Asthma is the most common chronic disease in chidhood 1-6 . In Brazil, asthma prevalence ranges between 4.7 % and 20.7 % in schoolchildren with ages from 6 to 7 years and between 4.8 % and 21.9 % for those aged 13 and 14 years 7 . In Duque de Caxias, a Rio de Janeiro County, asthma prevalence was found to be 27.7 % and 19 % in schoolchildren with ages ranging between 6 and 7 years and 13 and 14 years, respectively 8 .
Because of asthma high morbidity, several instruments and methodologies have been developed and tested aiming the detection of asthmatic individuals. The use of a questionnaire (QES) focusing, basically, on the referred symptoms has proven to be a promising and very valuable tool 9 .
Halls et al 10 used a QES 6 designed for children and adolescents, aiming the early detection of asthmatic cases. Its main advantages were: simplicity (only 4 questions to ask), in addition to the fact that it can be applied to a wide age range. In Brazil, there are few studies following this line of investigation, and the questionnaire of the International Study of Asthma and Allergies in Childhood (ISAAC) 6 is still the most used for the determination of asthma prevalence among schoolchildren. The aim of this study was to determine the diagnostic accuracy of a brief questionnaire (BQ) as a screening test for asthma in children and adolescents.
MATERIAL AND METHODS
Design of the studyA cross-sectional study, with prospective data collection was performed.
SettingsThe study was carried out in Ismélia da Silveira Children’s Hospital (ISCH), in Duque de Caxias County, Rio de Janeiro State, with a population of 775,456, of whom 99 % inhabit the urban area 11 . In 2002, based on hospital records, 128,121 children received medical care in the emergency department, with monthly and daily averages of 10,677 and 356 respectively.
Target population and sampleThe study target population were schoolchildren aged 5 to 15 years, living in Duque de Caxias. The sample consisted of the first eight patients, who come daily for medical treatment in the emergency department, accompanied by a parent or guardian, fulfilling eligibility criteria, and consenting to participate in the research.
Eligibility CriteriaChildren and adolescents with ages ranging from 5 to 15 years, who spontaneously sought the hospital emergency department for medical assistance, were included. Patients with a severe clinical condition that demanded emergency care or hospitalization; patients with clinical conditions that make difficult to carry out the measurement of the forced expiratory volume in the first second (FEV1) due to lack of cooperation; patients with a clinical-radiologi-cal condition of acute infection of the lower respiratory tract and; patients using medications that could adversely affect the exam, were excluded 12 .
Sample sizeSample size was calculated with asthma as the principal variable of interest. Considering that in Brazil the estimate prevalence of asthma in childhood and adolescence ranges between 15 % and 20 % 1 , our calculations were based on an expected frequency of 20 % of patients, with a ± 6 % margin of error (14 %26 %) and a 95 % confidence interval (CI). We found a sample size of 171 individuals.
Table I Brief Questionnaire (BQ) originated from ISAAC 6 and Halls et al 10 QES.
Data collection
The basis for the data collection instrument was the QES used by Halls et al 10 (table I). Translation into Portuguese was made by the author herself. Adaptations were required, such as: a) the addition of a Brazilian term similar to wheezing , usually referred by responsible and patients, themselves b) question n.º 1 from the original BQ about wheezing occurrence in the last 12 months was replaced by a similar one from the ISAAC QES, validated for Brazilian children by Solé et al 13 .
Study definitionsAsthma was defined as the occurrence of a minimal increment of 12 % in the FEV1 in relation to the initial base value after the use of a short acting bronchodilator 14 .
The four questions of the BQ (table I) aimed to get information about asthma from those responsible (parents or guardians) for children and adolescents, involving specific symptoms, such as: wheezing in the 12 months prior to the research; nocturnal coughing; coughing or difficulty of breathing during physical activities; persistent coughing for over 10 days.
Question n.º 1 “ Has your child ever had wheezing or whistling in the chest in the last 12 months? ” limits the period of time to 12 months in order to reduce the possibility of recall errors and are not dependent on seasonality. There is also no mention of the terms, crisis of wheezing to allow the detection of a greater number of patients with persistent symptoms, who could be excluded by using words as: crises, attacks or episodes .
Question n.º 2 “Has your child awakened at night because of coughing in the last 12 months? ” refers to nocturnal coughing, broadly accepted as an alternative asthma presentation 15 .
Question n.º 3 “Has your child had coughing, wheezing or shortness of breath with exercise or ac tivity and had to stop because of this symptoms at any time in the last 12 months? ” tries to identify individuals who present exercise induced bronchospasm.
Question n.º 4, “When your child has a cold, does the cough usually last more than 10 days?” aims the inclusion of children and adolescents who maintain persistent coughing, beyond the established limit for an acute respiratory infection without further complications.
The authors used two criteria to measure the sensitivity and specificity of the BQ. Criterion 1 considered the screening test to be positive when there was at least one affirmative response to any one of the 4 questions. Criterion 2 used a positive answer to question n 0 .1 to discriminate the asthmatic group from the other.
The sample was categorized by family income and educational level of the family provider according to the Brazilian Economic Classification Criteria 16 .
Screening ProcedureResearch lasted 5 weeks, beginning in June 2003. The first eight patients who arrived, consecutively, in the emergency department, from Monday to Friday, in the period 07:00-12:00, answered the BQ questions (table I), interviewed by the author, after obtaining informed consent. Weight and height were determined in accordance with standard patterns 17 and then FEV1 was measured, using the Micro Medical, Kent, UK, portable spirometer, following the American Thoracic Society 14 guidelines and the Brazilian Spirometry Consensus 12 . After FEV1 measurement, four puffs of salbutamol spray (100 mcg/dose) were administered by inhalation using a Flumax ® (600 ml) spacer connected to the dose-metered inhaler (MDI). After 15 minutes, the FEV1 was again determined 12 .
Quality controlA pilot study was conducted to test data collection dynamics; performance of the FEV1; patients flow, and to make the necessary adjustments and changes. Routinely, before starting the daily series of exams, spirometer calibration was checked using high and low flows with a 3-litre syringe 12 . All FEV1 measurements were performed by the same technician, with proven experience in the procedure. Collected data were stored in a double entry databank in an independent manner.
Statistical analysisVariables were described with frequency distribution for the categorical ones and with mean and standard deviation (SD) for the numeric ones. It were determined: sensitivity (Sens), specificity (Spec), positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR) and accuracy (A) 18 . As an exploratory way, odds ratio (OR) 18 was employed as a measurement of association between the outcome variables ( asthma and non-asth-ma ) and the independent variables, with results being presented with their respective 95 % confidence intervals (95 % CI) 19,20 . For statistical inference, < 0.05 was chosen as a value of significance. Statistical analysis was performed using: Statistical Package for the Social Sciences ( SPSS ), version 10.0 for Windows21 and Confidence Interval Analysis (CIA) version 2.0 22 softwares.
Ethical questionsThe study was approved by the Committee of Medical Ethics of Rio de Janeiro County Health Secretary. Informed consent from the person responsible for the patient was obtained prior to begin the interview.
RESULTSEvaluation included 226 children and adolescents with ages ranging from 5 to 15 years. From those 15 patients of 5 years old were excluded for not being able to perform the VEF1 assessment leading to a sample of 211 patients.
Table II describes the distribution of patients by: gender, age e annual family income.
It was observed that in 178 (84,40 %) cases it was the parents themselves, who had taken the child or adolescent to the emergency department for medical care. They were, in average ( ± SD), 36,33 (8,37) years old. The age distribution showed that 46 (21,80 %) adults belonged to the group of patients with ages ranging from 19 to 29 years, 147 (69,60 %) with ages from 30 to 49 years and 18 (8,60 %) with ages equal to 50 years or more.
The FEV1 assessment, identified 47 (22,27 %) asthmatic and 164 (77,73 %) non asthmatic patients. In average ( ± SD) the FEV1 increment observed after bronchodilatation test was 26,48 % (14,58) among asthmatics and 4,60 % (3,14) among non asthmatics.
The FEV1 mean values ( ± SD) related to pre/pos bronchodilatation test were: 0,98L (0,46)/1,21L (0,53) in the asthmatic and 1,57L (0,53)/1,63L (0,54) in the non asthmatic group, respectively.
Table III shows the sensitivity, specificity, positive predicted value, negative predicted value, positive likelihood ratio and OR, with their respective 95 %CI, related to the positive answers to the four questions of the BQ, individually or in combination.
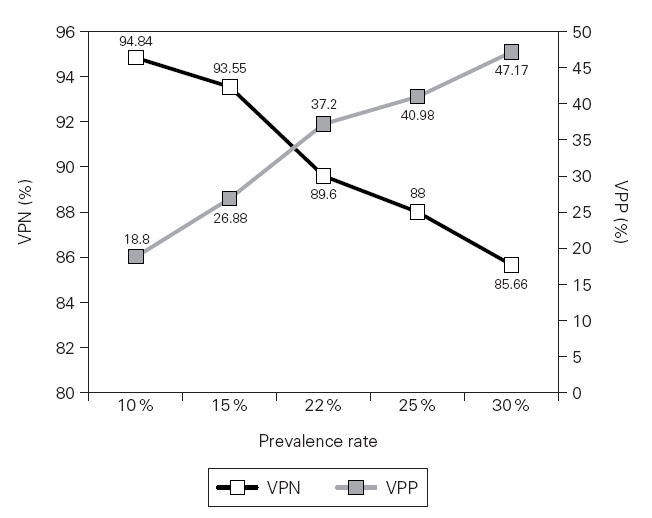
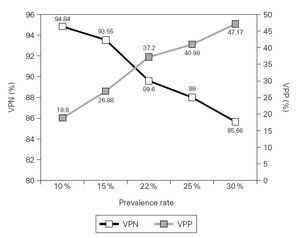
Figure 1 shows the PPV and NPV values obtained from hypothetical examples in which asthma prevalence rates range from 10 % to 30 %.
DISCUSSIONThe difficulty in a precise asthma definition has been highly discussed in the medical literature 23-25 .
Table II Sample distribution (n =211) by: gender, age, annual family income and education level. Hospital Infantil Ismélia da Silveira. Duque de Caxias County, Rio de Janeiro State/Brazil (2003)
Table III Sensitivity (Sens), Specificity (Spec), Positive Predicted Value (PPV), Negative Predicted Value (NPV), Positive Likelihood Ratio (PLR), Accuracy (A), Odds Ratio (OR) and their respective 95 %Confidence Intervals (95 %CI), considering affirmative answers to the four questions, individually or combined, as positive results for screening asthma
The lack of a gold standard for asthma means that no single measurement is capable of reliable information. FEV1, if considered solely, has been indicated as the best measurement of pulmonary function, to establish the disease severity 26-28 . It is a useful index of airway obstruction, that can be obtained with simple portable instruments, a choice favoured in diagnostic procedures 28 . Although limited, FEV1 measurement with bronchodilatation test seemed to us the complementary exam that best fitted the proposed objectives and the information so made available would be capable enough to identify populations with different disease rates.
Analysing BQ performance, we can identify high values of sensitivity when both criteria were used. A screening tool should be able to identify as many true positives as possible and to reduce the number of false negatives. Criterion 2, although showing a lower sensitivity (75 %) than the criterion 1 (83 %), seems to be more advantageous as a tool for screening asthmatic patients, due to its higher specificity (64 %).Therefore we propose that the use of only one question would be simpler and more convenient than the use of the full set of four questions, allowing to make a rapid determination of whether to proceed a more detailed investigation to confirm the initial diagnosis. Asymptomatic patients are not the target of specific therapeutic interventions with prophylactic medications. Thus, question n.º 1, that approaches wheezing in the last 12 months , can both identify one of the most common asthma manifestations and, at the same time, assure the recent temporality of the symptoms, which are requirements for the identification of the group that will need further medical assistance.
Compared to our results, Halls et al 10 , using a similar BQ, found similar sensitivity value (73 %) and higher specificity value (83 %) for wheezing in the last 12 months , in the group without previous asthma diagnosis. On the other hand, Wolf et al 29 , using a 5-question BQ which also approached the occurrence of wheezing in the last 12 months in a group of Chicago schoolchildren, found lower sensitivity value (65 %) and higher specificity value (88 %). These three groups, besides differing from the characteristics of the selected populations and the type of the study design, may also have showed distinct results just because of different comprehensions of the meaning of the word wheezing . Further, it is recognized that the reference of symptoms based on reports provided by parents or guardians is subjective, as they are not always capable of noticing the respiratory symptoms their children really present 29 . Their answers may suffer the influence of a variety of cultural, social and psychological factors 30 . So, it is possible that some classifications, based on the presence of wheezing , may have resulted from a misunderstanding by the parents or guardians about this matter. This assumption is reinforced by the fact that the sample was constituted essentially of low educational level individuals, with less than four school years of attendance.
It is probable that some mild cases of asthma presented normal spirometric values, and, for this very reason, were then classified as non-asthmatic. Nevertheless, we believe that the false negative rate was low because patients should have some degree of bronchial hyperreactivity (BHR), once they had sought medical assistance for their respiratory symptoms of variable severity. Although the bronchoprovocation test is a useful test to characterise BHR, it was not possible to include it in the study be-cause of possible risk complications. Besides, patients found to be without respiratory symptoms but who sought the emergency department presenting other symptoms, could not show BHR both for being under clinical control and because the limitations inherent to the test itself 23,31 .
The correct interpretation of the test result is closely linked to the a priori estimates of the probability of the disease. Thus, the calculations of the positive and negative predictive values for any test or procedure, whose sensitivity and specificity are known, may help to show when the test will be more useful, according to the influence of different prevalence rates, as exemplified in figure 1. We verified that NPV remained high, even in situations of lower prevalence rate (10 %). In this circumstance, the occurrence of a negative result for question n.º 1 will tend to exclude the disease in 96 % of the cases, whereas a positive result for this question will not be particularly useful in confirming asthma.
This research has some limitations. It is a descriptive study, justifiable in the current state of knowledge, because it brings data for subsequent researches in Brazil. The asthma prevalence rate may be greater than would be expected because the investigation was performed in a health service unit, reflecting a possible sampling bias, due to selection of only the individuals who sought for medical care. Also, it was not possible to include children less than 5 years old as it would be difficult of performing the FEV1 measurement in this age range.
In conclusion, we have showed that the BQ is quick and inexpensive to administer, convenient both to doctors and to patients and easy to implant for asthma screening at the emergency department. The use of only one question seems to be more advantageous because of the possibility of excluding asthma diagnosis in a more simplified way and with an accuracy of 66 %. NPV remained elevated in high and low risk populations, showing that the absence of wheezing in the last 12 months means, very likely, that the child or adolescent is not asthmatic.
Figure 1.—Hypothetical examples of asthma prevalence rates ranging from 10 % to 30 % and their related positive and negative predicted values when considering an affirmative answer to question n.º 1 as a positive screening test.
The BQ may be a useful tool for the general practitioner at the primary attention level, where a positive test will require additional investigation to confirm the diagnosis and the severity degree. Such approach would allow that patients receive appropriate treatment, assuring a clinical control of the disease and, consequently, reducing the number of visits to the emergency department.
We believe that the information made available as a result of this research may help future health service policies, contributing to improve the medical assistance quality provided to the children and adolescents in the Duque de Caxias County, Rio de Janeiro, Brazil.
Correspondence:
M.A. Rocha Crispino SantosRua Gurindiba, 76/303. Cep 20530-580 Rio de Janeiro. Brasil E-mail: marilenecs@terra.com.br