This ISAAC Phase Three synthesis provides summarised information on the main findings of the study, regional tables and figures related to the prevalence and severity of current symptoms of asthma, rhinoconjunctivitis and eczema in the main regions of the world. The large number of surveyed children (≈1,200,000), the large number of centres (233) and countries (98) that participated in ISAAC Phase Three makes this study the most comprehensive survey of these diseases ever undertaken. Globally, the prevalence for current asthma, rhinoconjunctivitis and eczema in the 13–14-year age group was 14.1%, 14.6% and 7.3%, respectively. In the 6–7-year age group the prevalence for current asthma, rhinoconjunctivitis and eczema was 11.7%, 8.5% and 7.9%, respectively. The study shows a wide variability in the prevalence and severity of asthma, rhinoconjunctivitis and eczema which occurs not just between regions and countries but between centres in the same country and centres in the same city. This study definitively establishes that the prevalence of those diseases can be very high in non-affluent centres with low socioeconomic conditions. The large variability also suggests a crucial role of local environment characteristics to determine the differences in prevalence between one place and another. Thus, ISAAC Phase Three has provided a large body of epidemiological information on asthma, rhinoconjunctivitis and eczema in childhood from contrasting environments which is expected to yield new clues about the aetiology of those conditions and reasons for their marked global variability.
Asthma, rhinoconjunctivitis and eczema in childhood have become three of the more important public health problems worldwide. Although in the past it was thought that these diseases occurred more frequently in populations from developed countries, it has been evident since the first global report from the International Study of Asthma and Allergies in Childhood (ISAAC) that prevalence of those conditions in some low-resourced countries was similar or even higher than in developed ones and that a wide variability in their prevalence occurred at regional and even at country level.1–4
Since then, a large body of new national, regional and global information on the prevalence, severity, risk factors, trends and several other aspects related to asthma, rhinoconjunctivitis and eczema in childhood, has been reported by ISAAC.5 The recently completed third ISAAC Phase included the largest number of centres from the main world regions ever studied in regard to these conditions, with about 1,200,000 schoolchildren surveyed; detailed information on the global prevalence and severity of asthma, rhinitis and eczema has been reported in the ISAAC world map journal articles.6–8
The well-known methodological consistency of the ISAAC programme, its originality and especially the inclusion of countries with different cultures, socioeconomic development and lifestyles, has led to its results being employed by several governmental and academic institutions at country and regional level. It has constituted the epidemiological basis for many of the well-known global initiatives on asthma, rhinitis and eczema management in childhood, and for guidelines and recommendations from international health organisations.
This article presents new information on disease overlap (asthma, rhinoconjunctivitis, eczema), socioeconomic and geospatial considerations from ISAAC Phase Three (written questionnaires) concerning the prevalence of asthma, rhinoconjunctivitis and eczema in children aged 6–7 and 13–14 years.
MethodsThe detailed methodology employed by ISAAC to obtain and analyse data for Phase Three, has already been published in detail elsewhere.5,9 Briefly, written questionnaires were self-completed at school by 13–14-year olds and completed at home by parents of 6–7-year olds. Samples of 3000 children for each age group (with a minimum of 1000) within each centre were selected by randomly sampling schools within the study area. Almost all centres studied the 13–14-year age group, but only some centres studied the optional 6–7-year age group. Data checks were undertaken by the ISAAC International Data Centre in Auckland, New Zealand which ensured adherence to the protocol. The English language questionnaire was translated where required, and a back translation to English was provided. In this paper, we focus on the current symptoms (past 12 months) of asthma, rhinoconjunctivitis and eczema; and reported asthma ever.
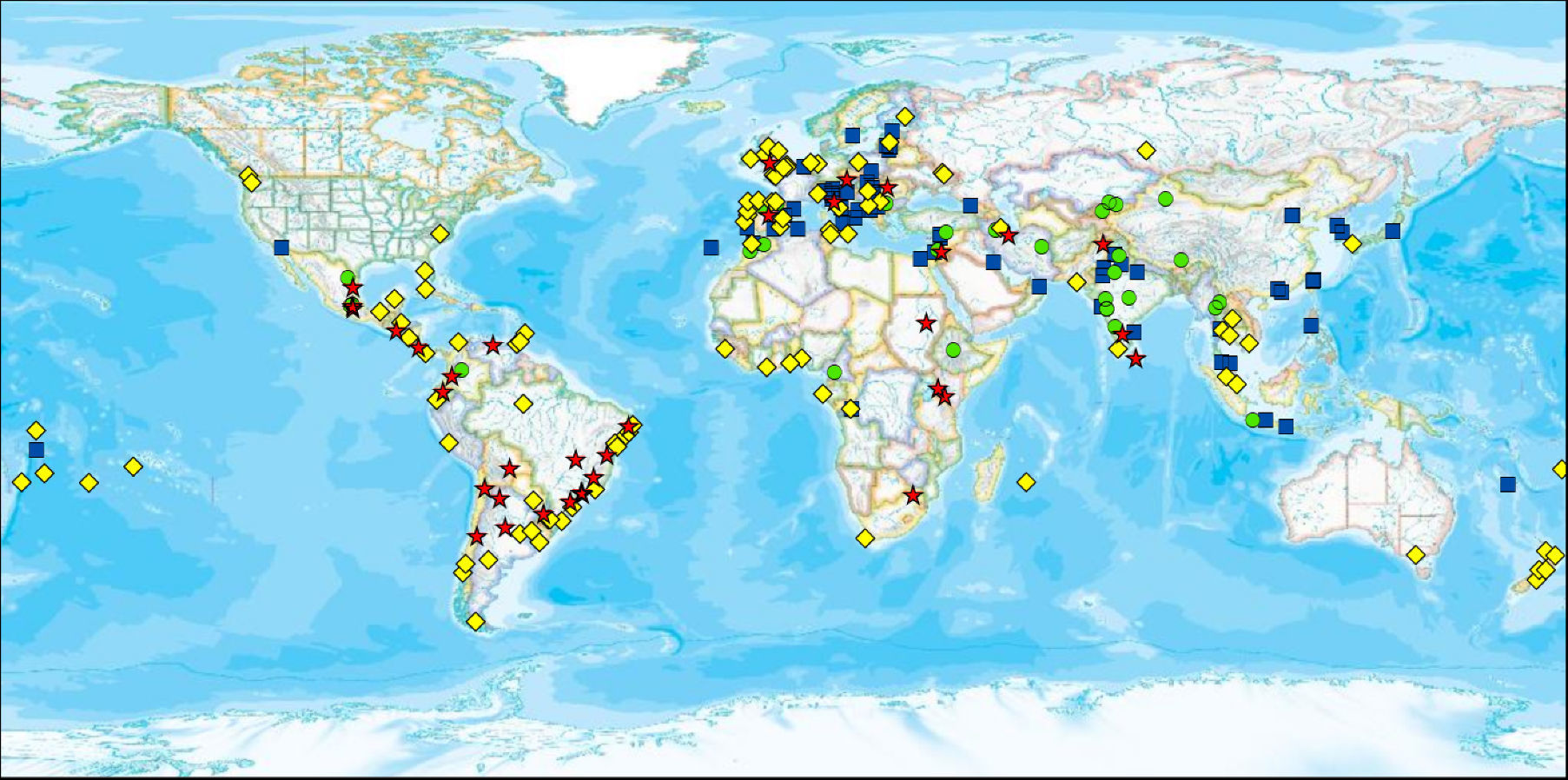
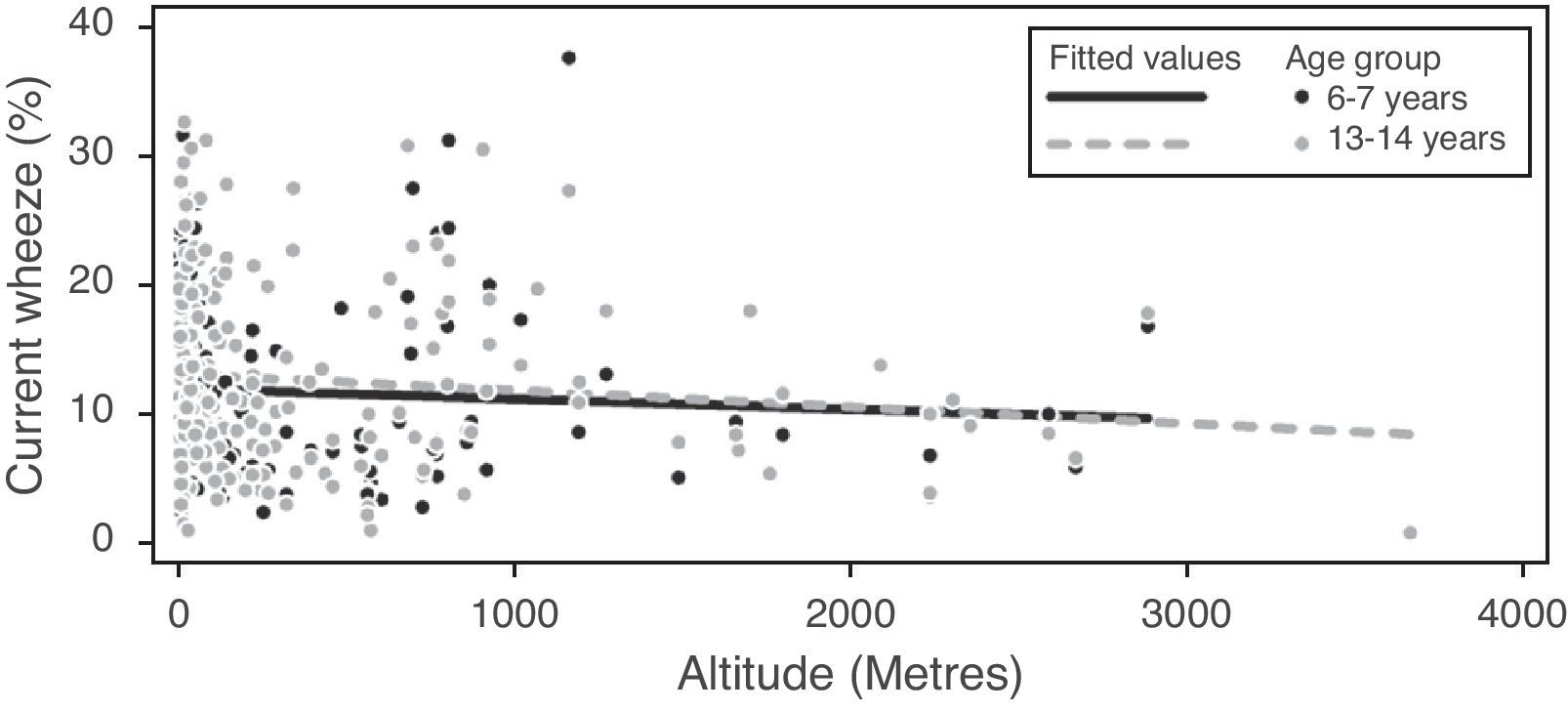
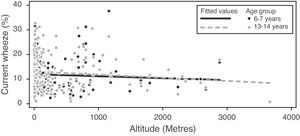
Associations between prevalence of current symptoms of asthma, rhinoconjunctivitis and eczema, and a range of geo-climatic factors were assessed using maps prepared in the ArcGIS geographic information system (version 9.3.1, ESRI Inc., Redlands, CA, USA). The factors presented are altitude,10 air pollution as indicated by the predicted concentrations (micro grams per cubic metre) of particulate matter less than 10μm in diameter (PM10),11 and Gross National Income per capita (GNI).12 High altitude was defined as ≥300m. High PM10 was defined as ≥50μg/m3. Data for altitude and air pollution were available at centre level whereas the GNI data were only available at country level. Non-affluent countries were those classified by the World Bank as low, lower middle, or upper middle income, and affluent countries are those classified as high income. The maps (Figs. 1–3) illustrate the distribution of low and high values of prevalence and GNI, altitude and PM10. For current symptoms of asthma (current wheeze) and current symptoms of eczema, high prevalence centres were defined as those with prevalence of 10% or greater. For current symptoms of rhinoconjunctivitis, high prevalence centres were defined as those with prevalence of 15% or greater for the 13–14-year age group and 7.5% or greater for the 6–7-year age group. These definitions are based on the levels used in the maps presented in the ISAAC prevalence papers.1–4,6–8 Spearman correlation (rho) was used to study the association of altitude, latitude and longitude with the prevalence of current symptoms of asthma, rhinoconjunctivitis and eczema.
Geospatial distribution of prevalence of current symptoms of asthma and country income, 13–14-year age group. Each symbol represents a centre. The four symbols depict different levels of prevalence of symptoms combined with their categorisation as affluent or non-affluent. Red stars indicate high prevalence of current symptoms of asthma (≥10%) and affluent (GNI>$9265); yellow diamonds indicate high prevalence of current symptoms of asthma and non-affluent; green circles indicate low prevalence of current symptoms of asthma and affluent; and blue squares indicate low prevalence of current symptoms of asthma and non-affluent. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of the article.)
Geospatial distribution of prevalence of current symptoms of asthma and altitude, 13–14-year age group. Each symbol represents a centre. The four symbols depict different levels of prevalence of symptoms combined with their categorisation as low or high altitude. Red stars indicate high prevalence of current symptoms of asthma (≥10%) and high altitude (≥300m); yellow diamonds indicate high prevalence of current symptoms of asthma and low altitude; green circles indicate low prevalence of current symptoms of asthma and high altitude; and blue squares indicate low prevalence of current symptoms of asthma and low altitude. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of the article.)
Geospatial distribution of prevalence of current symptoms of asthma and particulate matter (PM10), 13–14-year age group. Each symbol represents a centre. The four symbols depict different levels of prevalence of symptoms combined with their categorisation as low or high (PM10). Red stars indicate high prevalence of current symptoms of asthma (≥10%) and high PM10 (≥50μg/m3); yellow diamonds indicate high prevalence of current symptoms of asthma and low PM10; green circles indicate low prevalence of current symptoms of asthma and high PM10; and blue squares indicate low prevalence of current symptoms of asthma and low PM10. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of the article.)
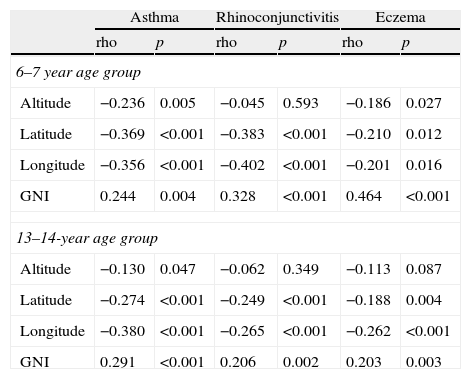
Spearman's correlation (rho) was employed to determine associations between current symptoms of asthma, rhinoconjunctivitis and eczema, with centre level altitude, latitude, longitude and PM10, and with country level GNI, in 6–7-year and 13–14-year age groups.
ResultsParticipantsISAAC Phase Three surveyed about 1,200,000 children from 233 centres in 98 countries, involving almost 800,000 children aged 13–14 years and almost 400,000 aged 6–7 years. For asthma the data sets comprised 1,187,496 schoolchildren from 233 centres in 98 countries, of whom 128 centres (689,413 participants) in 64 countries (34 countries new to ISAAC) had not undertaken ISAAC Phase One; 798,685 were aged 13–14 years and 388,811 were aged 6–7 years. The majority of the new ISAAC centres were from countries in Latin America, Eastern Europe and Africa, although there were also some from other regions.7 In the case of rhinoconjunctivitis, the 13–14-year age group involved 670,242 children and 388,811 children aged 6–7 years. Regarding eczema, for the 13–14-year age group there were 663,256 children and 385,853 for the 6–7-year age group.8 Of the 54 languages used in Phase Three, English was the most common (21% of centres) followed by Spanish (20%), Portuguese (11%), Arabic (7%), Italian (6%), French (5%) and Chinese (4%). The number of participating centres per region ranged from seven in North America to 56 in Latin America.
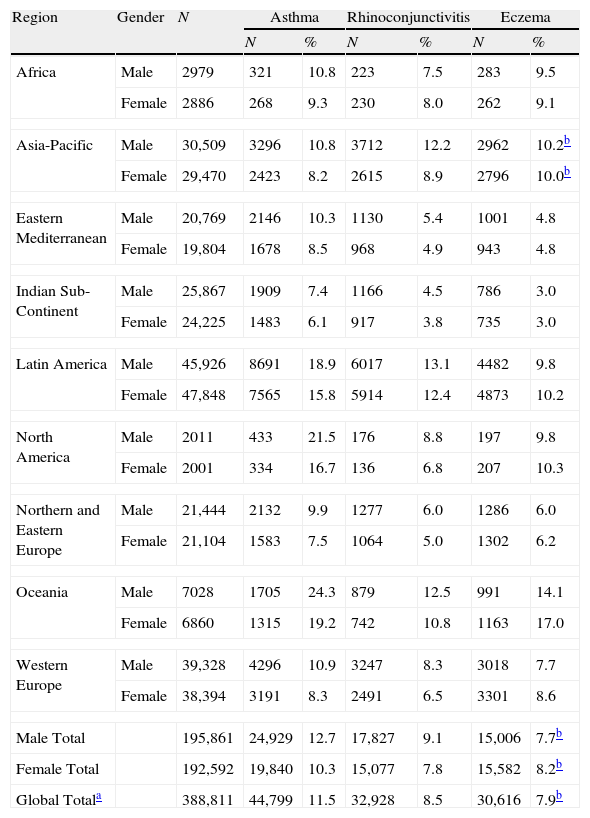
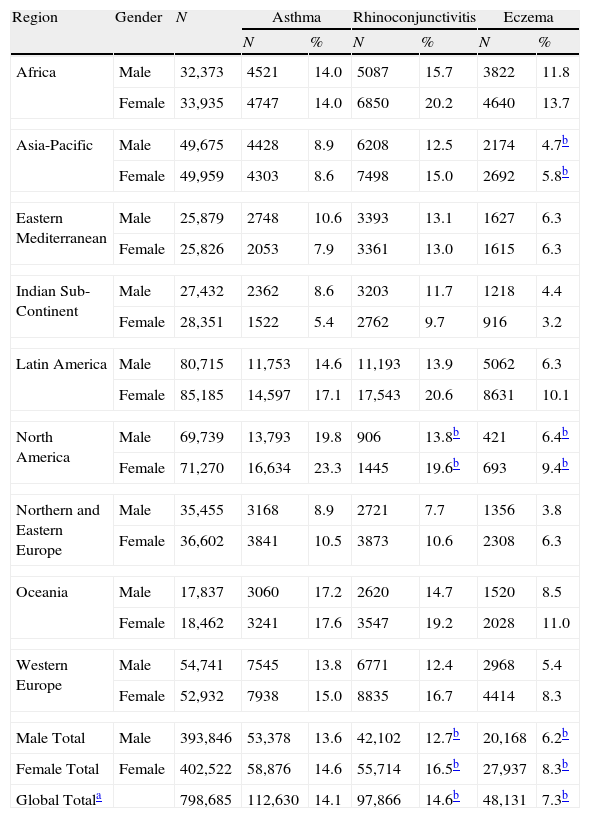
Symptoms by region and genderThe regional prevalences of current symptoms for the three conditions are shown in Tables 1 and 2 by gender.
Prevalence of current symptoms of asthma, rhinoconjunctivitis and eczema by world region and gender, 6–7-year age group.
| Region | Gender | N | Asthma | Rhinoconjunctivitis | Eczema | |||
| N | % | N | % | N | % | |||
| Africa | Male | 2979 | 321 | 10.8 | 223 | 7.5 | 283 | 9.5 |
| Female | 2886 | 268 | 9.3 | 230 | 8.0 | 262 | 9.1 | |
| Asia-Pacific | Male | 30,509 | 3296 | 10.8 | 3712 | 12.2 | 2962 | 10.2b |
| Female | 29,470 | 2423 | 8.2 | 2615 | 8.9 | 2796 | 10.0b | |
| Eastern Mediterranean | Male | 20,769 | 2146 | 10.3 | 1130 | 5.4 | 1001 | 4.8 |
| Female | 19,804 | 1678 | 8.5 | 968 | 4.9 | 943 | 4.8 | |
| Indian Sub-Continent | Male | 25,867 | 1909 | 7.4 | 1166 | 4.5 | 786 | 3.0 |
| Female | 24,225 | 1483 | 6.1 | 917 | 3.8 | 735 | 3.0 | |
| Latin America | Male | 45,926 | 8691 | 18.9 | 6017 | 13.1 | 4482 | 9.8 |
| Female | 47,848 | 7565 | 15.8 | 5914 | 12.4 | 4873 | 10.2 | |
| North America | Male | 2011 | 433 | 21.5 | 176 | 8.8 | 197 | 9.8 |
| Female | 2001 | 334 | 16.7 | 136 | 6.8 | 207 | 10.3 | |
| Northern and Eastern Europe | Male | 21,444 | 2132 | 9.9 | 1277 | 6.0 | 1286 | 6.0 |
| Female | 21,104 | 1583 | 7.5 | 1064 | 5.0 | 1302 | 6.2 | |
| Oceania | Male | 7028 | 1705 | 24.3 | 879 | 12.5 | 991 | 14.1 |
| Female | 6860 | 1315 | 19.2 | 742 | 10.8 | 1163 | 17.0 | |
| Western Europe | Male | 39,328 | 4296 | 10.9 | 3247 | 8.3 | 3018 | 7.7 |
| Female | 38,394 | 3191 | 8.3 | 2491 | 6.5 | 3301 | 8.6 | |
| Male Total | 195,861 | 24,929 | 12.7 | 17,827 | 9.1 | 15,006 | 7.7b | |
| Female Total | 192,592 | 19,840 | 10.3 | 15,077 | 7.8 | 15,582 | 8.2b | |
| Global Totala | 388,811 | 44,799 | 11.5 | 32,928 | 8.5 | 30,616 | 7.9b | |
Prevalence of current symptoms of asthma, rhinoconjunctivitis and eczema by region and gender, 13–14-year age group.
| Region | Gender | N | Asthma | Rhinoconjunctivitis | Eczema | |||
| N | % | N | % | N | % | |||
| Africa | Male | 32,373 | 4521 | 14.0 | 5087 | 15.7 | 3822 | 11.8 |
| Female | 33,935 | 4747 | 14.0 | 6850 | 20.2 | 4640 | 13.7 | |
| Asia-Pacific | Male | 49,675 | 4428 | 8.9 | 6208 | 12.5 | 2174 | 4.7b |
| Female | 49,959 | 4303 | 8.6 | 7498 | 15.0 | 2692 | 5.8b | |
| Eastern Mediterranean | Male | 25,879 | 2748 | 10.6 | 3393 | 13.1 | 1627 | 6.3 |
| Female | 25,826 | 2053 | 7.9 | 3361 | 13.0 | 1615 | 6.3 | |
| Indian Sub-Continent | Male | 27,432 | 2362 | 8.6 | 3203 | 11.7 | 1218 | 4.4 |
| Female | 28,351 | 1522 | 5.4 | 2762 | 9.7 | 916 | 3.2 | |
| Latin America | Male | 80,715 | 11,753 | 14.6 | 11,193 | 13.9 | 5062 | 6.3 |
| Female | 85,185 | 14,597 | 17.1 | 17,543 | 20.6 | 8631 | 10.1 | |
| North America | Male | 69,739 | 13,793 | 19.8 | 906 | 13.8b | 421 | 6.4b |
| Female | 71,270 | 16,634 | 23.3 | 1445 | 19.6b | 693 | 9.4b | |
| Northern and Eastern Europe | Male | 35,455 | 3168 | 8.9 | 2721 | 7.7 | 1356 | 3.8 |
| Female | 36,602 | 3841 | 10.5 | 3873 | 10.6 | 2308 | 6.3 | |
| Oceania | Male | 17,837 | 3060 | 17.2 | 2620 | 14.7 | 1520 | 8.5 |
| Female | 18,462 | 3241 | 17.6 | 3547 | 19.2 | 2028 | 11.0 | |
| Western Europe | Male | 54,741 | 7545 | 13.8 | 6771 | 12.4 | 2968 | 5.4 |
| Female | 52,932 | 7938 | 15.0 | 8835 | 16.7 | 4414 | 8.3 | |
| Male Total | Male | 393,846 | 53,378 | 13.6 | 42,102 | 12.7b | 20,168 | 6.2b |
| Female Total | Female | 402,522 | 58,876 | 14.6 | 55,714 | 16.5b | 27,937 | 8.3b |
| Global Totala | 798,685 | 112,630 | 14.1 | 97,866 | 14.6b | 48,131 | 7.3b | |
There was large variability of prevalence between regions for symptoms of each of the three conditions and both age groups. For the younger age group the lowest prevalence values for asthma symptoms were found in the Indian Subcontinent, with intermediate values in Africa, Asia-Pacific, Eastern Mediterranean, Northern and Eastern Europe, Western Europe, and the highest levels in Latin America, North America, and Oceania. The lowest prevalence values for rhinoconjunctivitis symptoms were found in Eastern Mediterranean, Indian Subcontinent, and Northern and Eastern Europe, with intermediate values in Africa, Asia-Pacific, and, Western Europe, and the highest in Latin America, North America, and Oceania. The lowest prevalence values for symptoms of eczema were found in Eastern Mediterranean, Indian Subcontinent, with intermediate values in Africa, Asia-Pacific, and Northern and Eastern Europe, Western Europe, North America, and the highest values in Latin America, and Oceania.
For the older age group the lowest prevalence values for asthma symptoms were found in Asia-Pacific, Eastern Mediterranean, Indian Subcontinent, and Northern and Eastern Europe, with intermediate values in Africa and Oceania, Western Europe, and Latin America, and the highest in North America. The lowest prevalence values for rhinoconjunctivitis symptoms were found in Indian Subcontinent, and Northern and Eastern Europe, with intermediate values in Asia-Pacific, Eastern Mediterranean, Oceania and Western Europe, and the highest values in Africa, Latin America, and North America. The lowest prevalence values for symptoms of eczema were found in Asia-Pacific, Eastern Mediterranean, Indian Subcontinent, and Northern and Eastern Europe, with intermediate values in Latin America, Oceania, North America, and Western Europe, and the highest values in Africa.
The summaries by gender for symptoms of each of the three diseases and both age groups showed that in the younger age group there were more boys than girls with asthma and rhinoconjunctivitis symptoms, and this held true for all regions for asthma, and most for rhinoconjunctivitis symptoms, but eczema symptoms overall were more common in girls although this varied across the regions. In the older age group there were more girls than boys with symptoms of all three conditions, and this held true for most regions.
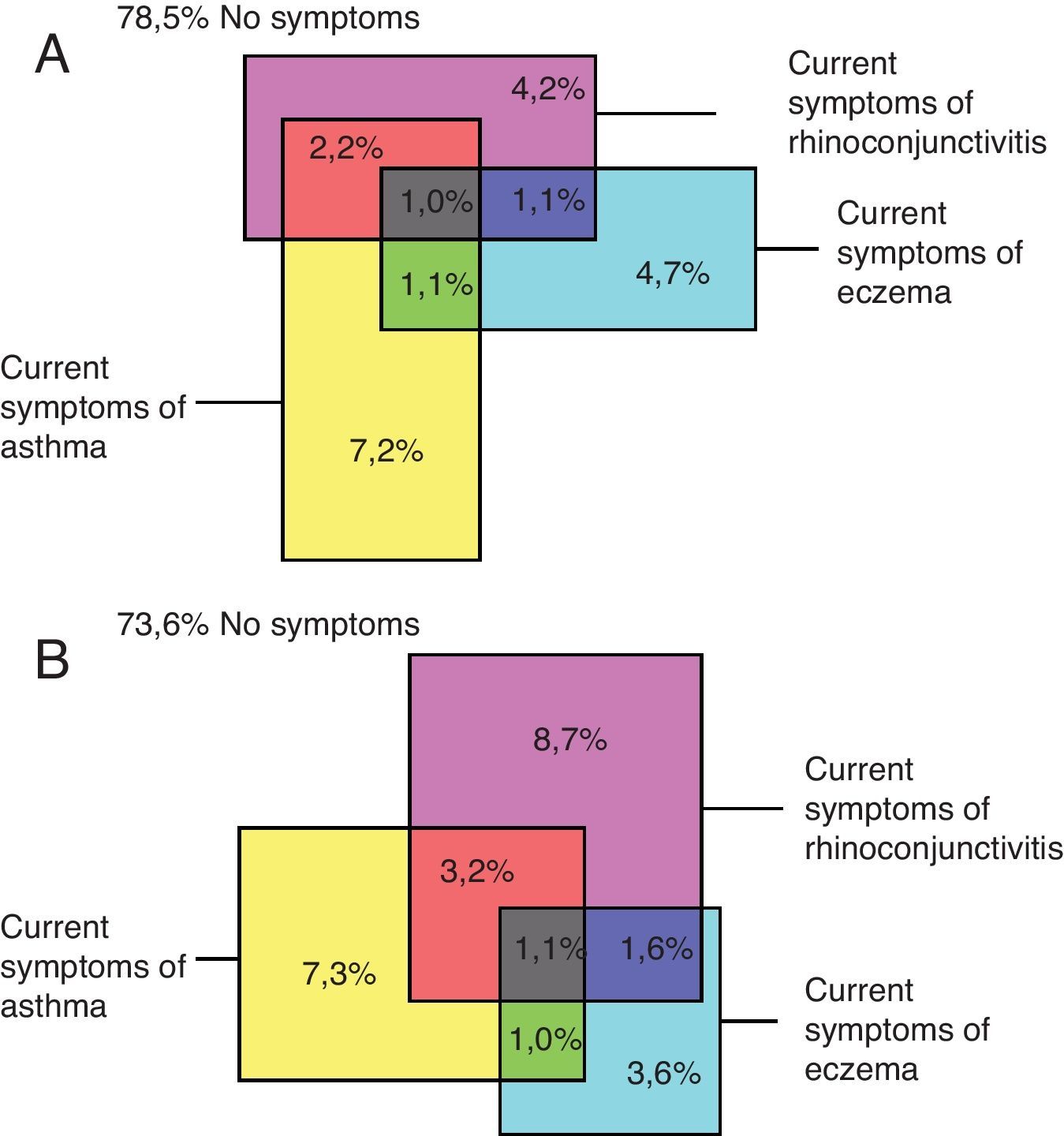
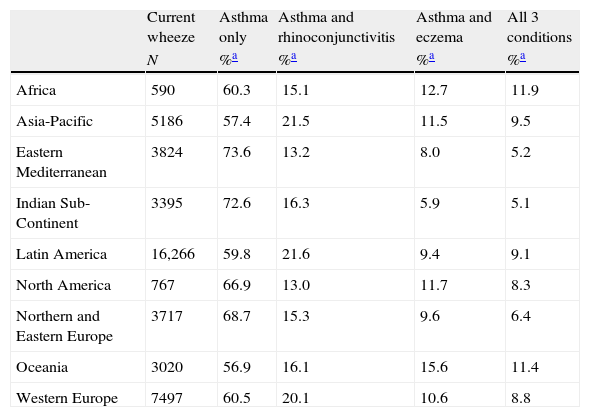
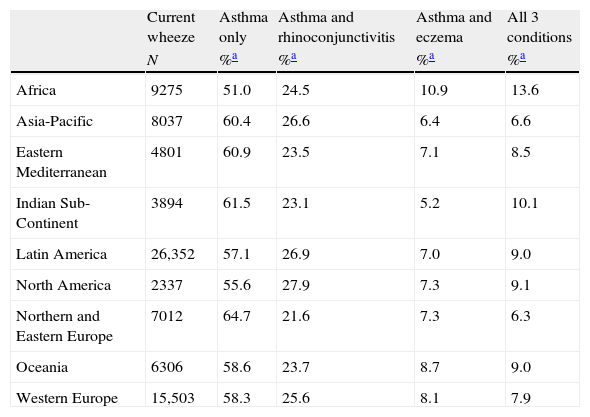
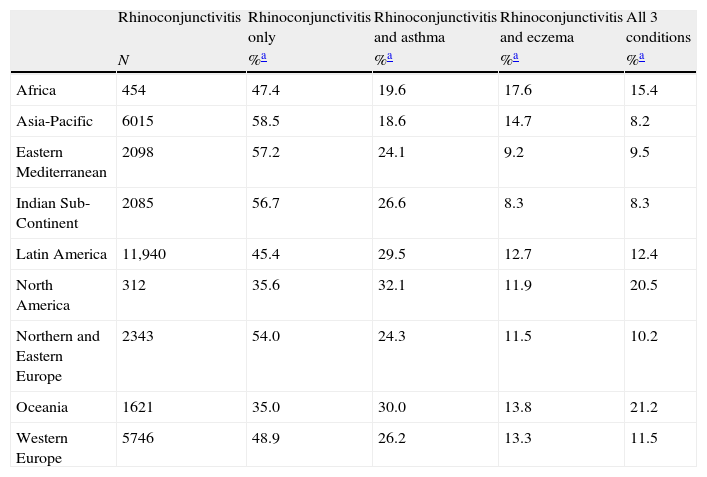
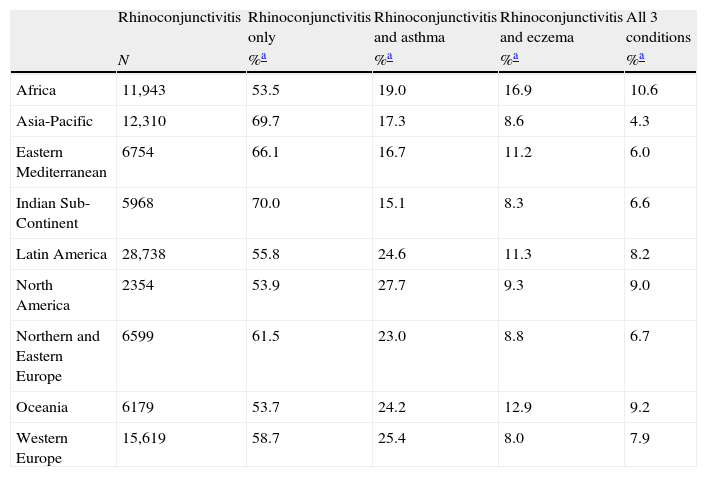
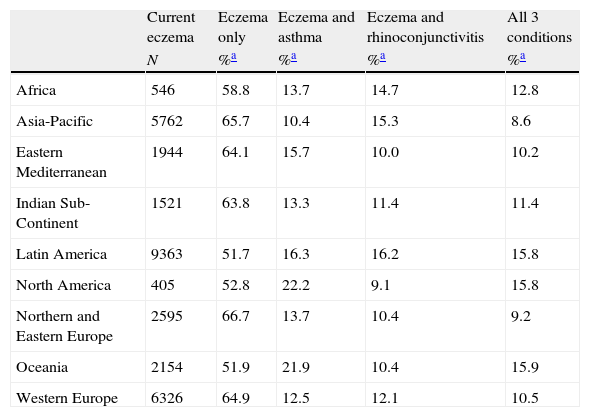
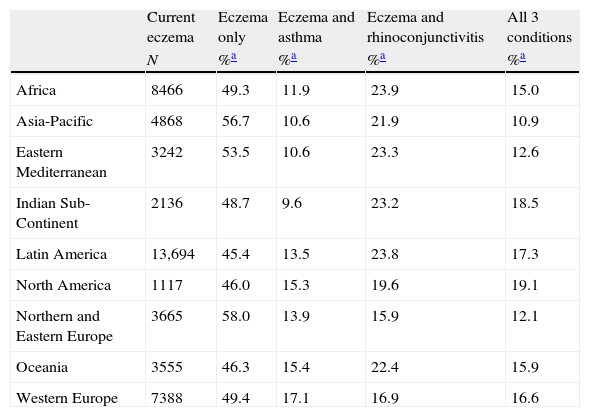
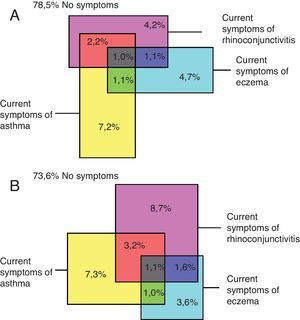
Concurrent prevalence of symptoms of current asthma, rhinoconjunctivitis and eczemaA low proportion of children simultaneously reported current symptoms of asthma, rhinoconjunctivitis and eczema. Amongst the world regions there was a large variability in the prevalence of the three diseases; for those with current symptoms of asthma the prevalence for the concurrence of the three conditions varied from 6.3% in Northern and Eastern Europe to 13.6% in Africa in the 13–14 years old group and from 5.1% in the Indian Subcontinent to 11.9% in Africa in those aged 6–7 years. The relative proportions for the regional concurrent prevalence of the three diseases are presented in Tables 3–8.
Prevalence of current symptoms of asthma only with associated co-morbidities, 6–7-year age group.
| Current wheeze | Asthma only | Asthma and rhinoconjunctivitis | Asthma and eczema | All 3 conditions | |
| N | %a | %a | %a | %a | |
| Africa | 590 | 60.3 | 15.1 | 12.7 | 11.9 |
| Asia-Pacific | 5186 | 57.4 | 21.5 | 11.5 | 9.5 |
| Eastern Mediterranean | 3824 | 73.6 | 13.2 | 8.0 | 5.2 |
| Indian Sub-Continent | 3395 | 72.6 | 16.3 | 5.9 | 5.1 |
| Latin America | 16,266 | 59.8 | 21.6 | 9.4 | 9.1 |
| North America | 767 | 66.9 | 13.0 | 11.7 | 8.3 |
| Northern and Eastern Europe | 3717 | 68.7 | 15.3 | 9.6 | 6.4 |
| Oceania | 3020 | 56.9 | 16.1 | 15.6 | 11.4 |
| Western Europe | 7497 | 60.5 | 20.1 | 10.6 | 8.8 |
Prevalence of current symptoms of asthma only with associated co-morbidities, 13–14-year age group.
| Current wheeze | Asthma only | Asthma and rhinoconjunctivitis | Asthma and eczema | All 3 conditions | |
| N | %a | %a | %a | %a | |
| Africa | 9275 | 51.0 | 24.5 | 10.9 | 13.6 |
| Asia-Pacific | 8037 | 60.4 | 26.6 | 6.4 | 6.6 |
| Eastern Mediterranean | 4801 | 60.9 | 23.5 | 7.1 | 8.5 |
| Indian Sub-Continent | 3894 | 61.5 | 23.1 | 5.2 | 10.1 |
| Latin America | 26,352 | 57.1 | 26.9 | 7.0 | 9.0 |
| North America | 2337 | 55.6 | 27.9 | 7.3 | 9.1 |
| Northern and Eastern Europe | 7012 | 64.7 | 21.6 | 7.3 | 6.3 |
| Oceania | 6306 | 58.6 | 23.7 | 8.7 | 9.0 |
| Western Europe | 15,503 | 58.3 | 25.6 | 8.1 | 7.9 |
Prevalence of current symptoms of rhinoconjunctivitis with associated co-morbidities, 6–7-year age group.
| Rhinoconjunctivitis | Rhinoconjunctivitis only | Rhinoconjunctivitis and asthma | Rhinoconjunctivitis and eczema | All 3 conditions | |
| N | %a | %a | %a | %a | |
| Africa | 454 | 47.4 | 19.6 | 17.6 | 15.4 |
| Asia-Pacific | 6015 | 58.5 | 18.6 | 14.7 | 8.2 |
| Eastern Mediterranean | 2098 | 57.2 | 24.1 | 9.2 | 9.5 |
| Indian Sub-Continent | 2085 | 56.7 | 26.6 | 8.3 | 8.3 |
| Latin America | 11,940 | 45.4 | 29.5 | 12.7 | 12.4 |
| North America | 312 | 35.6 | 32.1 | 11.9 | 20.5 |
| Northern and Eastern Europe | 2343 | 54.0 | 24.3 | 11.5 | 10.2 |
| Oceania | 1621 | 35.0 | 30.0 | 13.8 | 21.2 |
| Western Europe | 5746 | 48.9 | 26.2 | 13.3 | 11.5 |
Prevalence of current symptoms of rhinoconjunctivitis with associated co-morbidities, 13–14-year age group.
| Rhinoconjunctivitis | Rhinoconjunctivitis only | Rhinoconjunctivitis and asthma | Rhinoconjunctivitis and eczema | All 3 conditions | |
| N | %a | %a | %a | %a | |
| Africa | 11,943 | 53.5 | 19.0 | 16.9 | 10.6 |
| Asia-Pacific | 12,310 | 69.7 | 17.3 | 8.6 | 4.3 |
| Eastern Mediterranean | 6754 | 66.1 | 16.7 | 11.2 | 6.0 |
| Indian Sub-Continent | 5968 | 70.0 | 15.1 | 8.3 | 6.6 |
| Latin America | 28,738 | 55.8 | 24.6 | 11.3 | 8.2 |
| North America | 2354 | 53.9 | 27.7 | 9.3 | 9.0 |
| Northern and Eastern Europe | 6599 | 61.5 | 23.0 | 8.8 | 6.7 |
| Oceania | 6179 | 53.7 | 24.2 | 12.9 | 9.2 |
| Western Europe | 15,619 | 58.7 | 25.4 | 8.0 | 7.9 |
Prevalence of current symptoms of eczema with associated co-morbidities, 6–7-year age group.
| Current eczema | Eczema only | Eczema and asthma | Eczema and rhinoconjunctivitis | All 3 conditions | |
| N | %a | %a | %a | %a | |
| Africa | 546 | 58.8 | 13.7 | 14.7 | 12.8 |
| Asia-Pacific | 5762 | 65.7 | 10.4 | 15.3 | 8.6 |
| Eastern Mediterranean | 1944 | 64.1 | 15.7 | 10.0 | 10.2 |
| Indian Sub-Continent | 1521 | 63.8 | 13.3 | 11.4 | 11.4 |
| Latin America | 9363 | 51.7 | 16.3 | 16.2 | 15.8 |
| North America | 405 | 52.8 | 22.2 | 9.1 | 15.8 |
| Northern and Eastern Europe | 2595 | 66.7 | 13.7 | 10.4 | 9.2 |
| Oceania | 2154 | 51.9 | 21.9 | 10.4 | 15.9 |
| Western Europe | 6326 | 64.9 | 12.5 | 12.1 | 10.5 |
Prevalence of current symptoms of eczema with associated co-morbidities, 13–14-year age group.
| Current eczema | Eczema only | Eczema and asthma | Eczema and rhinoconjunctivitis | All 3 conditions | |
| N | %a | %a | %a | %a | |
| Africa | 8466 | 49.3 | 11.9 | 23.9 | 15.0 |
| Asia-Pacific | 4868 | 56.7 | 10.6 | 21.9 | 10.9 |
| Eastern Mediterranean | 3242 | 53.5 | 10.6 | 23.3 | 12.6 |
| Indian Sub-Continent | 2136 | 48.7 | 9.6 | 23.2 | 18.5 |
| Latin America | 13,694 | 45.4 | 13.5 | 23.8 | 17.3 |
| North America | 1117 | 46.0 | 15.3 | 19.6 | 19.1 |
| Northern and Eastern Europe | 3665 | 58.0 | 13.9 | 15.9 | 12.1 |
| Oceania | 3555 | 46.3 | 15.4 | 22.4 | 15.9 |
| Western Europe | 7388 | 49.4 | 17.1 | 16.9 | 16.6 |
The global prevalence of current symptoms of the three diseases reported simultaneously by children is shown in Fig. 4.
Prevalence in centres related to socioeconomic status of countriesIn both, the 6–7 and 13–14-year age groups, GNI was positively correlated (Spearman's rho) with current symptoms of asthma, rhinoconjunctivitis and eczema (Table 9). The geospatial distribution of current symptoms of asthma and GNI is shown in Fig. 1. There are four patterns of centres shown: a high prevalence in affluent centres; a high prevalence in non-affluent centres; a low prevalence in affluent centres; and a low prevalence in non-affluent centres.
Associations (Spearman's rho) between current symptoms of asthma, rhinoconjunctivitis and eczema, with centre level altitude, latitude, longitude and PM10, and with country level GNI, in 6–7-year (144 centres) and 13–14-year age groups (233 centres).
| Asthma | Rhinoconjunctivitis | Eczema | ||||
| rho | p | rho | p | rho | p | |
| 6–7 year age group | ||||||
| Altitude | −0.236 | 0.005 | −0.045 | 0.593 | −0.186 | 0.027 |
| Latitude | −0.369 | <0.001 | −0.383 | <0.001 | −0.210 | 0.012 |
| Longitude | −0.356 | <0.001 | −0.402 | <0.001 | −0.201 | 0.016 |
| GNI | 0.244 | 0.004 | 0.328 | <0.001 | 0.464 | <0.001 |
| 13–14-year age group | ||||||
| Altitude | −0.130 | 0.047 | −0.062 | 0.349 | −0.113 | 0.087 |
| Latitude | −0.274 | <0.001 | −0.249 | <0.001 | −0.188 | 0.004 |
| Longitude | −0.380 | <0.001 | −0.265 | <0.001 | −0.262 | <0.001 |
| GNI | 0.291 | <0.001 | 0.206 | 0.002 | 0.203 | 0.003 |
Globally, it was found that lower latitudes and Eastern longitudes were slightly but significantly associated with higher prevalence of current symptoms of asthma, and rhinoconjunctivitis and eczema in both age groups (Table 9). However, this was not a consistent finding. For instance, in large regions including both hemispheres as Latin America, no significant association was found between latitude/longitude and prevalence of current symptoms. The mean prevalence of the three diseases was similar in centres located in tropical versus non-tropical areas. The distribution of prevalence of current symptoms by altitude in the group aged 13–14 years (Fig. 5) showed a weak but significant inverse correlation just for current asthma but not for rhinoconjunctivitis or eczema; in the 6–7-year age group there was a weak but significant inverse relationship between altitude, asthma and eczema but not with rhinoconjunctivitis (Table 9).
Particulate matter less than or equal to 10μm (PM10) and the relationship with current prevalence of asthma, rhinoconjunctivitis and eczemaOverall, ISAAC Phase Three found that PM10 showed a trend to be inversely related with current symptoms of asthma, rhinoconjunctivitis and eczema at level centre; however, the relationship was inconsistent or null at within-country level.
DiscussionThis is the largest study of asthma, rhinoconjunctivitis and eczema ever conducted, and the first time that the relationship between the three diseases, and various geospatial and geo-climatic phenomena has been examined. ISAAC Phase Three was performed in all WHO regions thus the main continents and ethnic areas of the world were represented in the study.
The large variability of prevalence between regions, continents, countries, centres in the same country, and even between centres in the same city (as in Mexico City) is probably the main and most consistent finding of ISAAC.6–8 The marked difference of prevalence between centres in the same city, as occurred in Mexico City, has also been found amongst New York neighbourhoods, with a 3–19% difference in asthma prevalence across the city associated with variations in allergen exposures.13 This highlights the heightened impact of still undefined local environmental or ecologic factors present at each centre, which may determine varying epidemiological and clinical expressions of diseases in populations at similar settings.14–16 The latter, i.e. the influence of local variation in exposures on prevalence, seems to be supported by the large variability found amongst centres in the prevalence of allergen sensitisation 17 and airway hyperresponsiveness.18
Although the whole study found a subtle relationship between GNI and overall symptom prevalence, in large regions such as Latin America (56 centres in 17 countries), which accounted for about 25% of all the children surveyed by ISAAC Phase Three in the world,19 there was not a significant correlation between GNI and prevalence. Using the GNI or other country-average index to study the effect of socioeconomic status on the prevalence of current symptoms, especially when including centres from affluent and non-affluent countries, may be misleading, since the income distribution in developing countries is highly unequal. Therefore, assigning the GNI of a developing country to all centres in that country would be inadequate because the risk of losing the large differences in income distribution between centres in developing countries, and regions.20 Until socioeconomic data at an individual level are available for all participating centres, the effect of socioeconomic development on the prevalence and severity of asthma, rhinoconjunctivitis and eczema will be bedevilled by this methodological issue. The results of studies looking at the relationship between socioeconomic status and prevalence of symptoms vary from an inverse association,21–24 to no association25 to a positive association26; apart from methodological considerations which may reflect the lack of proper and standardised instruments to assess such associations at centre or individual level.
Higher or lower prevalence of current symptoms of asthma, rhinoconjunctivitis and eczema occurred regardless of whether centres were located in developing or developed countries or regions,1,2,5–8 and this was consistent with the findings of ISAAC Phase One.2 For instance, in Africa the 13–14-year age group had the same mean prevalence of current wheezing as Western Europe (14%); similar prevalence of rhinoconjunctivitis and eczema also occurred between developing and developed countries, as shown in Tables 1 and 2. In general, most centres with a high or low prevalence in Phase Three tended to remain close to the level of prevalence they had in Phase One; although there were some centres showing important increases or decreases between the two phases. In areas sharing the same language but different socioeconomic development, the prevalence of current asthma symptoms was higher in developing than developed countries (i.e., Iberian Peninsula vs. Latin America).19
The inclusion of many more centres from developing countries in Phase Three than in Phase One is an important achievement of ISAAC as the proportion of the world population that lives in developing areas is about 80%. This is important because several theories on asthma causation are related to the protective effect of factors usually associated with low socioeconomic status. Considering that conditions of poverty have been persistently affecting populations in developing areas for a long time, without dramatic changes in the last 20 years, a lower prevalence of asthma, rhinoconjunctivitis, and eczema would have been expected in children and adolescents from those low-resourced countries. The participation of many more centres from developing countries certainly provides a more realistic representation of the world prevalence of asthma, rhinoconjunctivitis and eczema in childhood. At present, and thanks to the information gathered by ISAAC, the old statement that asthma was just a disease of industrialised and developed countries can be considered simply as an exclusion bias.
As in Phase One, most symptomatic children had symptoms of only one disorder in the previous year, which indicates that many different risk factors may be required for the clinical expression of these related disorders or may involve different time of occurrence, latency periods and time trends.
Although the proportion of subjects having the three diseases simultaneously was relatively low, those children probably represent a highly demanding group for specialised health care. Furthermore, it is likely that as seen in daily practice, coexistence of these diseases may be associated with greater functional impairment in terms of activity limitation and lower quality of life as compared to children who have one condition alone. Co-morbidities are important for clinicians treating asthma as they may be markers of patients at risk of poor outcomes, they may point to specific effective treatment options and they are important to researchers as possible confounding factors in clinical trials.
The effect of geo-climatic factors on the current symptom prevalence should be interpreted cautiously because of the dynamic nature of climatic factors that sometimes act independently of latitude and longitude, as is apparently occurring in this last decade. Consequently, geo-climatic factors should be considered as part of a much more complex model interacting with several other ecological conditions which also could be altered by seasonal or yearly changes. As other authors previously found,27,28 ISAAC Phase Three found correlations between some geo-climatic factors and the prevalence of asthma, rhinoconjunctivitis and eczema; however, the interpretation and time-dependency of such effects remains difficult to understand.
The complex relationships between air pollution and symptoms of asthma, rhinoconjunctivitis and eczema probably cannot be elucidated from data as those obtained by ISAAC. Further information on the type, magnitude and temporality of exposures, which also consider variations caused by geo-climatic (i.e. seasonal) factors, should help to a better understanding of the true effects of air pollution on the prevalence of asthma, rhinoconjunctivitis and eczema in children.
LimitationsIn some way, ISAAC shares the potential limitations of any large multicentre international cross-sectional study (differences in language, socioeconomic development, lifestyle, cultural standard, environmental aspects, educational level, medical practice and health concepts, amongst others). We acknowledge the limitations of international prevalence comparisons of this kind and also of interpretations on its findings. Another concern is that centre GNI was assumed to be the same as country GNI. Unfortunately, for most of the centres in developing countries or regions there is no official information available regarding socioeconomic status. At present, it is clear that in those countries or areas with huge inequities of income distribution 19 the wholesale application of a country level measure to all centres conceals more than it reveals.Nevertheless, the worldwide scope of ISAAC Phase Three including centres across the main world regions, the use of standardised and validated methodology, a meticulous translation of questionnaires to different languages,29 strict data quality control and management, and a thorough repetition of the study after several years, has provided for the first time a unique and fundamental epidemiological analysis of the world distribution and trend of the prevalence and severity of asthma, rhinoconjunctivitis and eczema in children.30 At the same time ISAAC has provided a stimulus for the development of new hypotheses and a challenge to identify modifiable protective and risk factors for asthma, and the other diseases studied. The worldwide time trends in the prevalence of current symptoms are not described in the present paper because they have been extensively detailed elsewhere.31–33
As found in ISAAC Phase One, there was a low degree of overlap between the three conditions2 suggesting that asthma, rhinoconjunctivitis and eczema may have different aetiologies, time of occurrence and clinical course, probably related with particular enviromental exposures at each locality or area.The wide variability of the prevalence of the studied diseases, found by ISAAC in all its phases, strongly points to local ecological factors or exposures which are probably typical for each locality, as the main determinants for the observed variability of symptoms, allergic sensitisation and airways hyperresponsiveness reported by recent ISAAC studies. The latter is in accordance with current research on how and when exposures to environmental agents can induce epigenetic changes that will result in varying biological, clinical and epidemiological expressions of asthma and allergies.14–16
Another most successful task of ISAAC Phase Three was the consolidation of a world research force based on a huge scientific, trained and efficient network, throughout the continents and main regions of the planet and despite the marked differences in cultural and environmental aspects amongst participating countries and centres. Ellwood et al. have found that the majority of centres in this repeat multi-centre international research project undertaken by researchers with diverse cultural backgrounds were able to replicate the methodology between phases (data not shown).
The ISAAC programme has demonstrated that it is feasible to monitor the prevalence and severity of asthma, rhinoconjunctivitis, and eczema in children, globally. It is possible that prevalence of current symptoms of asthma rhinoconjunctivitis and eczema, as well as those factors that could induce changes on it, may behave accordingly to the important environmental and climatic changes presently occurring in the world. ISAAC Phase Three has extended, updated and disseminated valuable epidemiological information on asthma, rhinoconjunctivitis and eczema in childhood, proposing new hypotheses, contrasting old ones and modernising the basis for further aetiological research into the genetic, lifestyle, environmental, clinical and medical-care factors for those diseases.
Ethical disclosureProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Confidentiality of data. The authors declare that no patient data appears in this article.
Conflict of interestThe named authors declare that they have no conflict of interest.
FundingCurrently the main source of funding for the ISAAC International Data Centre (IIDC) is the New Zealand Lottery Board. Many New Zealand funding bodies have contributed support for the IIDC during the periods of fieldwork and data compilation (the Health Research Council of New Zealand, the Asthma and Respiratory Foundation of New Zealand, the Child Health Research Foundation, the Hawke's Bay Medical Research Foundation, the Waikato Medical Research Foundation, Glaxo Wellcome New Zealand, the Auckland Medical Research Foundation and Astra Zeneca New Zealand). Glaxo Wellcome International Medical Affairs supported the regional coordination for Phase Three and the IIDC as well as The BUPA Foundation. Without help from all of the above, ISAAC would not have been such a global success.
All authors participated in the development, design, analysis, and interpretation of this work and in the writing of this paper. We are grateful to the children and parents who participated in ISAAC Phase Three and the coordination and assistance by the school staff is sincerely appreciated. The authors also acknowledge and thank the many funding bodies throughout the world that supported the individual ISAAC centres and collaborators and their meetings.
ISAAC Steering Committee: N Aït-Khaled* (International Union Against Tuberculosis and Lung Disease [The Union], Cheraga, Algeria); HR Anderson (Division of Community Health Sciences, St Georges, University of London, London, UK); MI Asher (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand); R Beasley* (Medical Research Institute of New Zealand, Wellington, New Zealand); B Björkstén* (Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden); B Brunekreef (Institute of Risk Assessment Sciences, Universiteit Utrecht, The Netherlands); J Crane (Wellington Asthma Research Group, Wellington School of Medicine, New Zealand); P Ellwood (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand); C Flohr (St John's Institute of Dermatology, St Thomas’ Hospital, London, UK); S Foliaki* (Centre for Public Health Research, Massey University, Wellington, New Zealand); F Forastiere (Department of Epidemiology, Rome E Health Authority, Rome, Italy); L García-Marcos (Instituto de Salud Respiratoria, Universidad de Murcia, Spain); U Keil* (Institut für Epidemiologie und Sozialmedizin, Universität Münster, Germany); CKW Lai* (Department of Medicine and Therapeutics, The Chinese University of Hong Kong, SAR China); J Mallol* (Department of Pediatric Respiratory Medicine, Hospital CRS El Pino, University of Santiago de Chile, Chile); EA Mitchell (Department of Paediatrics: Child and Youth Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand); S Montefort* (Department of Medicine, University of Malta, Malta), J Odhiambo* (Centre Respiratory Diseases Research Unit, Kenya Medical Research Institute, Nairobi, Kenya); N Pearce (Department of Medical Statistics, Faculty of Epidemiology and Public Health, London School of Hygiene and Tropical Medicine, London, UK); CF Robertson (Murdoch Children's Research Institute, Melbourne, Australia); AW Stewart (Epidemiology and Biostatistics, School of Population Health, The University of Auckland, New Zealand); D Strachan (Division of Community Health Sciences, St Georges, University of London, London, UK); E von Mutius (Dr von Haunerschen Kinderklinik de Universität München, Germany); SK Weiland+ (Institute of Epidemiology, University of Ulm, Germany); G Weinmayr (Institute of Epidemiology, University of Ulm, Germany); H Williams (Centre for Evidence Based Dermatology, Queen's Medical Centre, University Hospital, Nottingham, UK); G Wong (Department of Paediatrics, Prince of Wales Hospital, Hong Kong, SAR China). *Regional Coordinators +Deceased
ISAAC International Data Centre: MI Asher, TO Clayton, P Ellwood, EA Mitchell, E Ellwood. Department of Paediatrics: Child and Youth Health, and AW Stewart, School of Population Health, Faculty of Medical and Health Sciences, The University of Auckland, New Zealand.
ISAAC Phase Three Collaborators: Albania: Prof A Priftanji* (Tiranë); Algeria: Prof B Benhabylès (Wilaya of Algiers); Argentina: Dr CE Baena-Cagnani* (Córdoba), Prof Dr CD Crisci (Rosario City), Dr M Gómez (Salta), Prof GE Zabert (Neuquén); Australia: Prof CF Robertson* (Melbourne); Austria: Assoc Prof G Haidinger* (Kärnten, Urfahr-Umgebung); Barbados: Dr ME Howitt* (Barbados); Belgium: Prof J Weyler (Antwerp); Bolivia: Dr R Pinto-Vargas* (Santa Cruz); Brazil: Dr CdSD Bernhardt (Itajaí), Dr WG Borges (Brasília), Assoc Prof PAM Camargos (Belo Horizonte), Dra MdS Cardoso (Manaus Amazonas), Prof AJLAd Cunha (Nova Iguaçu), Dr GB Fischer (Porto Alegre), Dr JM Motta (Aracaju), Prof FJ Passos (Maceió), Dr AC Pastorino (São Paulo West), Dr AC Porto Neto (Passo Fundo), Prof N Rosário (Curitiba), Assis Prof A Silva (Caruaru), Prof D Solé* (Rural Santa Maria, Santa Maria, São Paulo), Assoc Prof N Wandalsen (Santo Andre), Dr M de Britto (Recife), Assoc Prof L de Freitas Souza (Feira de Santana, Salvador, Vitória da Conquista); Bulgaria: Dr T Popov* (Sofia); Cameroon: Prof C Kuaban* (Yaounde); Canada: Prof A Ferguson (Vancouver), Prof D Rennie (Saskatoon); Channel Islands: Ms R Goulding (Jersey), Dr P Standring (Guernsey); Chile: Dr P Aguilar (South Santiago), Dr L Amarales (Punta Arenas), Dr LAV Benavides (Calama), Dr MA Calvo (Valdivia), Dra A Contreras (Chiloe); China: Prof Y-Z Chen* (Beijing, Tong Zhou), Assis Prof O Kunii (Tibet), Dr Q Li Pan (Wulumuqi), Prof N-S Zhong (Guangzhou); Colombia: Dr G Aristizábal (Bogotá), Dr AM Cepeda (Barranquilla), Dr GA Ordoñez (Cali); Congo: Prof J M’Boussa (Brazzaville); Cook Islands: Dr R Daniel* (Rarotonga); Costa Rica: Dr ME Soto-Quirós* (Costa Rica); Cote d’Ivoire: Dr BN Koffi* (Urban Cote d’Ivoire); Croatia: Dr K Lah Tomulic (Rijeka); Cuba: Dra P Varona Peréz* (La Habana); Ecuador: Dr S Barba* (Quito), Dr C Bustos (Guayaquil); Egypt: Dr ML Naguib (Cairo); El Salvador: Dr M Figueroa Colorado* (San Salvador); Estonia: Dr M-A Riikjärv* (Tallinn); Ethiopia: Assoc Prof K Melaku (Addis Ababa); Fiji: Dr R Sa’aga-Banuve (Suva); Finland: Dr J Pekkanen* (Kuopio County); Former Yugoslav Republic of Macedonia (FYROM): Assoc Prof E Vlaski* (Skopje); Gabon: Dr IE Hypolite* (Port-Gentil); Georgia: Dr M Gotua* (Kutaisi); Germany: Prof Dr U Keil* (Münster); Greece: Assoc Prof J Tsanakas (Thessaloniki); Honduras: Dr A Bueso-Engelhardt* (San Pedro Sula); Hong Kong: Prof YL Lau (Hong Kong), Prof G Wong (Hong Kong); Hungary: Dr Z Novák (Szeged), Dr G Zsigmond* (Svábhegy); India: Prof S Awasthi (Lucknow), Assoc Prof S Bhave (Rasta Peth), Prof J Chhatwal (Ludhiana), Dr NM Hanumante (Pune), Dr KC Jain (Jodhpur), Dr MK Joshi (Mumbai (16)), Dr VA Khatav (Borivali), Prof L Kumar (Chandigarh), Dr SN Mantri (Mumbai (29)), Dr AV Pherwani (Mumbai (18)), Prof S Rego (Bangalore), Prof M Sabir (Bikaner), Dr S Salvi (Nagpur, Pimpri), Dr G Setty (Chennai (3)), Prof SK Sharma (New Delhi (7)), Prof V Singh (Jaipur), Dr TU Sukumaran (Kottayam), Dr PS Suresh Babu (Davangere); Indonesia: Prof Dr CB Kartasasmita (Bandung), Prof P Konthen (Bali), Dr W Suprihati (Semarang); Iran: Dr M-R Masjedi* (Birjand, Rasht, Tehran, Zanjan); Isle of Man: Dr A Steriu (Isle of Man); Italy: Dr L Armenio (Bari), Dr L Bisanti (Milano), Dr E Bonci (Cosenza), Dr E Chellini (Firenze), Dr G Ciccone (Torino), Dr V Dell’Orco (Colleferro-Tivoli), Dr F Forastiere* (Roma), Dr C Galassi (Emilia-Romagna), Dr G Giannella (Mantova), Dr S La Grutta (Palermo), Dr MG Petronio (Empoli), Dr S Piffer (Trento), Dr P Sestini (Siena); Japan: Dr H Odajima (Fukuoka), Prof M Sohei (Tochigi); Jordan: Dr F Abu-Ekteish (Amman); Kenya: Dr FO Esamai (Eldoret), Dr L Ng’ang’a* (Nairobi); Kingdom of Tonga: Dr S Foliaki (Nuku’alofa); Kuwait: Dr JA al-Momen (Kuwait); Kyrgyzstan: Dr C Imanalieva* (Balykchi, Bishkek), Prof S Sulaimanov (Jalalabat); Latvia: Dr V Svabe (Riga); Lithuania: Prof J Bojarskas (Panevezys, Siauliai), Assoc Prof J Kudzyte* (Kaunas); Malaysia: Assoc Prof BS Quah (Kota Bharu), Dr KH Teh (Alor Setar), Assoc Prof J de Bruyne* (Klang Valley); Malta: Prof S Montefort* (Malta); Mexico: Dr M Baeza-Bacab* (Mérida), Dra M Barragán-Meijueiro (Ciudad de México (3)), Dra BE Del-Río-Navarro (Ciudad de México (1)), Dr R García-Almaráz (Ciudad Victoria), Dr SN González-Díaz (Monterrey), Dr FJ Linares-Zapién (Toluca), Dr JV Merida-Palacio (Mexicali Valley), Dra N Ramírez-Chanona (Ciudad de México (4)), Dr S Romero-Tapia (Villahermosa), Prof I Romieu (Cuernavaca); Morocco: Prof Z Bouayad* (Benslimane, Boulmene, Casablanca, Marrakech); Netherlands: Prof R Engels (Netherlands); New Zealand: Prof MI Asher* (Auckland), Dr R MacKay (Nelson), Dr C Moyes (Bay of Plenty), Assoc Prof P Pattemore (Christchurch), Prof N Pearce (Wellington); Nicaragua: Dr JF Sánchez* (Managua); Nigeria: Prof BO Onadeko (Ibadan); Niue: Ms M Magatogia (Niue Island); Nouvelle Caledonie: Dr I Annesi-Maesano (Nouvelle Caledonie); Pakistan: Dr N Mahmood* (Karachi), Dr MO Yusuf (Islamabad); Palestine: Dr N El Sharif* (Ramallah), Mr S Mortaja (North Gaza); Panama: Dr G Cukier* (David-Panamá); Paraguay: Dr JA Guggiari-Chase* (Asunción); Peru: Dr P Chiarella* (Lima); Philippines: Prof F Cua-Lim* (Metro Manila); Poland: Assoc Prof A Brêborowicz (Poznan), Assoc Prof G Lis* (Kraków); Polynesie Francaise: Dr I Annesi-Maesano (Polynesie Francaise); Portugal: Dr ML Chiera (Coimbra), Dra R Câmara (Funchal), Dr JM Lopes dos Santos (Porto), Dr C Nunes (Portimao), Dr J Rosado Pinto* (Lisbon); Republic of Ireland: Prof L Clancy (Republic of Ireland); Republique Democratique du Congo: Prof Dr J-M Kayembe (Kinshasa); Reunion Island: Dr I Annesi-Maesano (Reunion Island); Romania: Prof D Deleanu* (Cluj); Russia: Prof Dr EG Kondiourina (Novosibirsk); République de Guinée: Prof OY Sow (Conakry); Samoa: Ms P Fuimaono V Pisi (Apia); Serbia and Montenegro: Dr O Adzovic (Podgorica), Dr M Hadnadjev (Novi Sad), Dr E Panic (Sombor), Dr S Zivanovic (Nis), Dr Z Zivkovic* (Belgrade); Singapore: Assoc Prof DYT Goh (Singapore); South Africa: Prof K Voyi (Polokwane), Prof HJ Zar* (Cape Town); South Korea: Prof H-B Lee* (Provincial Korea, Seoul); Spain: Dr A Arnedo-Pena (Castellón), Dr J Batlles-Garrido (Almeria), Prof A Blanco-Quirós (Valladolid), Dr RM Busquets (Barcelona), Dr I Carvajal-Urueña (Asturias), Dr G García-Hernández (Madrid), Prof L García-Marcos* (Cartagena), Dr C González Díaz (Bilbao), Prof F Guillén-Grima (Pamplona), Dr A López-Silvarrey Varela (A Coruña), Prof MM Morales Suárez-Varela (Valencia), Prof EG Pérez-Yarza (San Sebastián); Sri Lanka: Dr KD Gunasekera* (Sri Lanka); Sudan: Prof OAA Musa (Khartoum); Sultanate of Oman: Assoc Prof O Al-Rawas* (Al-Khod); Sweden: Dr H Vogt (Linköping); Syrian Arab Republic: Dr S Mohammad* (Tartous), Prof Y Mohammad (Lattakia), Dr K Tabbah (Aleppo); Taiwan: Dr J-L Huang* (Taipei), Dr C-C(Kao (Taoyuan); Thailand: Dr A Kongpanichkul (Nakorn Pathom), Dr R Nettagul (Chiangrai), Dr T Prasarnphanich (Chantaburi), Assoc Prof J Teeratakulpisarn (Khon Kaen), Assoc Prof M Trakultivakorn (Chiang Mai), Dr P Vichyanond* (Bangkok); Togo: Prof O Tidjani (Lome); Tokelau: Dr T Iosefa* (Tokelau); Trinidad and Tobago: Dr MA Monteil (St Augustine, Tobago); Tunisia: Prof M Jerray (Sousse), Prof F Khaldi (Grand Tunis); USA: Prof GJ Redding (Seattle), Dr HH Windom (Sarasota), Dr K Yeatts (Chapel Hill); Ukraine: Assoc Prof V Ognev* (Kharkiv, Rural Kharkiv); United Kingdom: Prof HR Anderson* (North Thames, South Thames), Dr JB Austin (Scotland), Dr M Burr (Wales), Dr MH Shamssain (Sunderland), Prof D Strachan (Surrey/Sussex); Uruguay: Dra D Holgado* (Montevideo), Dra MC Lapides (Paysandú); Venezuela: Dr O Aldrey* (Caracas); Vietnam: Dr B Vaên Cam (Ho Chi Minh City). *National Coordinator
ISAAC Phase Three National Coordinators not identified above: MR Sears (Canada), HR Anderson (Channel Islands), V Aguirre (Chile), J Mallol (Colombia, interim), V Ahel (Croatia), L Waqatakirewa (Fiji), C Gratziou (Greece), CKW Lai (Hong Kong), HR Anderson (Isle of Man), J Shah (India), K Baratawidjaja (Indonesia), S Nishima (Japan), T Fakakovi (Kingdom of Tonga), R Otten (Netherlands), S Barny (Nouvelle Caledonie), R Chansin (Polynesie Francaise), P Manning (Republic of Ireland), JP Okiata (Republique Democratique du Congo), C Catteau (Reunion Island), RM Khaitov (Russia), N Tuuau-Potai (Samoa), B Lee (Singapore), A El Sony (Sudan), L Nilsson (Sweden).