor dissemination was extensive both lymphatic and hematogenous. C. The pleura is compromised and focally the lung parenchyma. D. The pelvic soft tissues show infiltration by the neoplasm; the serosa of a salpinx is observed.
Carcinomatosis was found in the uterus, fallopian tubes, ovaries, bladder, and soft tissues surrounding the uterus. Histologically, the uterus, bladder, fallopian tubes (Fig. 6D), and the ovaries were infiltrated by the neoplasm.
The bone marrow was acellular, with very few lymphocytes and erythrocytes, which explains the extensive bacterial proliferation without inflammatory response. The main disease was a gastric adenocarcinoma with signet-ring cells and endocrine differentiation.
Gastric carcinomas are infrequent in young patients. When present with signet-ring cells, approximately 25% show an endocrine differentiation, with extensive dissemination through the serosa and lymphatic vessels to the peritoneum, mesentery, serosa, small intestine, colon, rectum, uterus, pancreas, lungs, ovaries, and practically to all the lymph chains.
Signet-ring cells carcinoma has a survival rate of less than a year, according to published data in adults. These tumors have a rapid progression. Experience in children is scarce. In the last 10 years, three cases of gastric carcinoma have been treated at the HIMFG, including the present case.
4.1Final diagnosisGastric adenocarcinoma with signet-ring cells, endocrine differentiation, and lymphatic and hematogenous extensive dissemination to the parietal peritoneum, mesentery, small intestine serosa, colon, rectum, uterus, pancreas, lungs, ovaries, around the fallopian tubes, and to mediastinal, mesenteric, periaortic and peripancreatic lymph chains.
4.2Concomitant alterations- •
Malignant ascites (500ml)
- •
Abdominal wall collateral venous circulation
- •
Left pleural effusion (500ml, serohematic)
- •
Post-laparotomy status with wedge liver biopsy and partial omentectomy
- •
Post-endoscopy status chronic superficial gastritis
- •
Post-subclavian central venous catheter placement status
- •
Post-epidural catheter placement status
- •
Brain edema (OW 1150g/EW 1296g)
- •
Hepatomegaly (OW 2600g/EW 1050g)
- •
Splenomegaly (OW 400g/EW 129g)
- •
Bilateral nephromegaly (RK OW 300g/EW 101g; LK OW 200g/EW 108g)
Neuroendocrine tumors are infrequent neoplasms in the pediatric age, for which the opinion of several specialists was requested to have a complete view of the approach to these cases, which present with diverse manifestations, and because a timely detection is important.
The frequency of these tumors in children and adolescents is very low; in adult patients, the incidence is of 2-5 cases per 100 000 habitants per year, usually sporadic. Some have been related to hereditary syndromes, such as multiple endocrine neoplasia type 1 and 2, Von Hippel-Lindau syndrome and neurofibromatosis type 1.
This great variety of neoplasms include the neuroendocrine gastroenteropancreatic tumor, neuroendocrine neoplasms of unknown primary site, catecholamine producing tumors, neuro-adenohypophysary tumor, thyroid medullary carcinoma, neuroendocrine carcinoma, and pulmonary neuroendocrine tumor. Within these tumors, the most common are the neuroendocrine gastroenteropancreatic tumors, which are divided in functioning and non-functioning. Symptoms vary according to the type of substances released in the circulation, the localization, and the size of the tumor. Most of these tumors are non-functioning and the symptomatology is non-specific. The most common symptoms are the presence of abdominal pain, which usually is intermittent, a long course of the disease, and the presence of vomit, nausea, and anemia due to gastrointestinal bleeding can be concomitant.1–3 Abdominal pain can be related with tumor invasion, intestinal obstruction or mesenteric ischemia. Because the symptoms have a low specificity, an obvious symptomatology in the case of non-functioning tumors only appears when these exert a direct effect on one of the organs where they are located or when they present with liver metastasis. Due to the low specificity, a late detection of these tumors is common, and in many occasions, it occurs during an exploratory surgical procedure or with an imaging study assessment. In approximately 20% of neuroendocrine tumor cases, a clinical entity known as carcinoid syndrome is present, which is characterized by facial, neck and upper thorax flushing, with absent sweating, and concomitant tachycardia, diarrhea, rhinorrhea, and excessive tearing.
In the case of functioning tumors, the symptomatology depends on the substance that these tumors release. For example, in the case of insulinomas, patients present with diaphoresis, fatigue, loss of consciousness, usually after feeding. With gastrinomas, patients with peptic ulcers and diarrhea are usually observed. Patients with glucagonomas present weight loss, diarrhea and diabetes. With somatostinomas, the symptomatology is similar: weight loss, diabetes, cholelythiasis, abdominal pain, diarrhea. In VIPomas, patients present with watery diarrhea and hypokalemia.4–8
5.2Hemato-oncology ServiceIn these type of tumors, a two-cycle chemotherapy scheme is given, with the intention of limiting the tumor, decreasing tumor burden, carcinomatosis and trying to eliminate metastatic lesions. Subsequently, the tumor is treated surgically. If the diagnosis is not confirmed, treatment with a scheme that includes platinum, 5-FU, and an anthracycline can be administered; this scheme is useful for carcinomas presenting at pediatric and adult ages.
Furthermore, the concept of palliative care comprises the attention to the patient's needs. In this case, the patient required a chemotherapy treatment with the intention of decreasing the size of the tumor.
5.3Oncologic Surgery ServiceFor almost over 15 years, this is the third case of a gastric carcinoma managed at the HIMFG. In contrast with the present case, the other two cases did not present this neuroendocrine differentiation. In this patient, the diagnostic approach was initiated with a laparoscopy turned into a laparotomy, which was limited to obtaining tissue for the histopathological study. Apparently, in the second CT scan, a certain degree of response to chemotherapy was observed, with a certain decrease of volume and the quantity of ascites. The planned treatment included a second period of chemotherapy. Subsequently, an attempt to resect the primary tumor with cytoreductive or debunking surgery of the peritoneal disease was performed, according to recommendations by the European Society of Neuroendocrine Tumors. In this case, the patient was not a candidate to resection of the primary tumor because of the infiltration to the mesentery and the rest of the peritoneal surfaces.
Had the patient responded better, a resective surgery could have been performed, additionally to the cytoreductive surgery, and administering the hyperthermic intraperitoneal chemotherapy in the same surgical event.
A few experiences with hyperthermic intraperitoneal chemotherapy in other tumors have been achieved, which, in some cases, prolonged survival despite the diffuse disease.
This particular case was in a very advanced stage of the disease. Supported by the findings reported in the necropsy, the tumor was unresectable.
5.4Nuclear and Molecular Medicine ServiceIn the SPECT (Single Photon Emission Computed Tomography) study, a somatostatin analog was intensely positive. From that point, a potential therapeutic option with octreotide could have been proposed and the follow-up with the same study, to check the evolution and response to treatment.
It is important to mention that, in our country, there is a possibility to order PET-CT scan studies with 68Ga-DOTATATE and 68Ga-DOTATOC, which have more sensibility and specificity. At the National Cancer Institute, treatment with the same analogs is administered with 71Lu, apparently with good outcomes.
5.5Oncologic Surgery ServiceAt the moment of the abdominal exploration during the laparotomy, the surgeon can determine if it is possible to perform a surgical procedure, a biopsy or any procedure at all, although this it is not always possible. If an exuberant peritoneal reaction occurs, tissues become inflamed and it can be very difficult to decide whether it is a neoplastic tissue or a peritoneal reaction. The priority is not to injure important structures, provoke perforations or accidents. Finally, the definitive diagnosis is achieved through the histopathological study.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare no conflict of interests.
Please cite this article as: Perezpeña-Diazconti M, Hinojosa AV, Cortés SJ. Adenocarcinoma gástrico con células en anillo de sello y diferenciación neuroendocrina. Un tipo de cáncer poco frecuente en adolescentes. Bol Med Hosp Infant Mex. 2016;73:268–277.