To evaluate the relationship between meteorological factors in North-western Greece and the incidence of bronchiolitis.
MethodsMeteorological data (air temperature and rainfall) for Ioannina city in North-western Greece and medical data from hospitalised patients at University Hospital of Ioannina were collected between January 2002 and December 2013. The association between meteorological factors and rate of hospitalisation due to bronchiolitis was investigated. The data processing was done using the Pearson product-moment correlation coefficient and applying the chi-square test at contingency tables of the parameters.
ResultsOf the 792 hospitalised cases, 670 related to infants (<1 year) and 122 concerned patients aged 1–2 years old. The disease is more common among boys (59.5%) than girls (40.5%). The disease course through the year has a double variation with a main maximum in March and a main minimum in August. The statistical study showed statistically significant correlation of bronchiolitis with: (a) the temperature parameters on an annual basis; (b) precipitation in autumn and dryness in spring; and (c) with sudden changes in diurnal temperature range on an annual basis.
ConclusionA peak incidence of bronchiolitis was noticed in cold and wet seasons during the five days preceding hospitalisation.
Bronchiolitis is an acute inflammatory injury of the bronchioles that is usually caused by a viral infection. Although it may occur in persons of any age, severe symptoms are usually only evident in young infants. Bronchiolitis usually affects children younger than two years, with a peak in infants aged 3–6 months. Most cases of bronchiolitis result from a viral pathogen,1 such as respiratory syncytial virus (RSV:64%), human metapneumovirus (hMPV:9–30%), rhinovirus (RV:16%), parainfluenza virus (HPIV), influenza virus (IV:6%), or adenovirus. Risk factors for the development of bronchiolitis include2: low birth weight, gestational age, lower socioeconomic group, parental smoking, chronic lung disease, neurologic diseases, congenital heart diseases, congenital or acquired immune deficiency diseases, age less than three months and airway anomalies.
Furthermore, the effect between various meteorological variables on the incidence of lower respiratory tract infections has been a matter of investigation for the scientific community for decades.3–5 Many studies have been published exploring the impact of meteorological factors on the incidence of respiratory tract infections (RTI), but there is only limited data comparing the impact of such factors on bronchiolitis specifically.
RSV is the leading cause of bronchiolitis. Our knowledge of how epidemics of RSV are initiated is incomplete. In geographical regions with temperate climates, epidemics of RSV have been reported to peak during winter in both the Northern and Southern Hemispheres.6,7 This suggests that cold weather may increase RSV activity. In contrast, RSV activity has been described as being continuous throughout the year in warm equatorial areas,8,9 suggesting that temperature cannot be the only factor influencing activity of the virus. Recent studies10 suggest that although no clear connections were found between monthly temperatures/precipitation and RSV outbreaks apart from seasonality, a linkage to winter time cold spells was apparent on a daily basis. Unevenly, low minimum temperatures from the day of admittance to 10 days before were interestingly observed.10
Thus the present retrospective study aimed at evaluating the trend of bronchiolitis over an eleven-year period in the Ioannina (Greece) area and detecting a possible relationship with specific meteorological factors, such as air temperature and rainfall. An improved understanding of the relationship between meteorological factors and bronchiolitis may facilitate measures to reduce the incidence of the disease during adverse meteorological conditions.
Patients and methodsSettingUniversity Hospital of Ioannina (UHI) is west Greece's largest health fund and serves as health care provider, supplying most of the health care services within its system. These services include primary, secondary, and tertiary care, as well as pharmacies and paramedical services.
In UHI, children are predominantly treated at community private clinics by board-certified paediatricians.
Ioannina is the capital and largest city of Epirus, an administrative region in north-west Greece. The territory of Ioannina has a population of about 168,000 inhabitants. It lies at an elevation of approximately 500m (1640ft) above sea level on the western shore of lake Pamvotis. It is located 55km (35 miles) east of the port of Igoumenitsa on the Ionian Sea.
Data collectionMedical dataThis retrospective study included medical records from children aged up to two years, admitted to UHI and discharged between January 2002 and December 2013. Children were included if classified by their physician as having an underlying diagnosis of bronchiolitis. Among these children, we analysed acute episodes of bronchiolitis (AEB), presented at the emergency department of the UHI. Patients were managed per the discretion of the attending physician in the emergency department. We obtained the demographic data, the medical history and a detailed history of the current illness.
The distribution of AEB is described by age, sex and seasonality for hospitalisations to describe trends.
Meteorological dataThe meteorological data basis consists of daily values of maximum air temperature (Tmax), minimum air temperature (Tmin) and precipitation (R) for the 11-year period 2002–2013 recorded at the meteorological station of the University of Ioannina. The aforementioned area of Ioannina, has a borderline humid subtropical (Cfa) and Mediterranean climate (Csa) in the Köppen climate classification, since only two summer months have fewer than 40 millimetres (1.6in) of rainfall, preventing it from being classified as solely humid subtropical or Mediterranean. Summers are typically hot and moderately dry, while winters are wet and colder than on the coast with frequent frosts and occasional snowfall.11 Ioannina is one of the wettest cities in Greece with a total annual precipitation of approximately 1100mm. From the above parameters, mean daily temperature Tmean=(Tmax+Tmin)/2 and diurnal temperature range (Trange=Tmax−Tmin) were calculated. Also, the day-to-day changes of the above temperature parameters (Tmax, Tmin, Tmean and Trange) were calculated. Since the incubation time of the respiratory viruses ranges from one to five days, with a mean period of three days, the mean values of the four temperature parameters and their maximum (absolute) changes (Differences) (DTmax+, DTmin+, DTmean+, DTrange+, DTmax−, DTmin−, DTmean−, DTrange−) during the five days preceding hospitalisation were used in the analysis. Furthermore, precipitation was calculated for 10-day intervals before the admissions as too many of the five-day intervals were completely dry.
At first, the five-day values of all the parameters were distributed in quintiles (20% intervals) and the corresponding histograms were constructed. Subsequently, for a quantitative assessment of the connection between the admissions and the meteorological parameters, for each quintile, the number of days with none, one, two and more than two AEB cases was estimated and a contingency table was constructed for each parameter. Chi-square (χ2) test was applied on each contingency table in order to investigate the statistical significance of the relation between the sampling distributions.
Statistical analysisAt first, Pearson correlation coefficients between the seasonal and annual number of AEB and the corresponding seasonal and annual values of the various meteorological parameters were calculated. Then, chi-square test was applied on contingency tables constructed for five classes of the values of the meteorological parameters.
ResultsIncidence per age and sexDuring the study period, there were 792 hospitalisations for bronchiolitis in UHI.
Patients <1 year old accounted for 84.6% of the total number of hospitalisations for bronchiolitis, 15.5% of these being >1 year of age. A total of 59.5% of the hospitalisations were by males and 40.5% by females.
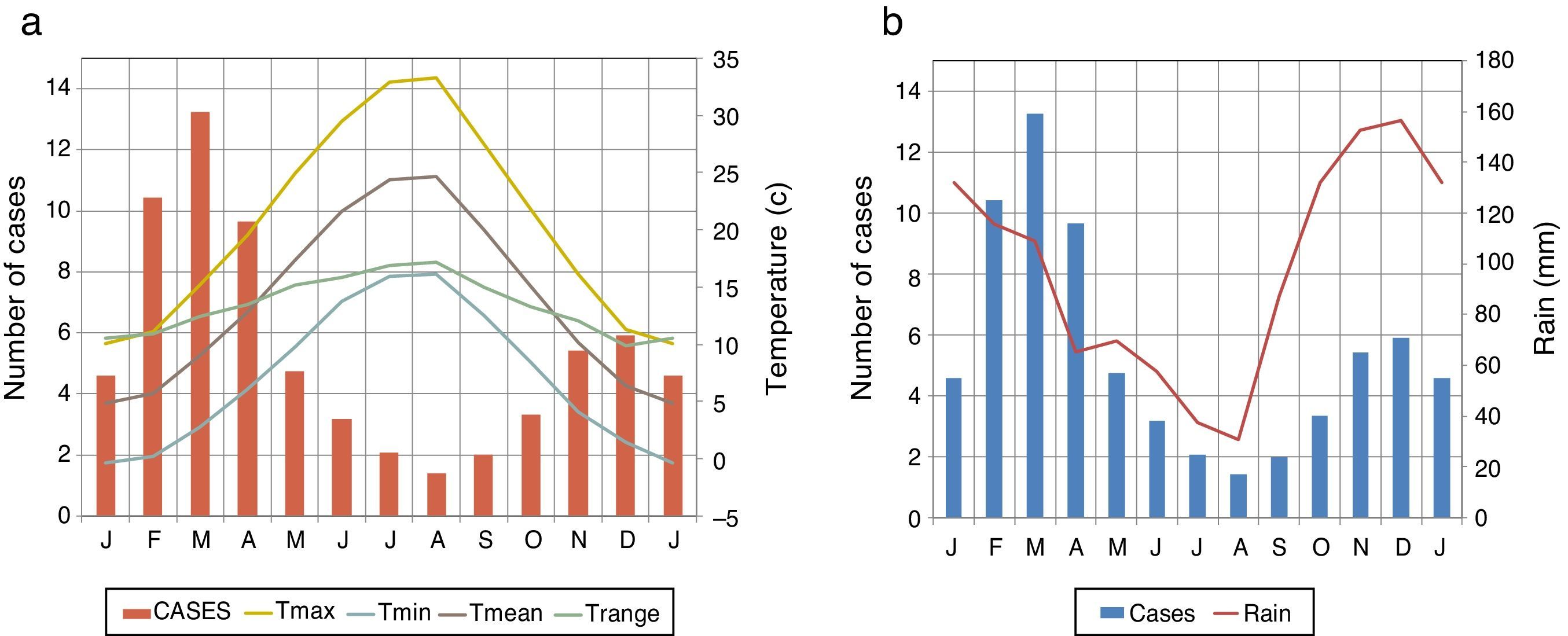
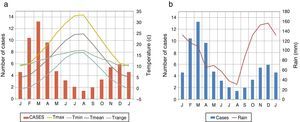
SeasonalityThe hospitalisation rate for AEB varied through the year. The largest numbers of admissions were recorded in March (20%), followed by February (15.6%) and the fewest in August (1.9%). The mean number of cases/day raised from 0.04/day in August to a maximum of 0.47/day in March. The mean frequency was 0.18 AEB admissions per day on annual basis. The month to month intra-annual variation of AEB along with the meteorological parameters is presented in Fig. 1. It is seen that all temperature parameters present maxima in July−August and minima in January, while precipitation is maximum in November−December and minimum in August. The variation of AEB generally resembles that of precipitation, while it appears to be the opposite to those of the temperature parameters.
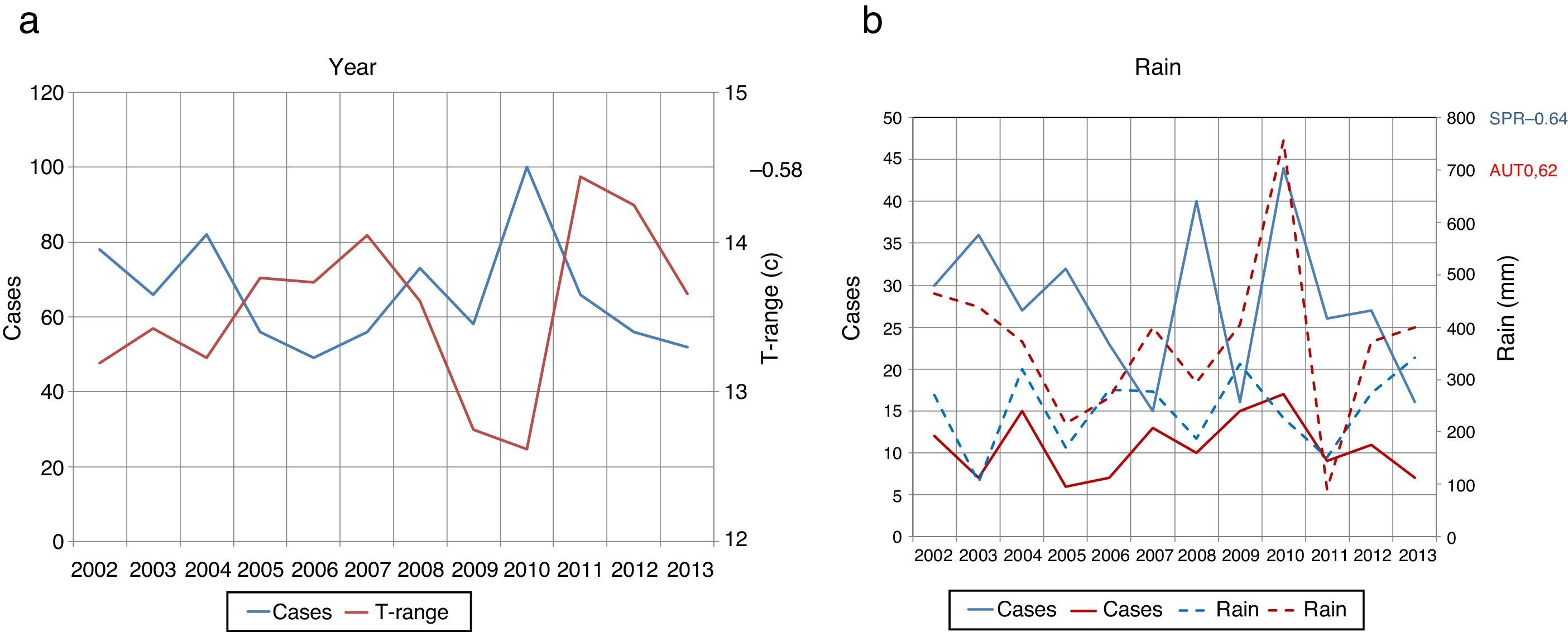
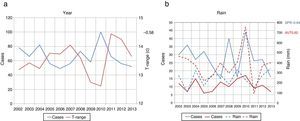
Inter-annual variationPearson correlations coefficients were calculated between the 12-year time series on seasonal and annual basis and statistically significant values at 95% confidence level (|r|>0.57) were found for three cases only:
- (a)
Diurnal temperature range is anti-correlated with admissions (r=−0.58) on a yearly basis (Fig. 2a), i.e. AEB are more frequent during years with low Trange. Low Trange is usually a result of more cloudy than average weather conditions.
- (b)
Autumn precipitation is positively correlated with admissions (r=0.62) (Fig. 2b), indicating high AEB number during wet autumns.
- (c)
Spring precipitation is negatively correlated with admissions (r=−0.64) (Fig. 2b); i.e. dry springs are associated with high admission numbers. Lack of precipitation during spring favours high pollen concentration in the atmosphere, because of the absence of wet deposition.
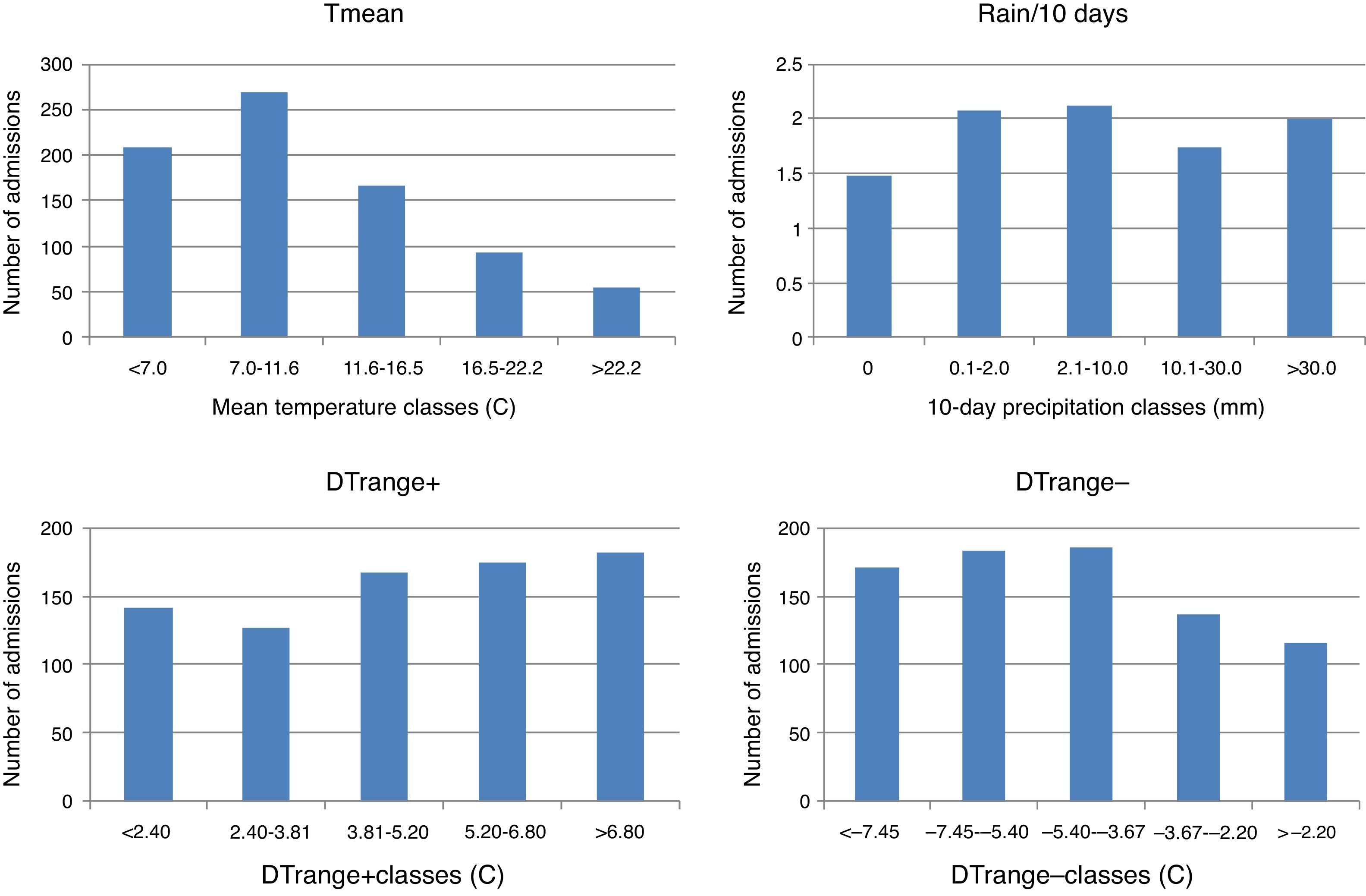
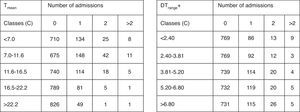
The constructed histograms (Tmean, R, DTrange+, DTrange−) representing the five-day values of the parameters (10-day for precipitation) are presented in Fig. 3. A general inspection of the histograms shows that all parameters except rainfall seem to be connected to AEB admissions. For example, admissions appear to be lower after high temperature periods. However, the extreme day-to-day changes of Trange appear to favour the admissions.
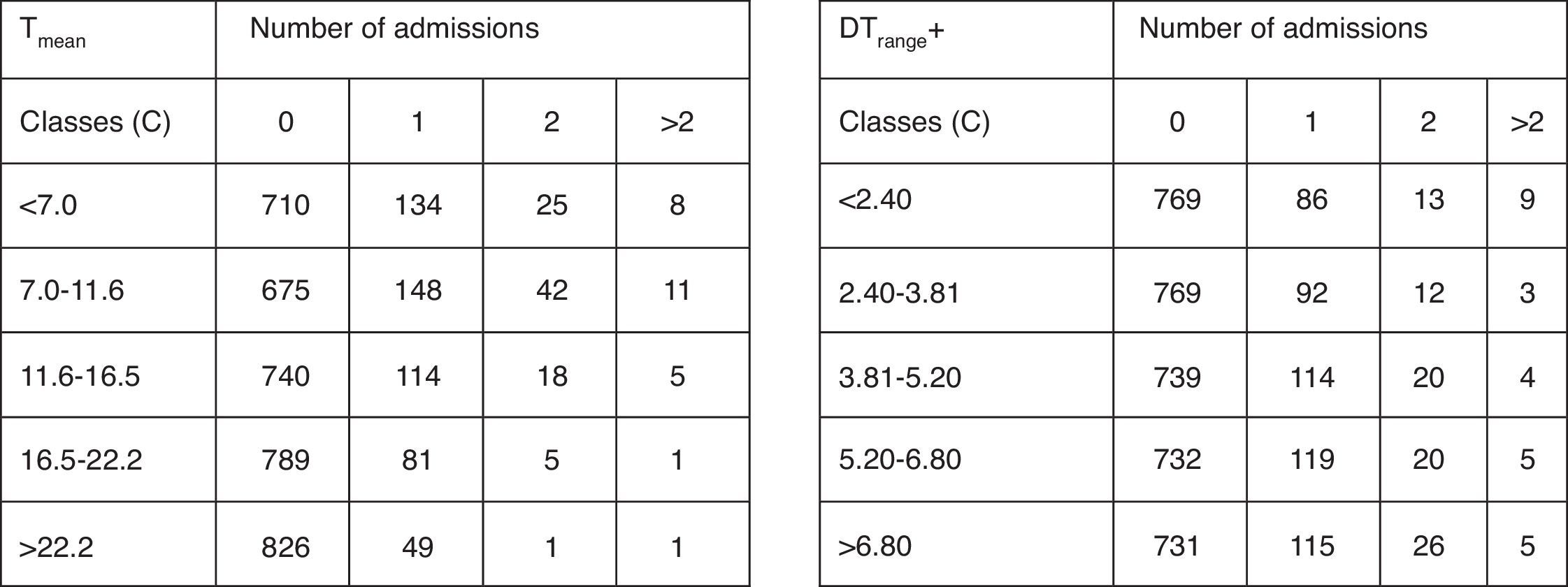
Regarding the quantitative assessment of the connection between admissions and the meteorological parameters, the results are presented in Fig. 4. There is a statistically significant (95% confidence level) relationship between the frequency of admissions and Tmax, Tmin, Tmean, Trange, DTrange+ and DTrange−. In Fig. 4, the contingency tables of Tmean and DTrange+ are presented as an example.
DiscussionThis is a retrospective study, conducted to analyse the relationship between meteorological parameters for 11 years and bronchiolitis, the most common RTI in infancy. Bronchiolitis is an acute inflammatory injury of the bronchioles that is usually caused by a viral infection in infants younger than two years and is a major cause of hospitalisations around the world.12 It might be associated with multiple external factors. Meteorological parameters have been found to be one of the most critical determinants in bronchiolitis.13
The effect of temperature level on the incidence of bronchiolitis has been reviewed in the past. Sirimi et al., in a recent retrospective analysis,14 reviewed the correlation between RSV epidemic activity with climate parameters. The peak monthly RSV incidence was observed during February with a mean temperature 10.34°C. A study by Chen et al.15 mentioned that most viruses responsible for bronchiolitis exhibited strong seasonal patterns, with the number of RSV, hMPV, and IV cases peaking during the winter and spring seasons. In the same line, our study cases showed higher incidence in months with low temperatures. The largest numbers of admissions were recorded in late winter and early spring. At this period of time, in the Ioannina area, cold leads to increased incidence of bronchiolitis. The direct effects of cold to viability and the transmissibility of various types of viruses may affect the respiratory tree. During periods with cold temperature, the culpable viruses are more stable in secretions by which they are transmitted. Furthermore, during cold weather people usually stay indoors, where viruses spread more readily.15 Additionally, Peynter reported that the cold, dry conditions of temperate winters appear to encourage the transmission of RSV and influenza virus, by increasing influenza virus survival in aerosols, and increasing influenza and RSV survival on surfaces.16
The correlation of bronchiolitis with precipitation has been a matter of study in the literature. Increased numbers of children with RSV bronchiolitis have been associated with higher relative humidity,4,14,17,18 lower relative humidity8,19 or relative humidity of 45–65%.20,21 Likewise, our study revealed that autumn precipitation is positively correlated with admissions, indicating high AEB number during wet autumns while spring precipitation is negatively correlated with admissions. In the same line, in a retrospective study form Italy which investigated the emergency calls for asthma exacerbation in children, two main peaks were evident: the most relevant during the autumn, and the second during the spring22; the latter one being in contradiction to our results. Potentially important keys to understanding the nature of these relationships are present in laboratory studies of the stability of RSV, which is the main causative agent of bronchiolitis.21
Furthermore, as is known, RSV is believed to be transmitted by large-particle aerosols and by direct contact with RSV in solutions of human secretions.23 Hence, the hot, wet conditions of tropical rainy seasons appear to discourage aerosol transmission of influenza, by reducing the amount of influenza virus that is aerosolised, and probably also by reducing influenza survival in aerosol.24 The wet conditions of tropical rainy seasons may, however, encourage contact transmission of influenza and RSV viruses, by increasing the amount of virus that is deposited on surfaces, and by increasing virus survival in droplets on surfaces.23 This evidence suggests that the increased incidence of influenza and RSV in tropical rainy seasons may be due to increased contact transmission. This hypothesis is consistent with the observation that tropical rainy seasons appear to encourage the transmission of RSV more than influenza.16 Generally speaking, respiratory pathogens have a different affinity to certain climatic conditions.4 Rhinovirus preferred a humid climate, whereas many other respiratory pathogens, such as RSV and influenza A, favoured low temperatures, explaining the peak incidence of bronchiolitis in cold seasons, at least in a temperate climate, as that of Ioannina. Thus, taking into account all the results of the aforementioned studies, which are comparable to ours, the synergy of both lower temperatures and a higher number of rainy days are associated with increasing frequencies of RTI, including bronchiolitis.
Several studies have examined the associations between diurnal temperature range (DTR) and the morbidity of respiratory diseases in children and the results were conflicting with each other. The study conducted in four metropolitan areas in Korea25 and the study conducted in Brisbane, Australia26 supported a positive association between DTR and asthma hospital admissions. On the other hand, a study conducted in Detroit, Michigan27 described that a greater 24-hour temperature change decreased the risk of asthma-related emergency department visits among children. Plausible biological mechanisms of DTR on respiratory diseases have been hypothesised. It was postulated that short-term temperature variation causes a mild inflammatory reaction and thereby causes airway narrowing which increases the risk of susceptibility to respiratory diseases. Sudden temperature changes caused more inflammatory nasal responses in an allergic rhinitis group,28 which may explain some of the mechanisms associated with the effects of DTR on asthma admissions. However, in our study we noticed that DTR is negatively correlated with bronchiolitis admissions (r=−0.58) on a yearly basis. This is possibly due to the fact that low temperature range is a result of either high wind speed or high cloud cover.29 Both may be responsible for high admission numbers, as wind may lead to high concentration of suspended particles, while cloudiness is usually combined with high relative humidity favouring fungus growth.
Finally, the correlation of bronchiolitis with changes of temperature parameters during the days preceding hospitalisation has been reviewed in the past. In a recent retrospective study,30 significant correlation was mentioned between the incidence of RSV infections and the mean minimum temperature registered during the same week and the previous weeks. Likewise, a Portuguese analysis of the influence of meteorological conditions on RSV10 mentioned that although no clear connections were found between monthly temperatures/precipitation and RSV outbreaks apart from seasonality, a linkage to wintertime cold spells is apparent on a daily basis. Inconsistently, low minimum temperatures were observed from the day of admittance back to 10 days before. As presumed, the incubation time of the respiratory viruses ranges from 1 to 5 days with a mean period of three days.31 In addition, our study mentioned a correlation of bronchiolitis incidence with changes of temperature parameters during the five days preceding hospitalisation. The results confirm the influence of air temperature and extreme day-to-day changes (increase and decrease) of Trange to the frequency of admissions.
Several studies have been performed so far to investigate the possible relationship between meteorological factors and respiratory tract infections, specifically asthma. To the best of our knowledge, there are only limited reports regarding the influence of meteorological parameters on bronchiolitis. Therefore, considering all these aspects, the present study has some limitations. We have not detected the bronchiolitis pathogens and their seasonality, including the effects of meteorological conditions on the survival and spread of infectious pathogens in the environment, as the frail association between viral acute respiratory tract infections and temperature/precipitation has already been supported by other studies.10,32
In conclusion, the data generated from this retrospective study revealed the meteorological factors that may affect bronchiolitis incidence in one of the wettest regions of Greece during a long observation period of 11 years. In particular, a significant correlation of bronchiolitis was noticed with (a) the low temperature on an intra-annual basis and (b) high autumn precipitation and low spring precipitation.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Conflicts of interestThe authors declare no conflicts of interest.