INTRODUCTION
Fixed drug eruptions are characterized by solitary or multiple red macules o plaques that are often tender and occur in the same place each time that a particular medication is administered. The erythematous and oedematous well-defined plaques may be one to many centimeters in size. Recurrence in the same location is the key to diagnosis. The face, the gland penis, the neck and the sacral region are commonly affected but any location is possible. Often, but not always, leaves an area of hyperpigmentation in the affected place during spontaneous resolution. Very rarely blisters centrally.
The drugs that are common causes of fixed drug eruptions are: ampicillin, aspirin, barbiturates, metronidazole, nonsteroidal antiinflammatory drugs, oral contraconceptives, phenolphtalein, sulfonamides and tetracyclines. Although antihistamines like cetirizine, dimenhydrinate, hydroxyzine and astemizole exceptionally provoke cutaneous side effects there is only one previous report about loratadine inducing the same fixed drug reaction as we are presenting now1-5.
CASE REPORT
A 8-years-old boy suffering perennial allergic rhinitis and bronchial asthma with familiar atopic background and a serum IgE level ≥1000 KU/L was receiving pharmacological support with β2-agonists and inhaled corticosteroids as well as specific immunotheraphy with the house-dust mite Dermatophagoides pteronyssinus in increasing doses during the last year. In occasion of a exacerbation of his atopic condition the boy received one tablet of loratadine 10 mg to relief his nasal symptoms.
When he came the next week for the shot-session his mother referred that in the right elbow the boy suffered a well-defined erythematous and oedematous plaque that was attributed to a exogenous noxa (trauma or pressure). As this skin lesion vanished without treatment the episode remained underdiagnosed. One month later the boy received again a single dose of loratadine 10 mg and 48 hs later he repeated the same pruriginous patch of size 5 x 5 cms at the same location as before (fig. 1).
Figure 1.--Macroscopic appearance of the fixed eruption in the skin of the right elbow.
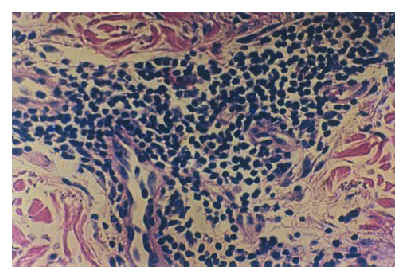
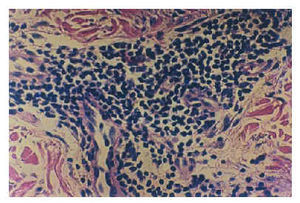
Figure 2.--Histopathologic appearance of the skin of the elbow showing a large lymphomonocytic infiltrate in the superficial dermis (24 h after loratidin intake) (HE, X100).
With the suspicion of a fixed drug eruption these methods were applied to clarify the condition: 1) patch-tests with loratadine, lactose and magnesium stearate 10 % each; 2) the UBCT (Ultra-Brief-Challenge-Test) which is our modification of the classical peroral provocation test published elsewhere with loratadine (10 mg), cetirizine (10 mg), ebastine (10 mg) and excipients suitably distributed in 4 sessions and 3) a skin biopsy from the plaque performed as routinely histopathological studies stained with hematoxilin-eosin6.
Results with these methods revealed that patch-tests were consistently negative with all the antihistamines after 48 and 96 hs; the UBCT demonstrated that only the ingestion of loratadine was able to reproduce in the right elbow the erythematous and oedematous skin lesion after 8 hs. On the other hand, the skin biopsy showed a hydropic degeneration of the basal cell layer, a important perivascular and disseminated lymphomonocytic infiltrates without the presence of metachromatic cells when it was stained with toluidin blue 1 %. As we know very little about the immunoreactivity of the metabolites of loratadine and that these low-molecular-weight molecules may not be the allergen itself we decided not to perform the conventional prick or intradermal skin tests with the drug.
CONCLUSIONS
We pressume that this is the second report about the relation between the oral ingestion of loratadine and the production of a typical fixed drug eruption.
Our findings reinforce the idea that this skin pathology has no limits in its appearance independently of age, gender and drug.
Also, the methods to assure the final diagnosis sustained that this fixed eruption were closely related to a skillful clinical record to detect the suspected drug and to the peroral provocation test to reproduce the lesion.