Allergic rhinitis (AR) is a classic Th2-mediated disease, with important contributions to the pathology of interleukins 4, 5, and 13. The co-stimulatory molecule of OX40 and its ligand interaction participate in the immune response by regulation of Th1/Th2 cells balance. Considering the paucity of information on the relation between OX40 ligand (OX40L) and AR, this study aimed to examine its expression on B lymphocytes.
Patients and methodsThis case–control study consisted of 20 AR patients and 20 healthy subjects. The serum level of total immunoglobulin E (IgE) was measured using the electro-chemiluminescence (ECL) technology. The percentage of B-lymphocytes expressing OX40L was assessed by flow cytometry. The amounts of IL-4 in CD4+ T cells culture supernatant was also measured by the enzyme-linked immunosorbent assay (ELISA).
ResultsOX40L expression on B lymphocytes of patients was significantly higher than the control group (44.32±19.21% vs. 2.79±2.48% respectively, p<0.001). In AR patients, OX40L expression correlated positively with the levels of serum total IgE and IL-4 produced by CD4+ T lymphocytes (p<0.01 – p<0.05) respectively.
ConclusionsCollectively, the findings of this work suggest that there is a relationship between the OX40L expression level on B lymphocytes and allergic markers such as IgE and IL-4 in patients with allergic rhinitis.
Allergic rhinitis (AR) is a chronic inflammation of the upper respiratory tract with certain symptoms and signs in sensitive individuals exposed to certain allergens. In spite of advances in immunology, AR is a significant problem for people's health: it appears in 30% of all adults and 40% of all children. Furthermore, AR is a symptomatic immune-related disorder created through Immunoglobulin E (lgE) related allergic responses to allergens. Its major symptoms consist of rhinorrhea, nasal congestion, nasal pruritus, and sneezing.1,2 The prevalence of this disease is increasing and imposing higher economic burdens on society. Besides, whether seasonal or annual, AR significantly increases the risk of asthma: more than 40% of people with allergic rhinitis are or will be asthmatic.3,4
Generally, the process of sensitization in people with rhinitis involves the uptake of the allergen by the antigen-presenting cells (APCs) in the nasal mucosa, which causes the activation of allergen-specific T cells. Simultaneously, the activity of epithelial cells through non-antigenic pathways (such as proteases) leads to the release of epithelial cytokines, such as thymic stromal lymphopoietin (TSLP), interleukin (IL) -25, IL-33, and eventually directs cellular response toward T-helper (Th) 2 cells. This altered direction of immune responses causes dendritic cells and type 2 innate lymphoid cells (ILC-2) along with basophils, to generate cytokines such as IL-4 and IL-13. This leads to production of Th2 lymphocytes and the conversion of B lymphocytes to allergen-specific IgE-producing plasma cells.5
Allergic diseases are associated with the balance shift of Th1/Th2 toward overcoming Th2.6 OX40 is a type-1 transmembrane glycoprotein that belongs to the tumor-necrosis factor (TNF) receptor family. Once T lymphocytes are activated through T-cell receptor antigen (TCR), this co-stimulatory receptor is expressed on these cells, which is required for their proliferation and survival. It seems that the OX40 receptor exists permanently on regulatory T lymphocytes. OX40 ligand (OX40L) is expressed on dendritic cells, macrophages, activated B lymphocytes, and other cells, including mast cells and endothelial cells.7,8 Researchers have also found that functional OX40L can also be induced on the activated CD4+ T and CD8+ T cells, whose expression increases due to transforming growth factor- beta-1 (TGFβ-1).9 The OX40 receptor engagement in naive CD4+ T lymphocytes may lead to preferably the production of Th2 cells, which seems to be the result of IL-4 production and the activation of nuclear factor of activated T-cells (NFAT) transcription factor. However, production of IL-12 or IFN-γ can lead to responses in Th1 cells.10 On the other hand, studies indicate that OX40 signaling inhibit IL-10 production and function of Treg lymphocytes.11 Generally, the interaction between OX40 and OX40L can be effective in cytokines production and thereby be effective with reference to T lymphocytes participating in immune responses through the balance of Th1/Th2 cells. OX40/OX40L interactions play an important role in the development of some inflammatory, infectious, allergic, and autoimmune diseases, making these interactions and their mechanism of action a remarkable candidate for clinical interventions.7,10
Considering the limited information available concerning the relation between OX40L and AR, this study aimed to examine the OX40L expression on the surface of peripheral blood B lymphocytes as antigen presenting cells in AR patients compared to the healthy subjects. Moreover, the values of serum total IgE and IL-4 produced by CD4+ T cells were measured in two groups. Lastly, the relation between OX40L expression on B cells and serum IgE levels as well as the amounts of IL-4 produced by CD4+ T cells was studied in two groups.
Subjects and methodsSubjectsPatientsThis case–control study consisted of 20 patients with allergic rhinitis who referred to an asthma and allergy super specialist from April 2016 to November 2016: all were diagnosed with allergic rhinitis. Patients were 18–50 years old; they comprised eight males and 12 females.
The inclusion criteria were diagnosing allergic rhinitis based on clinical examinations and disease history, specific signs and symptoms of allergic rhinitis, positive prick test, and absence of non-allergic diseases of nasopharynx and other organs.
The exclusion criteria were chronic rhinosinusitis, nasal polyps, and non-allergic rhinitis (infective), smoking, presence of other allergic diseases, existence of systemic diseases affecting the level of cytokines, consumption of steroids from six weeks before the blood test, and antihistamine consumption one week before sampling.
Healthy subjects (control group)Inclusion criteria including 20 healthy subjects who matched with patients in terms of age and gender and had no allergic signs, symptoms, or history of allergic diseases. The study protocol was confirmed by the Ethics Committee of Isfahan University of Medical Sciences. Written informed consent was taken from all subjects before taking the sample.
MethodsMeasurement of the serum level of total IgEThree milliliters of whole blood was taken from the two groups. It was centrifuged, whereupon serum was separated after clotting and kept at 4°C. The serum level of total IgE was measured using the electro-chemiluminescence (ECL) technology (Roche Diagnostics, Mannheim, Germany). Related concentrations were measured according to protocols using an immunoassay analyzer. The analytical sensitivity was 0.1IU/ml. Normal range was considered less than 100IU/ml.
Preparation of the peripheral blood mononuclear cells (PBMCs)Peripheral blood was obtained from the patients and healthy controls (20ml of ethylenediaminetetraacetic acid, EDTA containing blood). The peripheral blood mononuclear cells (PBMCs) were separated by using Ficoll density gradient centrifugation (Sigma, USA). The viability of the cells was examined using trypan blue dye exclusion method, in which a viability of over 95 percent was considered acceptable for further investigation.
OX40L expression on B lymphocytesThe PBMCs from each group were used in flow cytometric analysis (1×106). Before staining, cells were pre-incubated for 10min with 5μl blocking buffer (Biolegend, USA) per 100μl cell suspension so as to decrease the non-specific binding. This buffer contained specialized human IgG in PBS containing 0.09% sodium azide. Two tubes were used in each case: one as a test tube for cell staining with phycoerythrin (PE)-labeled anti-human OX40L and fluorescein isothiocyanate (FITC)-labeled anti-human CD19 antibodies; the other for PE and FITC isotype controls as control (Biolegend, San Diego, CA, USA). Then antibodies were added to cell suspensions and tubes were incubated at room temperature for 20min. The tubes were centrifuged at 1500rpm, at 4°C for 5min and were washed twice with phosphate-buffered saline (PBS). Lymphocytes were isolated based on gate, side scatter, and forward scatter. Thereafter, CD19+ B lymphocytes were isolated from lymphocytes’ gate. Finally, OX40L expression level was determined on B lymphocytes’ surface by a FACSCalibur flow cytometer (Becton Dickinson Biosciences, San Jose, CA, USA). The data were also analyzed by the FlowJo 7.6 software (FlowJo, USA).
Isolation of the peripheral blood CD4+ T lymphocytesAfter preparation of the PBMCs, the CD4+ T lymphocytes were separated using the magnetic beads and MACS® columns (Miltenyi Biotec GmbH, Germany) based on the negative selection, according to the instructions of the kit. The cells were thereafter stained with FITC-labeled anti-human CD4+ and PE-labeled anti-human CD3 antibodies (Biolegend, San Diego, CA, USA) and then examined by the flow cytometry method; finally, their purity was determined as over 90 percent.
Measurement of IL-4 level in the cellular cultivation supernatantThe isolated peripheral blood CD4+ T lymphocytes were cultured in the RPMI-1640 medium (Bioidea, Tehran, Iran), which contained 10% fetal bovine serum and 1% penicillin–streptomycin (Bioidea, Iran) under standard culture conditions (37°C; humid air (95%) and CO2 (5%)) for 72h. The supernatant was collected by centrifuging the samples at 1200g at 4°C for 5min. The centrifuged supernatant was then immediately preserved at −20°C to be used for measurement of IL-4 level. The concentration of IL-4 was measured by the enzyme-linked immunosorbent assay (ELISA) according to the kit protocol (Biolegend, San Diego, CA, USA). The minimal detection level of IL-4 was 2.4pg/ml.
Statistical analysisData analysis was conducted using IBM SPSS 21 Statistics (IBM, USA). Values are represented as mean±standard deviation (SD). Student's t-test was used to compare the quantitative variables of two groups. Chi-squared test was used to compare the qualitative variables. Pearson's correlation coefficient test was used to assess the strength of correlation between the OX40L and other variables. Significance level was considered as p<0.05.
ResultsThis study consisted of 20 AR patients (mean age=35.15±9.76 years old) with allergic rhinitis and 20 healthy subjects (mean age=36.2±8.39 years old) as controls group (eight males and 12 females in each group).
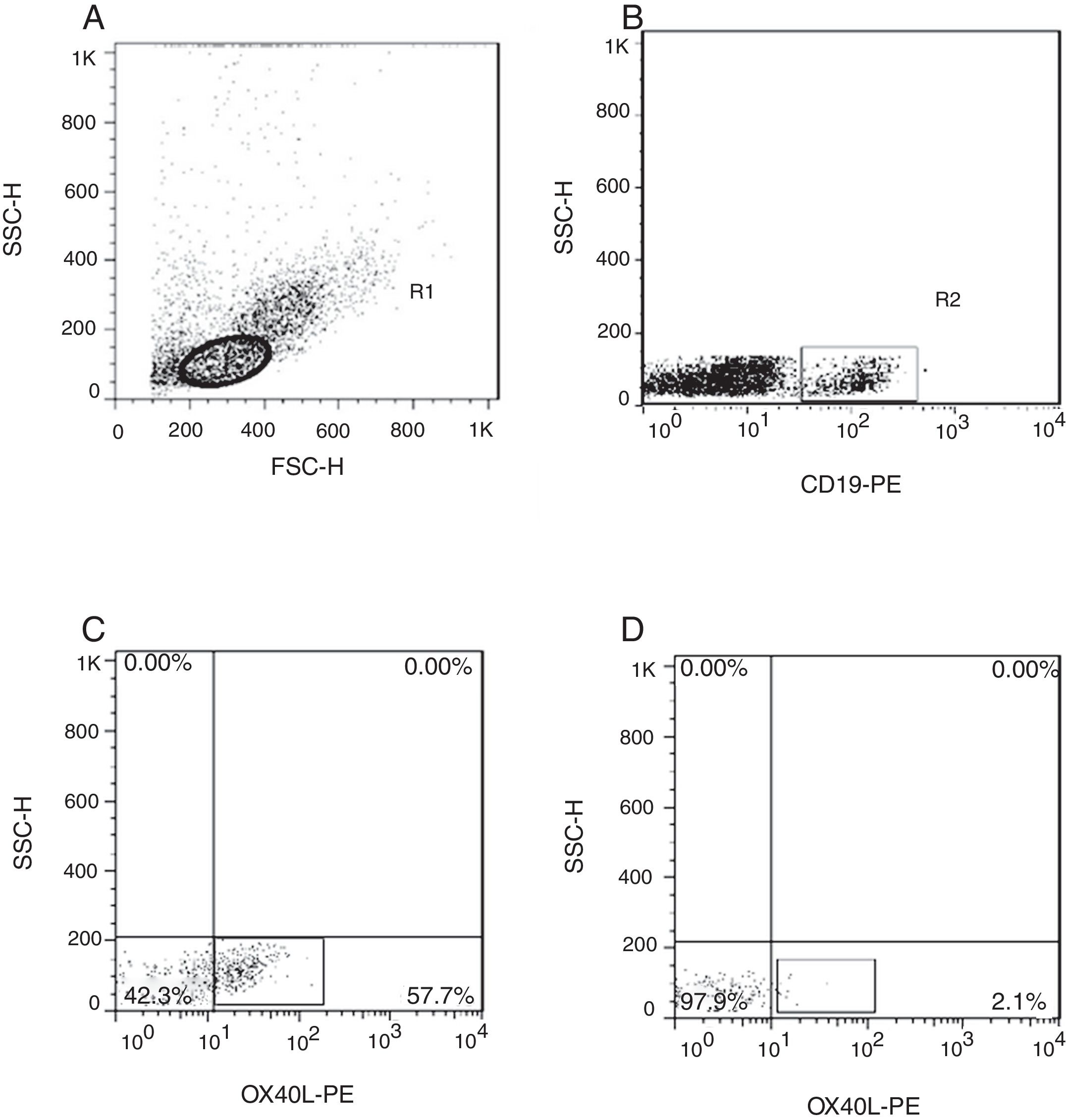
Evaluation of the expression levels of OX40L on B lymphocytesThis study evaluated OX40L on the surface of the peripheral blood B lymphocytes in two groups. Results showed that expression of OX40L was significantly different in the patients compared to the controls (44.32±19.21% vs. 2.79±2.48% respectively, p<0.001). Fig. 1 shows an example of the flow cytometric results of measuring the expression level of OX40L in the experimental and control groups.
Gating strategy and representative flow cytometric dot plots. (A) Initially, cells were gated in Region 1 on the basis of forward scatter (FSC) and side scatter (SSC), to gate lymphocytes. (B) Then these cells were selected for further analysis for CD19 and (C) OX40L expression (%) in CD19+ B cells of patients with allergic rhinitis and (D) healthy controls. OX40L, OX40 ligand.
Firstly, lymphocytes were gated out on the basis of forward scatter (size) and side scatter (complexity). Then, these cells were further analyzed for the expression of CD19 and OX40L (%) in CD19+ B cells of AR patients and controls.
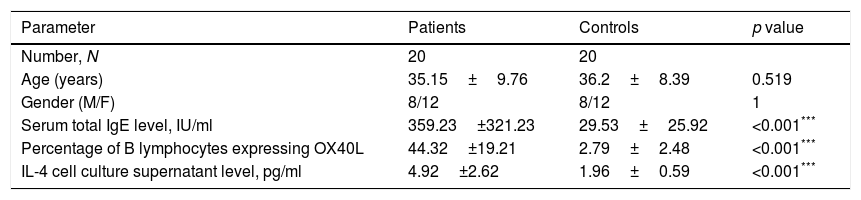
Measurement of the serum levels of IgE and IL-4 in the cell culture supernatantTo confirm the correlation of OX40L expression on B cells, the amounts of serum IgE and IL-4 produced by CD4+ T cells were measured in the patients and controls. The results showed that the IgE (359.23±321.23IU/ml vs. 29.53±25.92IU/ml) and IL-4 (4.92±2.62pg/ml vs. 1.96±0.59pg/ml) values respectively. These differences were significant (p<0.001, p<0.001). Characteristics of the two groups and values of the measured variables are summarized in Table 1.
Characteristics of the study groups.
| Parameter | Patients | Controls | p value |
|---|---|---|---|
| Number, N | 20 | 20 | |
| Age (years) | 35.15±9.76 | 36.2±8.39 | 0.519 |
| Gender (M/F) | 8/12 | 8/12 | 1 |
| Serum total IgE level, IU/ml | 359.23±321.23 | 29.53±25.92 | <0.001*** |
| Percentage of B lymphocytes expressing OX40L | 44.32±19.21 | 2.79±2.48 | <0.001*** |
| IL-4 cell culture supernatant level, pg/ml | 4.92±2.62 | 1.96±0.59 | <0.001*** |
IgE, immunoglobulin E; OX40L, OX40 ligand; IL-4, interleukin-4. Data are expressed as mean±standard deviation (SD).
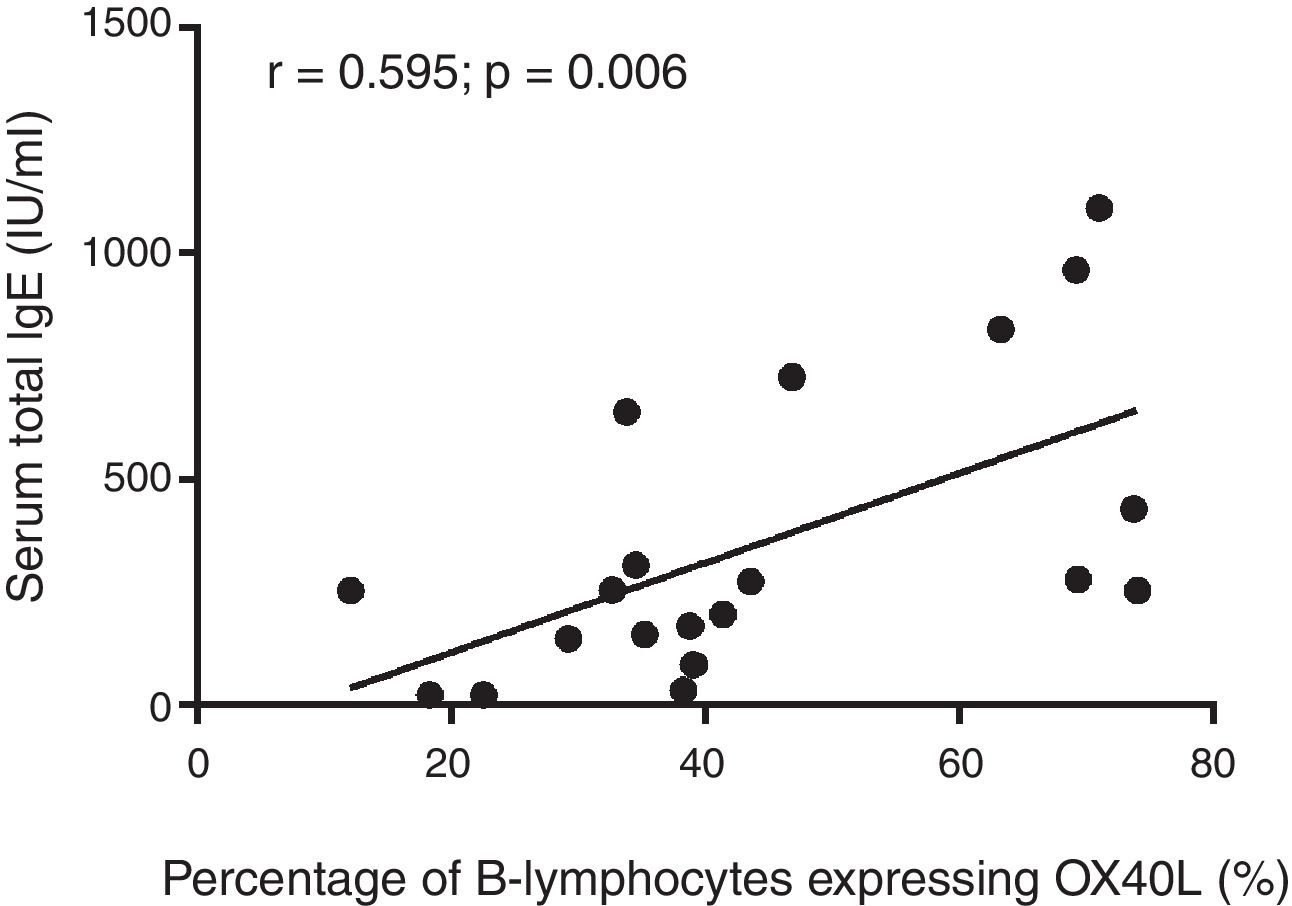
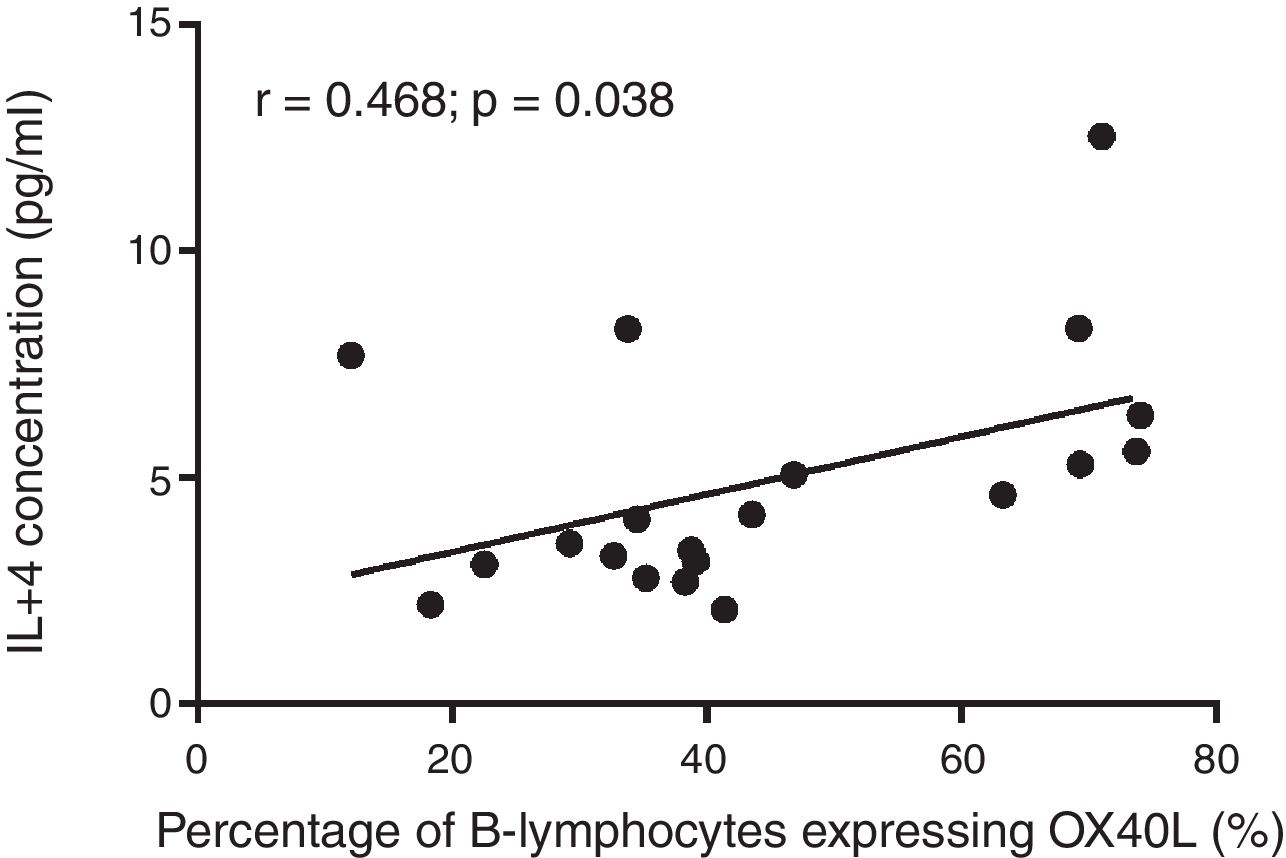
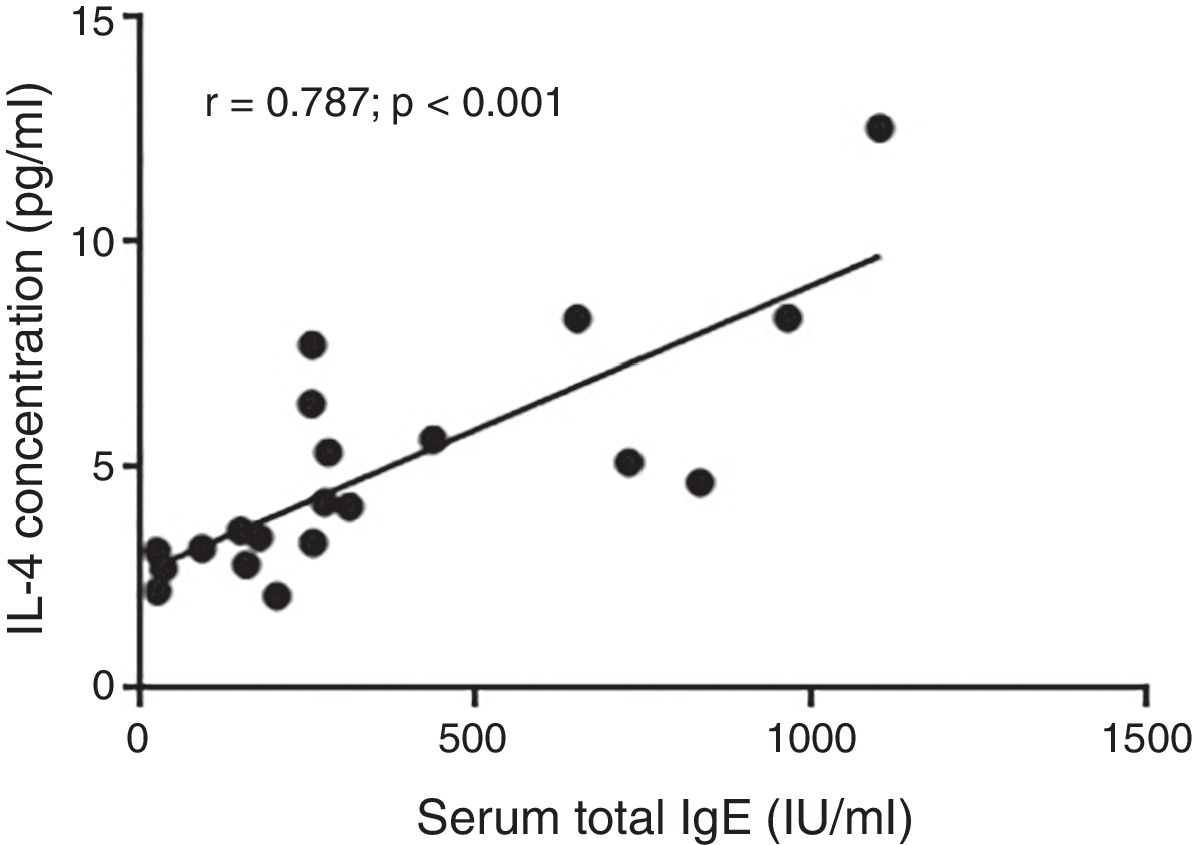
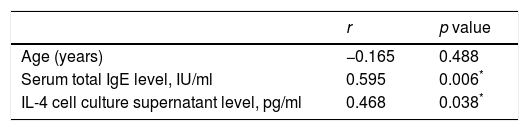
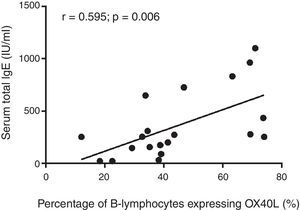
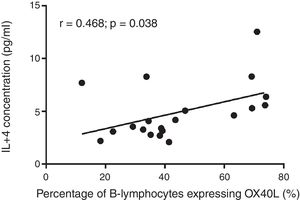
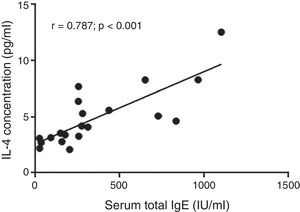
Moreover, there was a significant positive correlation between the OX40L expression levels on B lymphocytes of patients and values of serum total IgE and IL-4 produced by T CD4+ cells in this group (p=0.006 and p=0.038 respectively). Expression of OX40L was not significantly correlated with age (p>0.05) (Table 2 and Figs. 2 and 3). There was also a significant positive correlation between the levels of IgE and IL-4 in the patients (p<0.001) (Fig. 4).
Correlation between the percentages of OX40L+ B cells and other variables among AR patients.
| r | p value | |
|---|---|---|
| Age (years) | −0.165 | 0.488 |
| Serum total IgE level, IU/ml | 0.595 | 0.006* |
| IL-4 cell culture supernatant level, pg/ml | 0.468 | 0.038* |
OX40L, OX40 ligand; AR, allergic rhinitis; IgE, immunoglobulin E; IL-4, interleukin-4.
This study aimed to examine the OX40L expression on B lymphocytes as antigen presenting cells in the peripheral blood of AR patients compared to the healthy subjects. Th2 cells have an important role in the pathogenesis of allergic responses. Activation of these cells by antigen leads to production of Th2 cytokines, such as IL4 and IgE production by B lymphocytes. This is followed by IgE binding to receptors in mast cells and basophils, which activates these cells and produces allergic inflammatory mediators.12 Interaction between OX40 on T lymphocytes with OX40L on activated APCs provides an effective co-stimulatory factor for clonal expansion of T cells and their activation and survival as well as their progress toward the memory cells.8,13
Since AR is diagnosed, based on the clinical results and there are few screening tests available to diagnose it, measurement of the serum level of total IgE is considered beneficial even though it has a low negative predictive value in the general population. According to the results of one study, in vitro testing for specific IgE may be unnecessary in patients with low serum total IgE (IgE<10IU/ml), whereas high total IgE level (IgE>150IU/ml) suggests that in vitro testing would confirm specific sensitizations in patients with allergic rhinitis.14 Thus, as expected, the results of this study affirmed that the serum level of IgE in the AR patients increased significantly compared with the controls.
This study showed that OX40L expression level on B lymphocytes of patients with AR was significantly higher than the healthy subjects. This finding suggests that this up-regulation on patients B lymphocytes could be a marker of an atopic reaction. This finding is consistent with related studies, although they are on diseases other than AR, such as asthma. In a study on the levels of OX40L expression on B cells of patients with allergic asthma, the expression level of this receptor in these patients was higher than its level in patients with non-allergic asthma and controls. However, it was not significantly related with forced respiratory volume in 1st second (FEV1) values and the duration of the disease.15 The results of this study are similar to the above study in terms of increased OX40L expression levels on B lymphocytes of AR patients compared to healthy subjects. However, severity and duration of disease were not included in this study.
The findings of this study are in line with other reports which showed that the expression levels of protein and mRNA for OX40L receptor on airway wall of asthmatic patients and animal models of allergy increased.16–18 In addition, the serum level of OX40L increased in children with atopic asthma and was correlated with the severity of disease.19 Lei et al. measured the OX40L level in patients with acute and stable asthma: and found that its level in the acute type was higher than the stable type, and that in both groups this was higher than the healthy subjects, although it decreased after treatment.20
It has been reported that serum OX40L level in atopic dermatitis children can be a reliable factor to determine the severity of disease.21 However, an increase in the levels of OX40 and its ligand in the dermal lesions of atopic dermatitis patients without correlation with the clinical severity was observed.22
This study suggests a close relation between the expression level of OX40L and an atopic mechanism in AR. OX40/OX40L interaction play an important role by activating T lymphocytes and enhancing their differentiation into Th2 cytokines producer cells and increasing IgE secretion by activated B lymphocytes.8,23 Thus, this study indicates a strong positive correlation 24 (r=0.595) between the OX40L expression level on B lymphocytes and IgE production in the AR patients. This finding is consistent with the results of a similar study about asthma indicating the role of OX40L in an allergic mechanism.15
This study also showed a significant increase in IL-4 production by the activated peripheral blood CD4+ T lymphocytes of AR patients group compared with the controls. This finding is consistent with other studies, in which the investigators have found an increase in the level of IL-4 in AR. This study also indicated a very strong positive correlation (r=0.787) between IL-4 produced by CD4+ T lymphocytes and serum IgE levels.24 This positive correlation was also suggested in similar studies, while, mostly between serum IL-4 and IgE levels.25
In addition, the results of this study also showed a strong positive correlation (r=0.468) between the OX40L expression levels on B cells and the amounts of IL-4 in activated CD4+ T cells in patients with AR. However this correlation was weaker than the relationship between OX40L expression and IgE production,24 this result was in line with another study, showing an increase in number of OX40 and OX40L positive cells in the lamina propria tissue of patients with mild asthma. This may be related to the number of eosinophils and IL-4 positive cells in the bronchial submucosa.26
Thus, it appears that an increase in the number of OX40L+ B lymphocytes leads to enhancement of the interaction between these cells and Th2 lymphocytes. This may also increase IgE production by activated B lymphocytes by directing the Th1/Th2 balance more toward Th2 and thus causing greater IL-4 production by these cells. Thus, this is the probable cause of explicit positive correlation indicated in this study.27 Moreover, enhancement of interaction between OX40L on the surface of more abundant B lymphocytes can enhance the allergic inflammation process. This happens along with the OX40 expression on Th2 lymphocytes surface and higher production of IL-4 by these cells through mechanisms of this cytokine, causing enhanced activity of mast cells.5,28 Development of OX40/OX40L signaling on regulatory T lymphocytes lowers the function of these regulatory cells. Hence, the enhancement of interaction between B lymphocytes and Treg lymphocytes may also decrease the inhibitory activity of these cells against other immunological cells like Th1 and Th2, and may increase allergic reactions accordingly: this requires more investigations in the allergic patients.7
It seems that OX40L is effective in determining therapeutic targets in the treatment of allergic diseases: using anti-XO40L antibodies could provide a clear perspective in treatment of allergic diseases.
Preliminary studies indicated that inhibition of OX40/OX40L interaction impaired activation of Th2 cells, which in turn induced reduction of pulmonary inflammation.18 Another study investigating immunotherapy for house dust mite (HDM) allergy in AR patients found that OX40L gene expression and its expression levels on the surface of mononuclear cells decreased in the patients’ blood. Thus, it seems that immunotherapy has a role in the reduction of Th2-type immune responses, mediated by the TSLP-OX40L signaling pathway.29
It was reported that the level of cytokines like IL-4 and IL-10 increased even as interferon gamma (IFN-γ) decreased in bronchial alveolar lavage fluid (BALF) of a mice model of asthma in comparison with control mice. Using anti- OX40L antibody lowered IL-4 and raised IFN-γ levels in the experimental group. Actually, it was indicated that inhibiting co-stimulatory pathway using anti-OX40L neutralizer during sensitization of the mouse with asthma can regulate Th1/Th2 balance, and control pulmonary inflammation and reduce asthma symptoms.30
ConclusionThis study indicates a significant positive correlation between the percentages of OX40 ligand positive B lymphocytes and the serum IgE concentrations, as well as IL-4 produced by CD4+ T lymphocytes. However, the full understanding of this correlation requires more research to be done on the expression of OX40L on other cells such as dendritic cells, mast cells, and epithelial cells, and its interaction with OX40 on the surface of other main immune cells in allergic diseases.
Ethical approvalAll procedures performed in studies involving human participants were in accordance with the Ethics Committee of Isfahan University of Medical Sciences (Code of Ethics: IR.MUI.REC.1394.3.902) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consentInformed consent was obtained from all individual participants included in the study.
FundingThis work was supported by grant 394902 from Isfahan University of Medical Sciences.
Conflict of interestThe authors declare that they have no conflict of interests concerning this article.
The authors wish to thank the authorities in the research council of Isfahan University of Medical Sciences for financial support.