Comparative and descriptive analysis of the outcomes of percutaneous access for EVAR (pEVAR) compared to the control group submitted to surgical femoral access (cEVAR).
MethodsRetrospective case–control analysis between January 2013 and January 2015 of the outcomes of pEVAR (group 1) compared to a control group of cEVAR (group 2) taking into account the demographic data and the primary endpoints: Access complication and surgical time; and secondary endpoints: type of anaesthesia, length of hospital stay and hematic loss. The statistical analysis was performed with the SPSS 23.0 programme using the X2 test for categorical variables and t test for continuous variables.
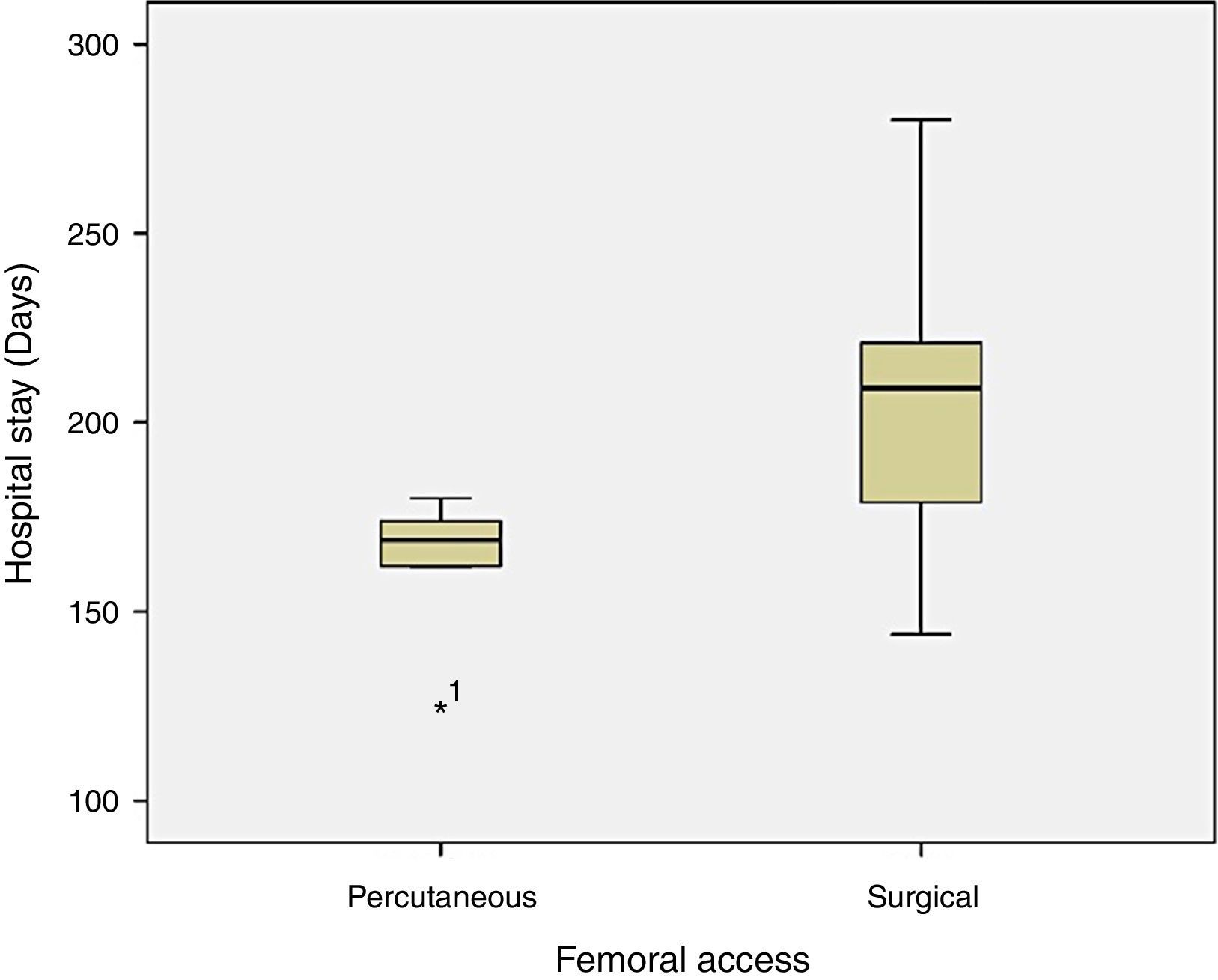
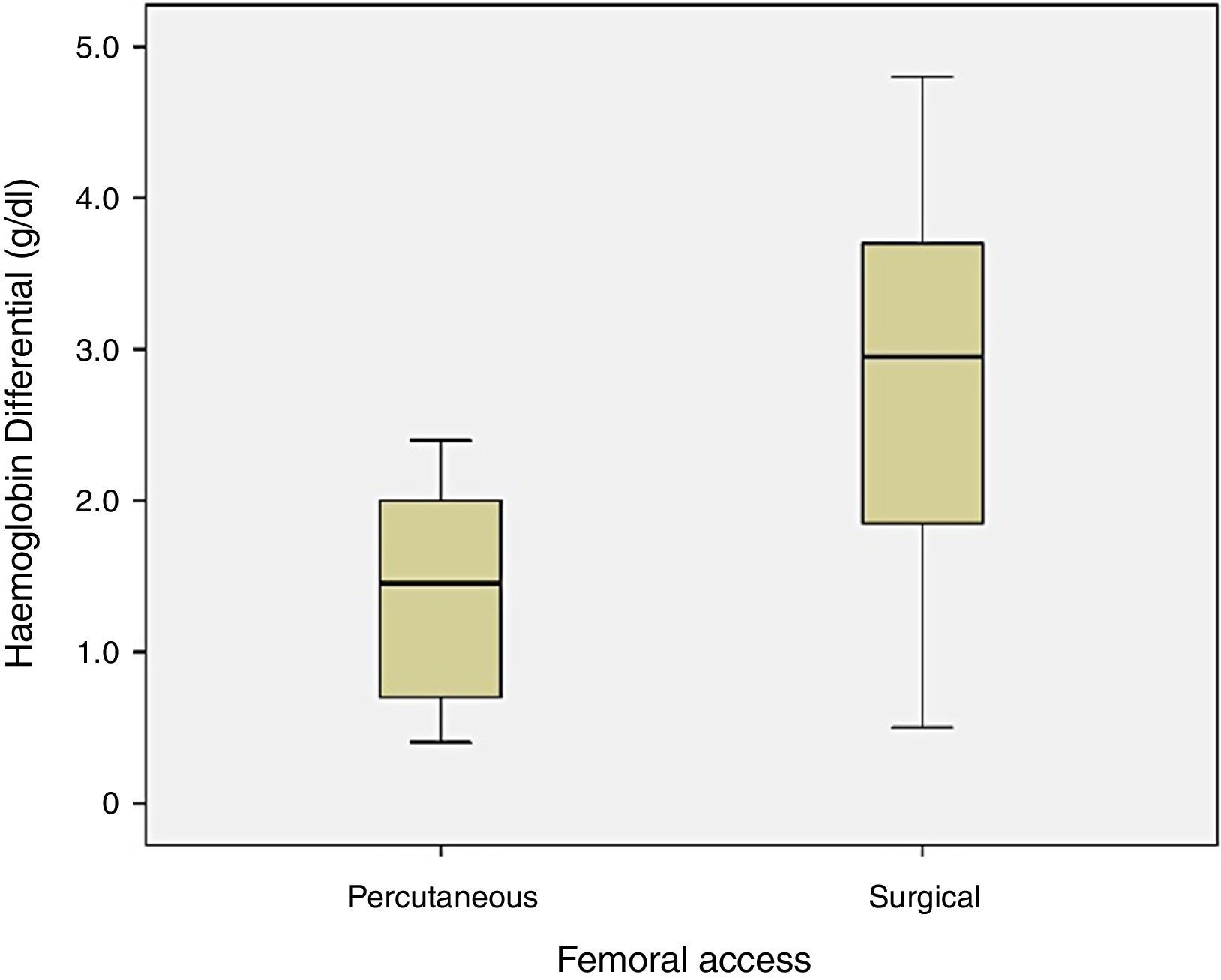
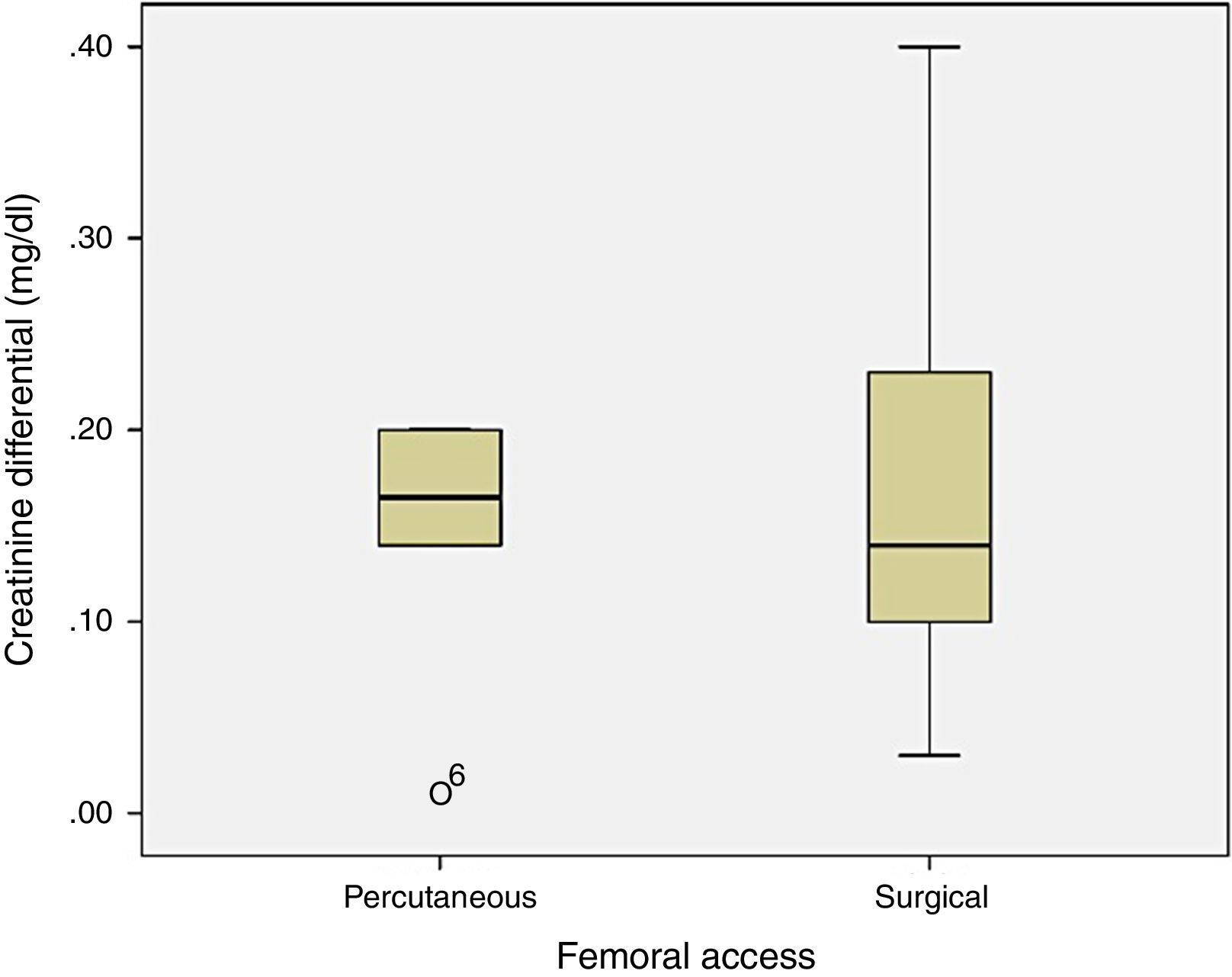
ResultsA total of 6 pEVAR cases were performed in the selected period. A random selection of 20 cEVAR control cases was obtained. The mean age was 75 years, 85% were male. There were no significant differences in comorbidities between the two groups; the most frequent were arterial hypertension, dyslipidaemia, COPD/CID and CRD. There were no differences in major access complications (haemorrhage, lymphatic drainage, pain and oedema), however more frequently in cEVAR, with a significant rate of minor complications such as bruising in pEVAR (3.5% vs. 11.5%, p=0.008). The surgical time was not significantly higher in cEVAR (p=0.21), but the median is greater than in pEVAR with equally high in-group variance (cEVAR vs. pEVAR: 169 vs. 209min; ANOVA: p<0.05). Analysing secondary endpoints, the most widely used anaesthesia was the epidural (p=0.03), hospital stay was higher in cEVAR (6.15 vs. 3.17; p=0.022), a fact not observed in hematic loss (p=0.17) despite the trend towards greater loss in cEVAR (group 1 and 2: 1.4 vs. 2.8mg/dl).
ConclusionPercutaneous access for EVAR demonstrates equal efficacy and safety compared to surgical femoral access, with shorter surgical time and hospitalization and less hematic loss without increasing local complications.
Análise comparativa e descritiva dos resultados do acesso percutâneo para EVAR (pEVAR) e do grupo de controlo submetido a acesso femoral cirúrgico (cEVAR).
MétodosAnálise retrospetiva caso-controlo entre janeiro de 2013 e janeiro de 2015 dos resultados do pEVAR (grupo 1) em comparação com grupo de controlo de cEVAR (grupo 2), tendo como endpoints primários – complicação de acesso e tempo cirúrgico – e os endpoints secundários – tipo de anestesia, tempo de internamento e perda hemática. A análise foi efetuada utilizando o programa SPSS 23.0, com os testes X2 para variáveis categóricas e teste t para variáveis contínuas.
ResultadosForam obtidos 6 casos de pEVAR no período selecionado e realizada uma seleção aleatória de 20 casos-controlo de cEVAR. A idade média foi de 75 anos, sendo 85% do sexo masculino. Não se verificou diferença significativa nas comorbilidades entre os 2 grupos, sendo as mais frequentes a HTA, a dislipidemia, a DPCO/DCI e a IRC. Não se observou diferença significativa nas complicações major de acesso (hemorragia, linforragia, dor e edema), mais frequentes, contudo, no cEVAR, sendo significativa a taxa de complicações minor como equimoses no pEVAR (11,5%, p=0,08). O tempo cirúrgico não foi significativamente superior no cEVAR (p=0,21), contudo a mediana é superior ao pEVAR (pEVAR vs. cEVAR: 169 vs. 209 minutos; ANOVA teste: p<0,05). Quanto aos endpoints secundários, o tipo de anestesia mais utilizado foi a epidural (p=0,03); o tempo de internamento em dias foi superior no cEVAR (6,15 vs. 3,17; p=0,022), facto não observado na perda hemática (p=0,17), apesar da tendência para maior perda no cEVAR (grupo 1 e 2: 1,4 vs. 2,8mg/dl).
ConclusãoO acesso percutâneo para EVAR demonstra igual eficácia e segurança em relação ao acesso femoral cirúrgico, com menor tempo cirúrgico e internamento, sem aumento das complicações locais.
Since first implant by Parodi in 1990, the endovascular repair of abdominal aortic aneurysms (EVAR) has gained acceptance and application in vascular community. Despite recent randomized trials did not demonstrate benefit of EVAR in the first 30 days overall mortality, with increase of reintervention rate,1–3 the total number of procedures has increased globally, with concomitant increase of indications.
It has been observed in recent years a need to reduce aggression in medical, surgical and anaesthetic procedures. As EVAR was traditionally carried out by direct femoral artery catheterization after surgical exposure, there was a recent trend for introduction of percutaneous arterial access, with a theoretical reduction of surgical and anaesthetic aggressiveness.
As demonstrated by recent data as PEVAR Trial,4 the percutaneous implantation of aortic endografts (pEVAR) has been associated with decreased operative time and hospital stay without increasing local complications, being a safe and effective technic. It is also associated with shorter anaesthetic time and aggression, with early onset of normal daily activity and hospital discharge.
This study aims to analyze the experience of a vascular single centre with competence in performing EVAR by both percutaneous (pEVAR) and surgical (cEVAR) access. These procedures were performed by the same set of surgeons, with selected patients compatible to both techniques, with the objective to produce data and evidence in an uncontrolled environment, being the closest possible to the clinical practice.
MethodsRetrospective, single-centre, non-randomized study, conducted in the period between January 2013 and January 2015, in order to compare the results of endovascular treatment of abdominal aortic aneurysms by percutaneous femoral access (pEVAR – group 1) with the results the surgical femoral access (cEVAR – Group 2). The percutaneous access included in all patients a pre-assembly of bilateral femoral closure devices (Proglide® – Abbott®).
The inclusion criteria were: (a) pEVAR in an infrarenal aortic aneurysm with a bifurcated stent graft (group 1); (b) cEVAR in an infrarenal aortic aneurysm with a bifurcated stent graft (group 2); (c) elective procedures; (d) asymptomatic patients; (e) fusiform or saccular aneurysms, with favourable anatomy.
The exclusion criteria were: (a) thoracic, thoracoabdominal, pararenal or juxtarenal aneurysm; (b) symptomatic or ruptured aneurysm; (c) complex aortic, iliac or femoral anatomy; (d) complex endovascular or hybrid procedure; (e) femoral circumference calcification >50% identified by arterial Doppler ultrasound; (f) extensive inguinal scar, previous femoral complication or intervention; (g) coagulation disorders.
There was no preference of bifurcated aortic endografts. Three types of endorafts were used: Zenith®, Excluder® and Endurant®.
Were defined as primary endpoints: (a) complication in the femoral access; (b) surgical time. In access complication, four main points were analyzed: (a) major bleeding, defined as identified hematic loss requiring blood transfusion; (b) minor bleeding as a bruise or haematoma without the need for transfusion support; (c) lymphatic drainage at the site of percutaneous or surgical femoral access; (d) inguinal pain; (e) lower limb oedema, unilateral or bilateral.
As secondary endpoints were selected: (a) type of anaesthesia; (b) length of hospital stay; (c) hematic loss; (b) renal function. Hematic loss is defined as haemoglobin value differential collected by peripheral venous puncture before and after surgery. Renal function was assessed by analytical value of serum creatinine before and after surgery (minimum interval of 24h).
The access choice was based on personal experience of a surgeon capable of independent use of the two techniques, after guaranteed the exclusion criteria. All percutaneous accesses were ultrasound guided and at least one loading dose of 5000 units of unfractionated heparin was administrated at the beginning of the procedure.
Statistical analysisStatistical analysis was performed using the SPSS 23.0 programme with descriptive evaluation of demographic data, and applying the χ2 tests for the analysis of categorical variables and the t test for continuous variables.
ResultsA total of 6 patients submitted to pEVAR (group 1) were identified in the described period. Of the patients submitted to cEVAR (group 2) in this same interval, a random selection of 20 patients was selected and defined as the control group.
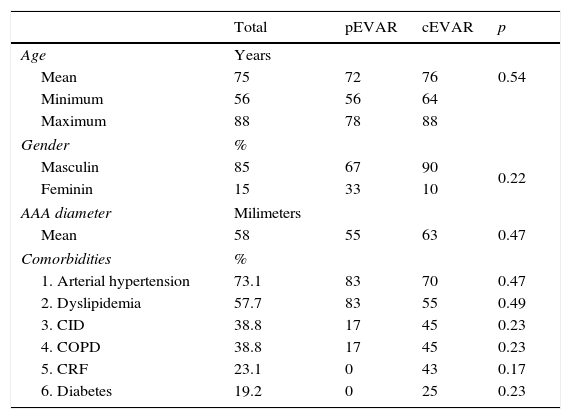
The average age of both groups was 75±8 years (min: 56; max: 88 years) with a mean age of 72 years for group 1 and 76 years for group 2. Twenty-two patients (85%) were male. The average diameter of the aneurysm was 58mm (Table 1).
Demographic factors, aneurymal characteristics and comorbidities.
| Total | pEVAR | cEVAR | p | |
|---|---|---|---|---|
| Age | Years | |||
| Mean | 75 | 72 | 76 | 0.54 |
| Minimum | 56 | 56 | 64 | |
| Maximum | 88 | 78 | 88 | |
| Gender | % | |||
| Masculin | 85 | 67 | 90 | 0.22 |
| Feminin | 15 | 33 | 10 | |
| AAA diameter | Milimeters | |||
| Mean | 58 | 55 | 63 | 0.47 |
| Comorbidities | % | |||
| 1. Arterial hypertension | 73.1 | 83 | 70 | 0.47 |
| 2. Dyslipidemia | 57.7 | 83 | 55 | 0.49 |
| 3. CID | 38.8 | 17 | 45 | 0.23 |
| 4. COPD | 38.8 | 17 | 45 | 0.23 |
| 5. CRF | 23.1 | 0 | 43 | 0.17 |
| 6. Diabetes | 19.2 | 0 | 25 | 0.23 |
AAA, abdominal aortic aneurysm; CID, coronary ischaemic disease; COPD, chronic obstructive pulmonary diseade; CRF, chronic renal failure.
The most common co-morbidities were arterial hypertension (73%), dyslipidemia (58%), coronary ischaemic disease (39%), chronic obstructive pulmonary disease (39%), chronic renal failure (23%) and type 2 diabetes (19%).
Comparing the two groups, there were no significant differences between each comorbidities (p>0.05), registering however more prevalence in group 2 of coronary ischaemic disease (45%), chronic obstructive pulmonary disease (45%) and chronic renal failure (43%) (Table 1).
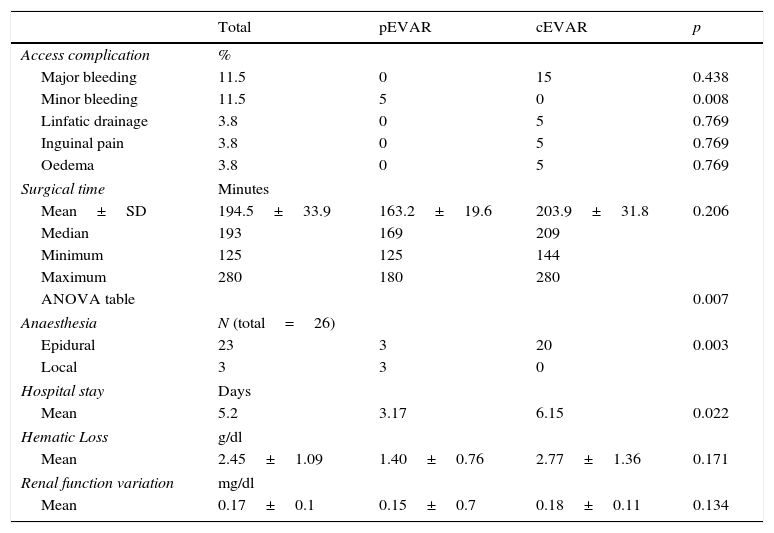
Primary endpointsThe overall major bleeding rate was 11.5%, not obtaining however statistical significance between the two groups (p=0.438), unlike minor bleeding, higher in-group 1 (11.5%, p=0.008). Lymphatic drainage, inguinal pain and lower limb oedema, all with an overall incidence rate of 3.8%, although higher in group 1, achieved no significant difference between groups (p=0.769) (Table 2).
Results of primary and secondary endpoints.
| Total | pEVAR | cEVAR | p | |
|---|---|---|---|---|
| Access complication | % | |||
| Major bleeding | 11.5 | 0 | 15 | 0.438 |
| Minor bleeding | 11.5 | 5 | 0 | 0.008 |
| Linfatic drainage | 3.8 | 0 | 5 | 0.769 |
| Inguinal pain | 3.8 | 0 | 5 | 0.769 |
| Oedema | 3.8 | 0 | 5 | 0.769 |
| Surgical time | Minutes | |||
| Mean±SD | 194.5±33.9 | 163.2±19.6 | 203.9±31.8 | 0.206 |
| Median | 193 | 169 | 209 | |
| Minimum | 125 | 125 | 144 | |
| Maximum | 280 | 180 | 280 | |
| ANOVA table | 0.007 | |||
| Anaesthesia | N (total=26) | |||
| Epidural | 23 | 3 | 20 | 0.003 |
| Local | 3 | 3 | 0 | |
| Hospital stay | Days | |||
| Mean | 5.2 | 3.17 | 6.15 | 0.022 |
| Hematic Loss | g/dl | |||
| Mean | 2.45±1.09 | 1.40±0.76 | 2.77±1.36 | 0.171 |
| Renal function variation | mg/dl | |||
| Mean | 0.17±0.1 | 0.15±0.7 | 0.18±0.11 | 0.134 |
SD, standard deviation.
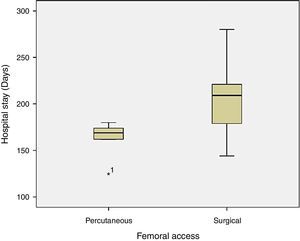
The mean operative time was 194.5±34min. The mean in-group 1 was 163.2±19.6min (min: 125; max: 180) and group 2 reached 203.9±31.8min (min: 144; max: 280). The analysis does not showed differences between groups (p=0.206). Observing the higher range of surgical time in group 2 (144 to 280min) evidenced in the analysis of clustered bar chart (Fig. 1), we proceeded to the analysis of intra-group variance with ANOVA table which revealed significant difference of the surgical times between the two groups (p=0.007), being higher in group 2 (Table 2).
Secondary endpointsThe most common type of anaesthesia was the epidural (n=20) with statistical significance in relation to the local anaesthesia (p=0.003). This was the technique of choice in every patient of group 2 and three patients in group 1, the remainder being subject to local anaesthesia. None of the patients underwent the procedure under general anaesthesia (Table 2).
The average length of hospital stay was 5.2±1.9 days with 3.17 days in group 1 and 6.15 days in group 2, reaching significant difference between the two groups (p=0.022).
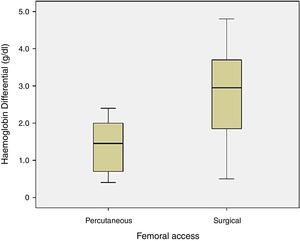
The haemoglobin differential before and after surgery was not significant between the two groups (p=0.171), with hematic loss of 1.4±0.8g/dl in group 1 and 2.8±1.4g/dl in group 2 (Fig. 2).
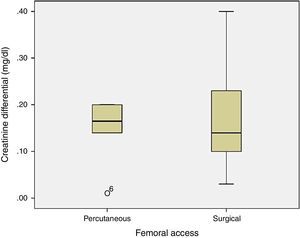
Renal function was not significantly different between the two groups (p=0.134), with 0.15±0.07mg/dl difference in plasma creatinine in group 1 and 0.1±0.18mg/dl in group 2 (Fig. 3).
DiscussionAlthough recent studies such as EVAR trial1 or the Cochrane review by Paravastu et al. in 20142 not demonstrate benefit in the medium and long-term results of endovascular treatment of aortic aneurysms compared to surgical approach, technological and scientific expansion with application in ruptured, young patients or complicated and complex aneurysms provided an enlargment and affirmation of EVAR as first-line therapy for infra-renal aortic aneurysms.
It has also been observed in recent years a progressive and supportive minimal invasive approach to medical and global surgical intervention. In this appreciation, for nearly 10 years that percutaneous access for EVAR has gained more supporters with some centres currently holding more than 90% of procedures using this technique with success rates close to 100%.4–9
The scientific evidence demonstrated by the PEVAR trial4 in 2014 or more recently by Buck et al. 5 with analysis of over 1000 patients undergoing pEVAR, show excellent results of this technique in relation to surgical femoral approach with high success rate, shorter operative time and hospitalization, and lower complication rate.
This study aims to analyze the results of pEVAR in a vascular department that performs both techniques by the same set of professionals. The analysis is compared with the results of the group submitted cEVAR, and the decision on the type of access per patient was made based on preference and experience of the professional, obtaining an review independent of randomization, being the closest possible to daily clinical practice.
All the patients analyzed had clinical and anatomical characteristics compatible with both techniques. There were no significant differences in all comorbidities in both groups; however, the surgical approach group had higher prevalence of coronary ischaemic disease group and chronic kidney failure as well as lung disease.
In primary endpoints analysis, the most frequent access complication rate was bleeding, reaching 11.5%, not significantly different between the two groups (bleeding requiring transfusion support). Nevertheless, minor bleeding without need for intervention reaches statistical significance, higher in pEVAR. This is probably related to the initial service experience in the use of percutaneous closure devices. This fact has recently been demonstrated by Bechara et al. where the closing failure rate decreased from 45% to 5% with increasing operator experience, being this one of the main factors associated with the treatment success.10–12 This success rate also relates with use of ultrasound to percutaneous puncture,13 a technique that since 2007 is positively related to the reduction of local complications. Another interesting fact is that the use of therapeutic intraoperative levels of heparin was not associated with increased bleeding rate, even if not performing reversal at the end of the intervention.14,15
The remaining access complications such as lymphatic drainage, inguinal pain at the site of access or leg oedema did not obtain significant differences between the groups, despite being expecting an increase in cEVAR, with overall rate of 3.8%, in line with current evidence, that ranges from 2.9% to 10.1%.16,17
In this study we considered three types of bifurcated endograft most used in our country, with sheath diameter ranging between 14F and 18F. Despite the described increased rate of access complications using sheath diameters higher than 20F, obesity and femoral calcification,11,18 there is no scientific evidence to support deleting the percutaneous access from these patients. As described by several authors,19–22 percutaneous access can be safely performed in obese patients with calcified femoral arteries using sheaths up to 24F. These results apparently persist in the long-term follow-up, with late complication rate around 2% at twelve months.23
Analysing the surgical time for intervention, with an average of 195min globally, there was no expected significant differences between the two groups. However, besides the difference between the two means (pEVAR vs. cEVAR: 163 vs. 204min), a wide range of values in-group 2 raised the possibility of having high intra-group variance of values that would associate the lack of significance. The bar cluster graph showed higher surgical time tendency in group 2. The analysis of the ANOVA table proves the hypothesis, since the intra-group variance was statistically significant (p<0.05). It is thus understood that the tendency for sustained reduction of surgical time with the pEVAR was not statistically supported by the lower sample homogeneity of the cEVAR group.
The analysis of the secondary endpoints shows that although most patients have been undergoing epidural anaesthesia (77%), there is a tendency for local anaesthesia with pEVAR, representing 50% of the patients in this study, steadily increasing in time. This factor is also associated with a decreased surgical time,24 as well as the postoperative recovery and hospital discharge.
The length of hospital stay was significantly lower in patients in-group 1, with a mean difference of around 3 days. This factor is apparently related to the type of anaesthesia and decrease in access complications. Despite there was no significant difference in the later, those complications were 5% lower in the percutaneous access.
Despite having not been a subject of this study, this data creates an assumption that percutaneous access may decrease total costs, not balanced by the cost of percutaneous closure devices. This hypothesis was demonstrated by Jean-Baptiste et al.25 in 2008 where the difference in length of hospital stay was related to the decrease in total costs in patients undergoing pEVAR. This cost can be even lower if one considers the ambulatory hypothesis of percutaneous procedure in patients with good functional capacity and low medical risk, without complication during the procedure.26
Analysing the hematic loss and change in renal function between the two groups, there was no significant differences. However, the difference in hematic loss between groups reaches 1.3g/dl, with a greater loss tendency for patients undergoing surgical access, fact evidenced by the analysis of the clustered bar graph. That difference was not observed in renal function variation, with close serum creatinine values before and after procedure.
This study presents some limitations as the small number of selected patients, which is related to the recent initiation of the percutaneous technic in EVAR, despite the pre-existing experience in other percutaneous arterial treatments (occlusive disease for example), a number that will significantly increase in the forthcoming months.
Another limitation is related to the non-randomization of patient. There is thus a natural selection bias, which may alter the results. However, not excluding the logical statistical limitations, the option allowed to have a close approach of the results of the reality of clinical practice.
ConclusionDespite the limited experience, the pEVAR presents itself as a safe and effective option compared to cEVAR, with lower local complications rate, decreased surgical time and hospitalization. It is still required a sample increase and medium and long term outcomes to confirm the percutaneous access as first-line option in patients undergoing endovascular repair of abdominal aortic aneurysms.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestNo conflicts of interest to declare.