The aim of this study was to determine the incidence of neck bleeding, requiring or not surgical intervention, after carotid endarterectomy (CE) and to identify its predictive parameters and its influence in stroke, myocardial infarction (MI) and mortality.
MethodsThis was a retrospective review of 200 CEs carried out in 194 patients between 2010 and 2014 in our institution. The endpoints were: postoperative major cervical bleeding MB (that required reintervention) and global cervical bleeding GB (registered neck bleeding) as also its major post reintervention complications. Patient demographics, antiplatelet and anticoagulant therapy (pre, intra and postoperative), anesthetic data, surgical technique, and perioperative management data were collected. Univariate analysis with Pearson chi-Squared or Fisher Test was applied for categorical variables and t-test for continuous variables.
ResultsNeck bleeding after CE occurred in 25 cases (12%), requiring reoperation in 8 cases (4.0%). Univariate analysis (Pearson chi-squared test) showed significance (p<0.05) for global hematoma in which concerns clopidogrel use until surgery (p=0.04), elevated mean arterial pressure during hospitalar stay (p=0.006). For major hematoma it has significance previous dual antiplatelet therapy (p=0.039), patch use compared to other techniques (p=0.017), and neurological repercurssion after clamping (p=0.03). Individual analysis of surgical technique did not show significant value for major or global hematoma. There were to 2 deaths, one related to reeintervention, 2 strokes and one MI nonprocedure associated.
ConclusionsCarotid hematoma is a devastating and relatively common complication in our institution although the incidence of major hematoma is reduced. The main factors associated with reeintervention were previous double anti-platelet therapy, non-patch surgical techniques and patient neurological instability (shunt use), probably associated with less accurate hemostasis. Global bleeding is related to the use of clopidogrel 24h before, and as post-operative factors poor tensional control (high)
O objetivo deste estudo consiste na determinação da incidência de hematoma carotídeo após endarterectomia carotídea (EC), identificando os fatores preditivos do mesmo e a sua influência em complicações major, nomeadamente AVC, EAM e mortalidade.
Material e métodosEstudo retrospetivo de 200 EC em 194 doentes, entre 2010-2014, na nossa instituição. Os endpoints primários foram a incidência de hematoma carotídeo major (requerendo intervenção) e hematoma carotídeo global registados e as complicações major pós reintervenção. Foram colhidos os dados demográficos, os dados de antiagregação e hipocoagulação pré, intraoperatórios e pós-operatórios imediato, técnica anestésica e cirúrgica e detalhes da vigilância pós-operatória. Foi efetuada análise univariada com o teste qui-quadrado de Pearson ou Fisher para variáveis categóricas, teste t para contínuas, calculando os odds ratio (OR) para a influência destes fatores relativamente ao grupo sem hematoma.
ResultadosA incidência de hematoma carotídeo registado foi de 25 casos (12%), e de 8 casos (4%) de hematoma major requerendo intervenção. A análise univariada (teste qui-quadrado de Pearson) mostrou significância (p<0,05) para o hematoma global no que diz respeito à utilização de clopidogrel até à cirurgia (p=0,04), pressão arterial média elevada durante a estadia hospitalar (p=0,006). Para o hematoma major é significativo a dupla terapêutica antiagregante (p=0,039), uso de patch em comparação com outras técnicas (p=0,017) e repercussão neurológica após o clampagem (p=0,03). A análise individual das técnicas cirúrgicas não foi significativa para o hematoma major. Ocorreram 2 mortes, uma relacionada à reintervenção, 2 AVC e um EAM não associado à cirurgia.
ConclusõesO hematoma de carotídeo é uma complicação devastadora e relativamente comum na nossa instituição, embora a incidência de hematoma major seja reduzida. Os principais fatores associados à reintervenção foram: terapêutica dupla antiagregante, não uso de patch (técnicas cirúrgicas) e instabilidade neurológica do paciente (uso shunt), provavelmente associado a hemostase menos precisa. A hemorragia global está relacionada com a utilização do clopidogrel 24 horas antes da cirurgia, e como fatores pós-operatórios o fraco controlo tensional (alto).
Carotid hematoma is a well-known complication of vascular surgeon with major consequences in morbidity and mortality depending on the surgeon's quick actuation. The incidence of carotid hematoma in the literature varies between 1.2 and 12%1–8 which reflects both the hematoma requiring intervention and uncomplicated postoperative hemorrhage. Several factors have been identified as predictors of neck bleeding in previous studies.6,9,10 These factors can be arranged in preoperative, intraoperative or postoperative. The first group includes patient morbidity factors, antiplatelet and anticoagulation therapy, creatinine level and platelets. Intraoperative factors refer to the operator, neurological alterations during surgery, shunt use, surgical technique, protamine use, mean arterial pressure. Finally postoperative factors, such as blood pressure control and postoperative coagulation, are also associated with carotid endarterectomy bleeding.
The primary endpoint of this study was to determine, over a period of five years (2010–2014) in 200 CEs, the incidence of complicated hemorrhage (CH) needing reintervention and global hemorrhage (GH) and its association with those previous mentioned factors. A secondary end-point was to determine the incidence of perioperative mortality and morbidity (stroke and MI) hemorrhage related.
Material and methodsThis was a single-center, retrospective, non-randomized, observational study of all CEs performed in our institution, between January 2010 and December 2014. Demographics, intra-operative and perioperative data (until 15 days) were collected from our retrospective database.
DefinitionsComplicated hemorrhage (CH), if surgical exploration was needed after carotid endarterectomy which was inherently associated with the need for intubation.
Global hemorrhage (GH), CH plus uncomplicated neck bleeding defined as hematoma at surgical site without transfusional support, airway obstruction, requirement of reintubation or reoperation and blood drainage <500ml overall.
Mean Arterial Blood Pressure (MABP); parameter evaluated in this study and calculated as: (systolic blood pressure (mmHg)+2×dyastolic blood pressure)/3.
For intraoperative blood pressure, the value is a mean of the 3 highest values, excluding those associated to arterial clamping. For postoperative MABP it's a mean of values calculated during hospital stay.
Preoperative protocolPatients are globally admitted the day before surgery. They underwent preoperative electrocardiogram, bloodcount with platelets, biochemistry including renal function and coagulation study. A vast majority of patients were treated with single antiplatelet therapy (acetylsalicylic acid – ASA 100mg/24h or clopidogrel 75mg/24h). In our institution, most of those patients taking ASA do not stop therapy but clopidogrel is usually stopped 5–7 days before surgery, according to surgeon choice. Hipocoagulation therapy with oral anticoagulants (e.g. Varfine, Sintrom) is always stopped 5–7 days before and replaced by Low Molecular Weight Heparine (LMWH) which is given the night before surgery. Locoregional anesthesia requires a normal coagulation study, if hemostasis is altered, it may be necessary a 10-mg vitamin K dose.
Anesthetic techniqueThe choice of the anesthetic technique is decided by both surgeon and anesthetist, and based also on patient preference, clinical and behavioral expected characteristics. In our hospital most of times locoregional anesthesia is used with exceptions of patient preference, bad collaboration, non-reversible coagulation alterations. Invasive arterial blood pressure by arterial access is always made plus bispectral index control (BIS Vista: Aspect Medical Systems, Inc.) last one during general anesthesia.
Antimicrobial prophylaxis is made with 2-g intravenous (IV) cefazolin and 400mg Teicoplanin or 500mg IV Cyprofloxacin if there is an allergy to beta-lactams.
Surgical technique and perioperative managementThe surgical technique depends mainly on surgeon choice and includes: eversion thromboendarterectomy, patch (venous or synthetic) closure thromboendarterectomy and direct closure, the last one usually required by patient neurological instability.
Systemic heparinization with 5000IU dose of heparin sodium is used, excluding renal dysfunction, with function dependent reduction. There were no reversions with protamine.
If general anesthesia is applied, back flow arterial pressures are measured, when below 40mmHg or a 50% reduction of mean arterial pressure, carotid–carotid shunt is used. In locoregional anesthesia, shunt use is dependent on neurological status alterations monitored before, during and after clamping.
The patches used were very rarely saphenous patches in 2 cases, and Dacron (Dacron patch Hemashield Finesse Ultra-thinPlatinum Knitted Cardiovascular Patch, Maquet Cardiovascular, LLC, Wayne, NJ), or expanded polytetrafluoroethylene – PTFE (Gore Cardiovascular Patch Acuseal, WL Gore & Associates, Inc., Flagstaff, AZ). It was used routinelyin all patients a 14 or 16 French suction drain system connected to a vacuum system, and dismissed 24h after an uncomplicated surgery.
Follow-upClinical follow-up is in Intermedial, Post-Anesthetic or Intensive Unit Care for 12–24h with antiplatelet therapy (ASA) and 40mg SC LMWH are usually given at night. When stopped, clopidogrel is only given 1 week after surgery. In uncomplicated surgeries, patients go home 48h after surgery.
Statistical analysisSPSS for Windows (version 20.0; SPSS Inc., Chicago, IL) was used for statistical analysis. The variables associated with the presence of bleeding and major bleeding were identified by univariate analysis for categorical variables, using the Pearson chi-squared test or Fisher test if 2 cells have expected count less than 5, Student's t-test for continuous data and odds ratio calculation (OR) with 95% confidence intervals (CIs).
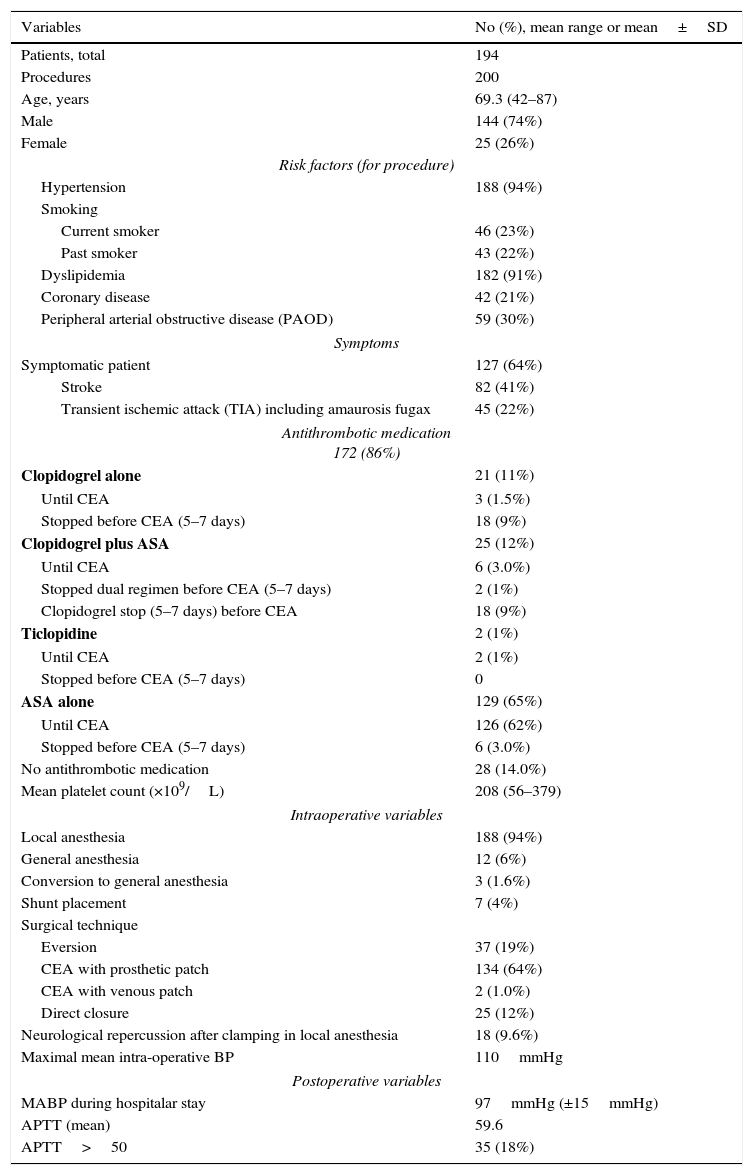
ResultsFrom January 2010 to December 2014, 200 EC were performed in 194 patients and 6 (3%) were bilateral during this period. The average age of the patients was 69.3±8.6 years (range: 42–87 years); 74% were men and 26% women. Patient risk factors are mainly hypertension (94%) and dyslipidemia (91%) and most of them where symptomatic (64%). Most common surgical technique is thromboendarterectomy with synthetic patch closure (64%) under locoregional anesthesia (94%). Demographic, clinical, operative and post-operative data are summarized in Table 1.
Cervical hematomaOverall postoperative cervical hematoma occurred in 25 CEAs of 200 CE (12.5%). Seventeen were treated conservatively, and 8 cases were severe hematomas which required reeintervention. Symptoms associated with the presence of severe hematoma were: cervical edema in 8 (100%), dysfagia 4 (50%), dyspneia 2 (25%). However about half of them had only cervical edema, without other symptoms. Seven in a total of 8 patients were reeinterventionated 24h after CE. Intraoperatively the vast majority 5 (63%) of the cases were diffuse bleedings without an identifiable cause, 1 was a patch associated and 1 a facial venous branch bad ligation.
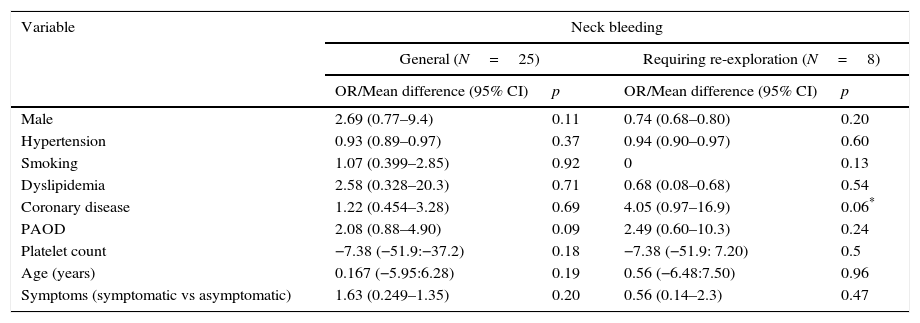
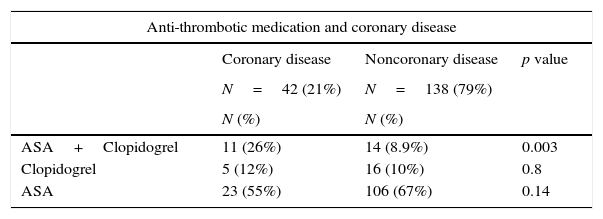
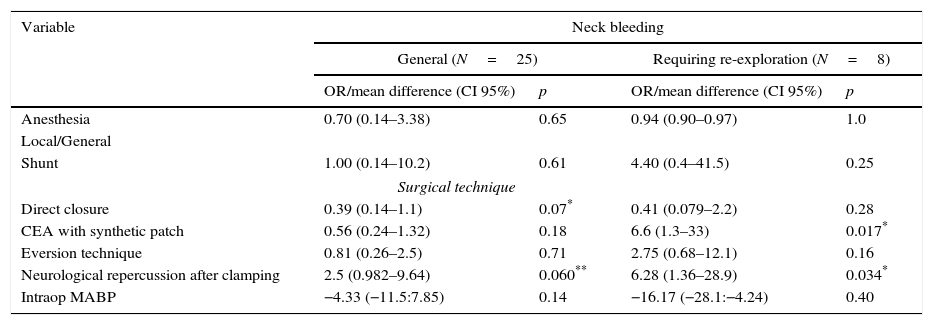
Factors predisposing to bleedingPreoperative factorsIn the univariate analysis (Table 2), none of demographic characteristics of patients were associated with postoperative bleeding, however coronary disease has an almost significant (p=0.06) association with major bleeding. When analyzing and comparing anti-platelet regimens in coronary disease patients they are more often under dual therapy (ASA+clopidogrel), 26% versus 9% with p=0.003, a significant difference which can justify this positive association. No other anti-platelet therapy schemes were significantly associated with bleeding (Tables 3 and 4).
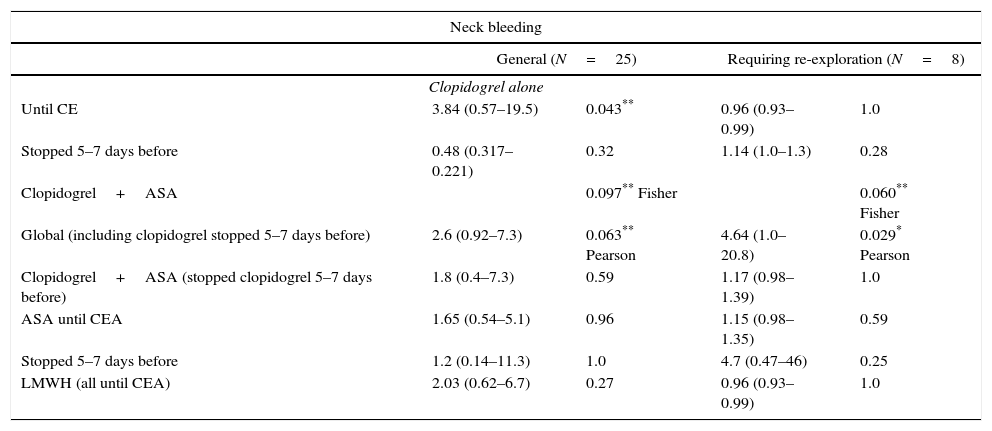
Antiplatelet and anticoagulation therapyFor major bleeding, global dual antiplatelet therapy was significantly associated with reeintervention (p=0.03, Pearson Chi-squared test) and OR=4.6, but no positive association was made if clopidogrel was not stopped before, which only happened in 6 patients (3%). Also in GH, it seems to be a tendency for bleeding with this medical approach as shown by very close significances (p=0.06, Pearson Chi squared test) and OR=2.6. Clopidogrel previous therapy until CE had a significant effect on GH (p=0.04, Fisher test), but when it was stopped no significant neck bleeding was identified. LMWH in previous anticoagulated patients was not associated with bleeding.
Intraoperative factorsIn what concerns surgical technique (Table 5) it was compared each single technique was compared with the others; there were no statistically significant differences for global hematoma. For major hematoma synthetic patch use is associated with less events than the others techniques; only 2 major hematoma in 134 patch technique use (1.5%) and 6 events for the other surgical techniques (66 episodes), 9.1%, p=0.017. This is also true for neurological intraoperative deficit after clamping (p=0.03) and OR=6, more bleeding associated with neurological instability during surgery.
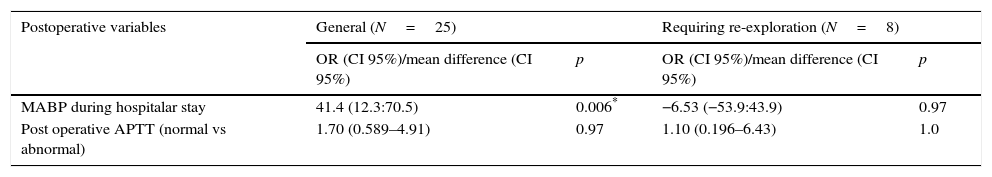
Postoperative factorsIn what concerns patients perioperative follow-up, coagulation study and MABP during hospital stay was studied, Table 3. The only factor that has a significant p value is Blood Pressure and Global Bleeding (p=0.006), patients with poor BP control (high) had more tendency to bleed. Postoperative coagulation study was evaluated using APTT cut-off of 40 (greater than 40 abnormal), but no significant results are associated with postoperative APTT changes.
Influence on major complicationsPerioperative mortality at 30 days was 2/200 (1%) one of them hematoma related, and a total of 2 strokes in non-reeinterventionated patients. There was also one MI non-hematoma associated.
DiscussionThis study showed a global bleeding rate of 12.5%, with major bleeding representing just 4% (8 patients) which required reeintervention. This result is comparable to other published studies in literature 1–12%1,2,6,8,9 and reaches up 25% when less severe bleeding (radiological and clinical criteria) is considered.10 It seems to be reasonable to mention those cases because there is an inevitable operator subjectivity to define indication for intervention, which can affect results.
There is not a Universal criteria for surgical intervention in our institution, so this individual decision is made on an individual basis, however there are some clinical criteria (transfusional support, airway obstruction, requirement of reintubation or reoperation and blood drainage <500ml overall) that indicate a surgical intervention.
Symptoms associated to hematoma were not always straightforward, about 50% of patients had just neck tumefaction, so a high clinical suspicion and sometimes surgeon aggressive attitude was mandatory. It is absolutely crucial to perform an early intubation, to avoid more severe morbidity associated to tracheotomy. Our death was associated with a failed attempt to intubate, and a consequent fatal airway obstruction.
Regarding factors affecting bleeding, as in previous studies,6,9 demographic factors did not show a significant association with bleeding rates, however this study found an almost significant association with coronary disease and major bleeding probably related with dual anti-platelet therapy which was significantly most common in coronary diseased patients.
Anti-platelet treatment associated with major bleeding was ASA+clopidogrel even when stopped 5–7 days before, which suggests a residual effect from this medication as demonstrated in 2001 by Weber in a single cell analysis that shown an irreversible mode of action in humans. Also, for general bleeding, clopidogrel was significantly associated (p=0.04, OR=3.9) with hematoma if it was continued until procedure, similar to other previous published studies.6,9,11–14 Dual antiplatelet therapy was even associated previously with all-cause mortality after carotid revascularization for asymptomatic carotid disease,15 with apparent small benefits in reducing embolic new episodes in symptomatic patients. None of our 8 patients with major bleeding keep clopidogrel so it is not possible to evaluate its action in this group. Low Molecular Weight Heparine (in hipocoagulated patients) did not affect bleeding, probably owing to more rigorous pre and postoperative clinical surveillance.
Intraoperative factors associated with major bleeding where surgical technique, with eversion plus direct closure and venous patch use (2 cases), had a significant p value (0.017) of bleeding comparing to patch use. This is probably justified by surgical technique associated bias (direct closure in neurological instable patients) which leads to a less accurate hemostasis, as shown by significant neurological repercussion after clamping (p=0.03, OR=6.3) in major bleeding. Direct closure was used as a mean of diminishing operative time, in neurological instable patients and alternative to shunt use, according to surgeons’ criteria. However when analyzing independently eversion and direct closure, comparing to the others techniques, p value was not significant for each individual technique.
None of those intraoperative previous factors had a significant impact in global bleeding, however they were close to significance.
Finally, postoperative factors namely high arterial blood pressure, had a very strong effect (p=0.006) in global bleeding, similar to other previous studies9 justifying established anti-hypertensive protocols at the Unit Care.
ConclusionsPostoperative severe bleeding in our institution, although rare, is a considerable complication, comparable to other experienced centers. There is no significant morbidity or mortality associated to reeintervention which suggests an aggressive and immediate actuation. Previous clopidogrel use is associated with major and global bleeding, especially if it is used 24h before surgery. Intraoperative factor as neurological instability is associated with poor hemostasis and consequent major bleeding. Surgical technique like eversion or direct closure are associated with more major hematoma which can be associated with less accurate hemostasis in direct closure (bias), however they do not have significance when individually compared. Postoperative factors such as a high BP are associated with global bleeding.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Patient demographic, clinical, intraoperative and postoperative data.
| Variables | No (%), mean range or mean±SD |
|---|---|
| Patients, total | 194 |
| Procedures | 200 |
| Age, years | 69.3 (42–87) |
| Male | 144 (74%) |
| Female | 25 (26%) |
| Risk factors (for procedure) | |
| Hypertension | 188 (94%) |
| Smoking | |
| Current smoker | 46 (23%) |
| Past smoker | 43 (22%) |
| Dyslipidemia | 182 (91%) |
| Coronary disease | 42 (21%) |
| Peripheral arterial obstructive disease (PAOD) | 59 (30%) |
| Symptoms | |
| Symptomatic patient | 127 (64%) |
| Stroke | 82 (41%) |
| Transient ischemic attack (TIA) including amaurosis fugax | 45 (22%) |
| Antithrombotic medication 172 (86%) | |
| Clopidogrel alone | 21 (11%) |
| Until CEA | 3 (1.5%) |
| Stopped before CEA (5–7 days) | 18 (9%) |
| Clopidogrel plus ASA | 25 (12%) |
| Until CEA | 6 (3.0%) |
| Stopped dual regimen before CEA (5–7 days) | 2 (1%) |
| Clopidogrel stop (5–7 days) before CEA | 18 (9%) |
| Ticlopidine | 2 (1%) |
| Until CEA | 2 (1%) |
| Stopped before CEA (5–7 days) | 0 |
| ASA alone | 129 (65%) |
| Until CEA | 126 (62%) |
| Stopped before CEA (5–7 days) | 6 (3.0%) |
| No antithrombotic medication | 28 (14.0%) |
| Mean platelet count (×109/L) | 208 (56–379) |
| Intraoperative variables | |
| Local anesthesia | 188 (94%) |
| General anesthesia | 12 (6%) |
| Conversion to general anesthesia | 3 (1.6%) |
| Shunt placement | 7 (4%) |
| Surgical technique | |
| Eversion | 37 (19%) |
| CEA with prosthetic patch | 134 (64%) |
| CEA with venous patch | 2 (1.0%) |
| Direct closure | 25 (12%) |
| Neurological repercussion after clamping in local anesthesia | 18 (9.6%) |
| Maximal mean intra-operative BP | 110mmHg |
| Postoperative variables | |
| MABP during hospitalar stay | 97mmHg (±15mmHg) |
| APTT (mean) | 59.6 |
| APTT>50 | 35 (18%) |
Risk of neck bleeding in general and neck bleeding requiring re-exploration related to clinical demographic data (preoperative) – univariate analysis.
| Variable | Neck bleeding | |||
|---|---|---|---|---|
| General (N=25) | Requiring re-exploration (N=8) | |||
| OR/Mean difference (95% CI) | p | OR/Mean difference (95% CI) | p | |
| Male | 2.69 (0.77–9.4) | 0.11 | 0.74 (0.68–0.80) | 0.20 |
| Hypertension | 0.93 (0.89–0.97) | 0.37 | 0.94 (0.90–0.97) | 0.60 |
| Smoking | 1.07 (0.399–2.85) | 0.92 | 0 | 0.13 |
| Dyslipidemia | 2.58 (0.328–20.3) | 0.71 | 0.68 (0.08–0.68) | 0.54 |
| Coronary disease | 1.22 (0.454–3.28) | 0.69 | 4.05 (0.97–16.9) | 0.06* |
| PAOD | 2.08 (0.88–4.90) | 0.09 | 2.49 (0.60–10.3) | 0.24 |
| Platelet count | −7.38 (−51.9:−37.2) | 0.18 | −7.38 (−51.9: 7.20) | 0.5 |
| Age (years) | 0.167 (−5.95:6.28) | 0.19 | 0.56 (−6.48:7.50) | 0.96 |
| Symptoms (symptomatic vs asymptomatic) | 1.63 (0.249–1.35) | 0.20 | 0.56 (0.14–2.3) | 0.47 |
Differences between antithrombotic regimen in coronary and noncoronary patients.
| Anti-thrombotic medication and coronary disease | |||
|---|---|---|---|
| Coronary disease | Noncoronary disease | p value | |
| N=42 (21%) | N=138 (79%) | ||
| N (%) | N (%) | ||
| ASA+Clopidogrel | 11 (26%) | 14 (8.9%) | 0.003 |
| Clopidogrel | 5 (12%) | 16 (10%) | 0.8 |
| ASA | 23 (55%) | 106 (67%) | 0.14 |
Risk of neck bleeding in general and neck bleeding requiring re-exploration related to antithrombotic/hipocoagulation medication – univariate analysis.
| Neck bleeding | ||||
|---|---|---|---|---|
| General (N=25) | Requiring re-exploration (N=8) | |||
| Clopidogrel alone | ||||
| Until CE | 3.84 (0.57–19.5) | 0.043** | 0.96 (0.93–0.99) | 1.0 |
| Stopped 5–7 days before | 0.48 (0.317–0.221) | 0.32 | 1.14 (1.0–1.3) | 0.28 |
| Clopidogrel+ASA | 0.097** Fisher | 0.060** Fisher | ||
| Global (including clopidogrel stopped 5–7 days before) | 2.6 (0.92–7.3) | 0.063** Pearson | 4.64 (1.0–20.8) | 0.029* Pearson |
| Clopidogrel+ASA (stopped clopidogrel 5–7 days before) | 1.8 (0.4–7.3) | 0.59 | 1.17 (0.98–1.39) | 1.0 |
| ASA until CEA | 1.65 (0.54–5.1) | 0.96 | 1.15 (0.98–1.35) | 0.59 |
| Stopped 5–7 days before | 1.2 (0.14–11.3) | 1.0 | 4.7 (0.47–46) | 0.25 |
| LMWH (all until CEA) | 2.03 (0.62–6.7) | 0.27 | 0.96 (0.93–0.99) | 1.0 |
Risk of neck bleeding in general and neck bleeding requiring re-exploration related to intraoperative data – univariate analysis.
| Variable | Neck bleeding | |||
|---|---|---|---|---|
| General (N=25) | Requiring re-exploration (N=8) | |||
| OR/mean difference (CI 95%) | p | OR/mean difference (CI 95%) | p | |
| Anesthesia | 0.70 (0.14–3.38) | 0.65 | 0.94 (0.90–0.97) | 1.0 |
| Local/General | ||||
| Shunt | 1.00 (0.14–10.2) | 0.61 | 4.40 (0.4–41.5) | 0.25 |
| Surgical technique | ||||
| Direct closure | 0.39 (0.14–1.1) | 0.07* | 0.41 (0.079–2.2) | 0.28 |
| CEA with synthetic patch | 0.56 (0.24–1.32) | 0.18 | 6.6 (1.3–33) | 0.017* |
| Eversion technique | 0.81 (0.26–2.5) | 0.71 | 2.75 (0.68–12.1) | 0.16 |
| Neurological repercussion after clamping | 2.5 (0.982–9.64) | 0.060** | 6.28 (1.36–28.9) | 0.034* |
| Intraop MABP | −4.33 (−11.5:7.85) | 0.14 | −16.17 (−28.1:−4.24) | 0.40 |
Intraop: intraoperative.
Risk of neck bleeding in general and neck bleeding requiring re-exploration related to postoperative data – univariate analysis.
| Postoperative variables | General (N=25) | Requiring re-exploration (N=8) | ||
|---|---|---|---|---|
| OR (CI 95%)/mean difference (CI 95%) | p | OR (CI 95%)/mean difference (CI 95%) | p | |
| MABP during hospitalar stay | 41.4 (12.3:70.5) | 0.006* | −6.53 (−53.9:43.9) | 0.97 |
| Post operative APTT (normal vs abnormal) | 1.70 (0.589–4.91) | 0.97 | 1.10 (0.196–6.43) | 1.0 |
Presented in XV meeting (11–13th June, Albufeira, Algarve).