The standard treatment for metastatic hormone-sensitive prostate cancer (mHSPC) is now a combination of androgen deprivation therapy plus an androgen receptor-targeted therapy (abiraterone, apalutamide, enzalutamide or darolutamide), with or without chemotherapy (docetaxel). The selection of suitable patients for each therapeutic approach has become a determining factor to ensure efficacy and minimize side effects. This article combines recent clinical evidence with the accumulated experience of experts in medical oncology, radiation oncology and urology, to provide a comprehensive view and therapeutic recommendations for mHSPC.
El tratamiento estándar del carcinoma de próstata hormonosensible metastásico (CPHSm) es en la actualidad una combinación de terapia de privación androgénica más una terapia dirigida al receptor androgénico (abiraterona, apalutamida, enzalutamida o darolutamida) con o sin quimioterapia (docetaxel). La selección de pacientes adecuados para cada enfoque terapéutico se ha convertido en un factor determinante para garantizar la eficacia y minimizar los efectos secundarios. Este artículo combina la evidencia clínica reciente con la experiencia acumulada de expertos en oncología médica, oncología radioterápica y urología, para proporcionar una visión integral y recomendaciones terapéuticas para el manejo del CPHSm.
Treatment for metastatic hormone-sensitive prostate cancer (mHSPC) consists of androgen deprivation therapy (ADT) plus an androgen receptor-targeted therapy (abiraterone, apalutamide, enzalutamide or darolutamide), with or without the addition of docetaxel and/or locoregional radiotherapy in selected patients.
Randomized trials demonstrate improvements in overall survival (OS) with doublet therapy (ADT plus androgen receptor pathway inhibitor [ARPI]) and with triplet therapy, adding docetaxel. Doublet therapy is compared with ADT and triplet therapy is compared with docetaxel+ADT.1–7 However, there are no comparative studies of triplet vs. doublet therapy, so the choice between them should be made according to the characteristics of the patient and the clinical-molecular features of the neoplasm.
This article aims to provide therapeutic recommendations in mHSPC based on clinical evidence and therapeutic guidelines as well as the opinion of experts in medical oncology, radiation oncology and urology,
The role of local treatment in patients with mHSPCAccording to different subgroup analyses in large, randomized trials and retrospective analyses, local treatment of the primary tumor in the face of metastatic disease would have an impact on survival,8–13 mainly in those patients classified as oligometastatic.
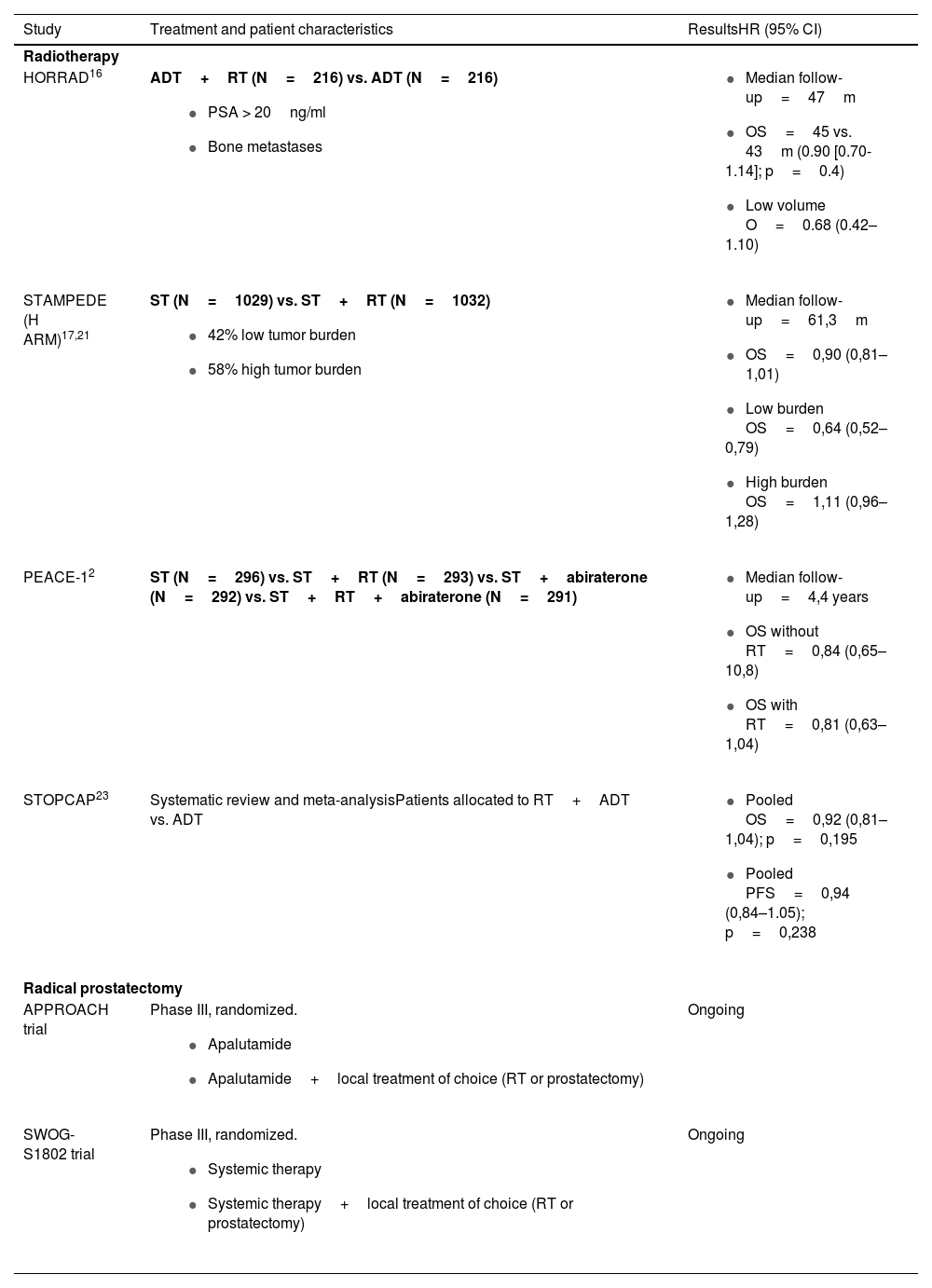
The role of local treatment of the primary tumor in mHSPCIn metastatic disease, local treatment of the primary tumor has a biological rationale, by decreasing the total tumor burden and inducing an immunogenic response that releases substances that trigger systemic anti-tumor effects (abscopal effects).14 There is also a clinical basis, as retrospective series have suggested that radiotherapy has a cytoreductive effect that would induce the delay of systemic therapy through the destruction of subclones of resistant cells. In addition, this would reduce, with better local control, the development of urinary symptomatology12,15 (Table 1).
Evidence on local treatment for primary tumors in mHSPC.
| Study | Treatment and patient characteristics | ResultsHR (95% CI) |
|---|---|---|
| Radiotherapy | ||
| HORRAD16 | ADT+RT (N=216) vs. ADT (N=216)
|
|
| STAMPEDE (H ARM)17,21 | ST (N=1029) vs. ST+RT (N=1032)
|
|
| PEACE-12 | ST (N=296) vs. ST+RT (N=293) vs. ST+abiraterone (N=292) vs. ST+RT+abiraterone (N=291) |
|
| STOPCAP23 | Systematic review and meta-analysisPatients allocated to RT+ADT vs. ADT |
|
| Radical prostatectomy | ||
| APPROACH trial | Phase III, randomized.
| Ongoing |
| SWOG-S1802 trial | Phase III, randomized.
| Ongoing |
mHSPC: metastatic hormone-sensitive prostate cancer; HR: hazard ratio; CI: confidence interval; m: months; PSA: prostate-specific antigen; RT: radiotherapy; OS: overall survival PFS: progression-free survival; ST: standard treatment; ADT: androgen-deprivation therapy.
The HORRAD study was the first clinical trial designed between 2004 and 2014 that randomized 432 patients with mHSPC to ADT±radiotherapy.16 They found no significant difference in OS, but in the subgroup of low-volume patients (n=160, <5metastases), radiotherapy showed a non-statistically significant trend of improvement in OS (HR: 0.68; 95% CI: 0.42–1.10).16
During 2013–2016, the phase III STAMPEDE trial (ARM H) randomly allocated 2,061 patients with de novo mHSPC to standard of care (ADT+docetaxel at 18%) with or without external prostate radiotherapy.17 Radiotherapy improved progression-free survival (PFS) compared to standard treatment (HR: 0.76; 95% CI: 0.68–0.84; p<0.0001) but did not improve OS (HR: 0.92; 0.80–1.06; p=0.266). However, in a prespecified analysis using CHAARTED criteria for tumor volume (high: ≥bone metastases including ≥1metastasis beyond spine or pelvis and/or visceral metastases; low: other than high),18–20 in the low-volume group of patients (n=819), radiotherapy improved 3-year OS compared to standard treatment (81% vs. 73%; HR: 0.68; 0.52–0.90; p=0.007) and PFS (50% vs. 33%; HR: 0.59; 0.49–0.72; p<0.0001), with no significant increase in urinary or bowel toxicity. Patients with high volume did not benefit from local treatment.17
Updated results after a median follow-up of 61.3 months showed that prostate radiotherapy maintained OS benefit in patients with low tumor volume (HR: 0.64; 0.52–0.79; p<0.001), with no benefit in patients with high volume (HR: 1.11; 0.96–1.28; p=0.164).21
The PEACE-1 study is a multicenter phase III trial conducted in 2013-2018. It randomly assigned 1,173 patients with de novo mHSPC (1:1:1:1:1) to standard of care (ADT±docetaxel), standard of care plus radiotherapy, standard of care plus abiraterone, or standard of care plus radiotherapy and abiraterone.2 Patients who received radiotherapy (both in the population with low tumor volume and in the whole population) showed a decrease in the time to onset of serious genitourinary events, regardless of the systemic therapy used. The results of a subanalysis with 505 patients comparing radiotherapy in the low tumor volume subgroup have been presented at ASCO 2023.22 With a median follow-up of 73 months, these patients showed no significant benefit in OS with the addition of radiotherapy, but a significant improvement in radiographic PFS, in the subgroup of patients treated with abiraterone (HR: 0.65; p=0.02). Treatment with radiotherapy prolonged the time to castration resistance, both in the low-volume population (median 3.4 vs. 2.5 years; HR: 0.74; 95% CI: 0.60–0.92; p=0.007) and overall (2.5 vs. 1.9 years; HR: 0.79; 95% CI: 0.69–0.90; p=0.007). The use of a higher radiation dose would justify the differences observed in the results between PEACE-1 and STAMPEDE (74 vs. 67Gy) and a more effective systemic treatment.
The STOPCAP systematic review and meta-analysis (with 2,126 patients from HORRAD, STAMPEDE and PEACE-1) described that prostate radiotherapy was more favorable in patients with low metastatic burden (<5 vs. ≥5metastases; HR: 1.47; 95% CI: 1.11–1.94; p=0.007). There was a 7% improvement in 3-year OS in patients with <5metastases.23
EXPERT RECOMMENDATION: Prostate radiotherapy should be recommended in patients with mHSPC and low tumor volume. Treatment in other subgroups should be individualized and justified by the benefits observed in the reduction of local events.
Radical prostatectomyThere are no data from phase III trials that clarify the role of prostatectomy in de novo mHSPC. Theoretically, the morbidity associated with surgery could have a negative effect on the immune system and cancer control. The series published so far, with limited number of patients, conclude that prostatectomy provides benefits in local control and PFS, being a reproducible technique in carefully selected patients.24
There are two ongoing phase III trials: APPROACH (NCT05649943) and SWOG-S1802 (NCT03678025). The first is a multicenter trial that will enroll 566 patients with oligometastatic HSPC.25 After 6months from the start of treatment with apalutamide, patients will be randomized (1:1) to continue treatment with apalutamide alone or plus a local treatment (according to the investigator’s choice, radiotherapy vs. prostatectomy). SWOG-S1802 is a randomized phase III trial studying the efficacy of standard systemic therapy with or without definitive treatment (cytoreductive prostatectomy or radiotherapy) in patients with metastatic prostate cancer.
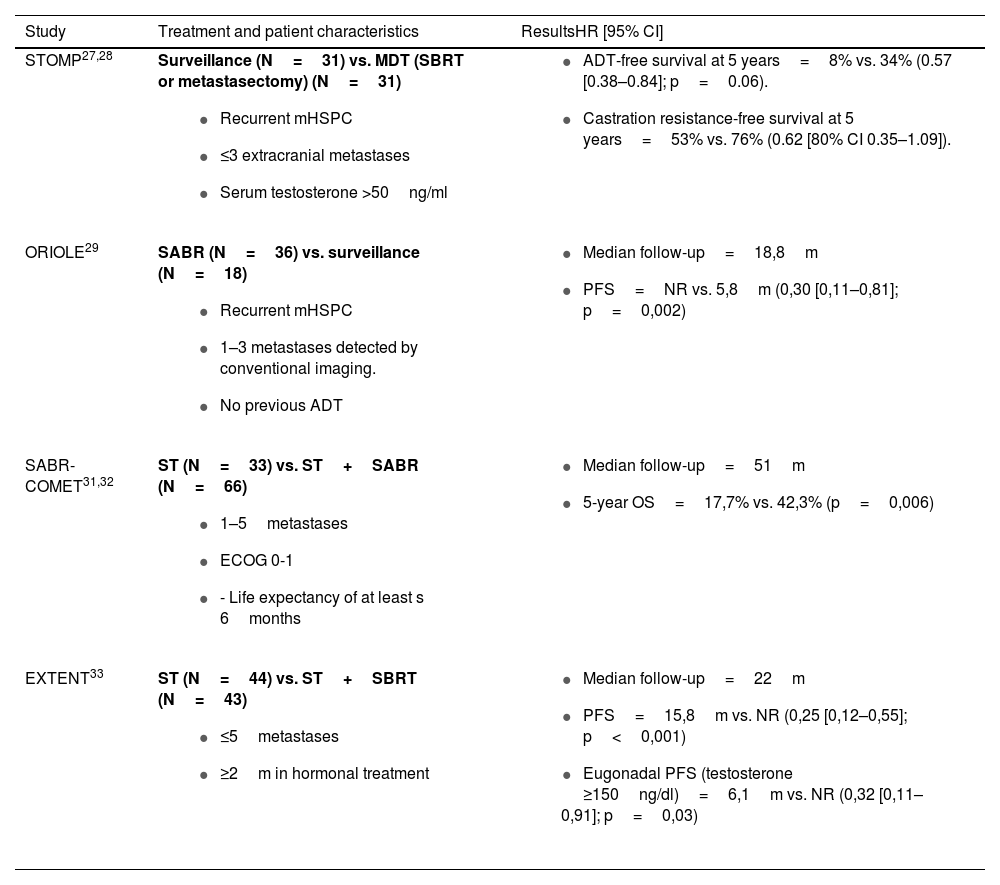
Role of local treatment for oligometastatic disease in mHSPCClinically, metastasis-directed therapy (MDT), commonly by stereotactic body radiotherapy (SBRT or SABR)26 has been shown to improve PFS. The main evidence comes from two phase II trials (STOMP and ORIOLE) that randomized patients with oligometastatic disease (1–3 lesions) to MDT (SBRT in 81% of patients in STOMP and 100% in ORIOLE) or surveillance.27–29 In both trials, MDT delayed the start of ADT (Table 2). The combined data showed that MDT improved PFS (5.9 months for the observation group and 11.9 for the MDT group; HR: 0.44; 95%CI: 0.29–0.66; p<0.001).30 There were no significant differences in radiographic PFS, time to castration resistance or OS.
Evidence on local treatment for oligometastases in mHSPC.
| Study | Treatment and patient characteristics | ResultsHR [95% CI] |
|---|---|---|
| STOMP27,28 | Surveillance (N=31) vs. MDT (SBRT or metastasectomy) (N=31)
|
|
| ORIOLE29 | SABR (N=36) vs. surveillance (N=18)
|
|
| SABR-COMET31,32 | ST (N=33) vs. ST+SABR (N=66)
|
|
| EXTENT33 | ST (N=44) vs. ST+SBRT (N=43)
|
|
mHSPC: metastatic hormone-sensitive prostate cancer; HR: hazard ratio; CI: confidence interval; m: months; NR: not reached; PSA: prostate-specific antigen; SABR: stereotactic ablative radiotherapy; OS: overall survival PFS: progression-free survival; MDT: metastasis directed therapy; ST: standard treatment; ADT: androgen-deprivation therapy.
The phase II, open-label, randomized multitumor SABR-COMET study (18% of patients had prostate cancer) evaluated the effect of SABR in oligometastatic disease (1–5metastases).31,32
Patients were randomly assigned (1:2) to receive standard of care treatment±SABR. With a median follow-up of 51months, the 5-year OS rate was 17.7% in the control group and 42.3% in the SABR group (p=0.006).32 The phase II EXTENT study also evidenced the benefit of MDT in mHSPC, which provided a significant improvement in PFS after a median follow-up of 22months.33
There are currently a number of clinical trials evaluating the use of SBRT in oligometastases in patients receiving standard treatment with new antiandrogens.34–37 Among these is the Spanish phase III START-MET study (NCT05209243),38 which will include 266 patients with mHSPC, with limited disease (≤3 lesions according to CT and bone scintigraphy and ≤5 lesions according to choline PET/CT or PSMA) at diagnosis or at an oligorecurrent stage, and they will be randomly assigned (1: 1) to standard of care treatment+SBRT (for all lesions) vs. standard of care treatment.
EXPERT RECOMMENDATIONS: Pending the results of randomized trials, treatment with MDT (and more specifically SBRT) in oligometastatic disease seems to be an individualized option in well-informed patients and within the framework of multidisciplinary committees.
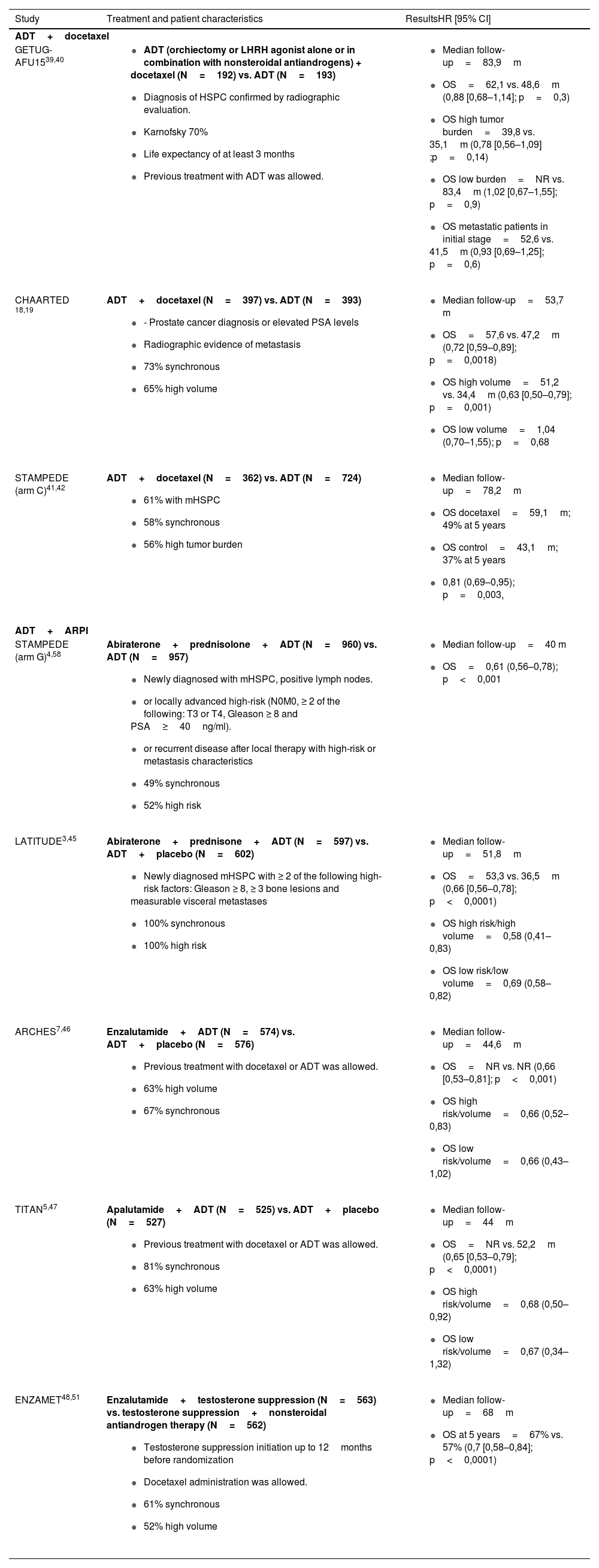
Review of doublet activityADT plus docetaxel: Doublet TherapyDocetaxel improves survival when combined with ADT vs. ADT monotherapy.18,19,39–42 Although the GETUG-AFU study15 was negative for OS,39,40 probably due to the greater number of low-volume patients, the CHAARTED study18,19 and STAMPEDE ARM C41,42 obtained positive results in terms of OS (Table 3). According to CHAARTED, the improvement was more pronounced in high-volume patients.18,43 However, disease volume did not affect OS benefit in STAMPEDE when adding docetaxel to ADT,41,42 probably because STAMPEDE included more low-volume patients than CHAARTED (44% vs. 35%). Several meta-analyses have shown that the benefit of docetaxel is greater in synchronous, high-volume disease.18,19,44
Evidence on the use of doublets in mHSPC.
| Study | Treatment and patient characteristics | ResultsHR [95% CI] |
|---|---|---|
| ADT+docetaxel | ||
| GETUG-AFU1539,40 |
|
|
| CHAARTED 18,19 | ADT+docetaxel (N=397) vs. ADT (N=393)
|
|
| STAMPEDE (arm C)41,42 | ADT+docetaxel (N=362) vs. ADT (N=724)
|
|
| ADT+ARPI | ||
| STAMPEDE (arm G)4,58 | Abiraterone+prednisolone+ADT (N=960) vs. ADT (N=957)
|
|
| LATITUDE3,45 | Abiraterone+prednisone+ADT (N=597) vs. ADT+placebo (N=602)
|
|
| ARCHES7,46 | Enzalutamide+ADT (N=574) vs. ADT+placebo (N=576)
|
|
| TITAN5,47 | Apalutamide+ADT (N=525) vs. ADT+placebo (N=527)
|
|
| ENZAMET48,51 | Enzalutamide+testosterone suppression (N=563) vs. testosterone suppression+nonsteroidal antiandrogen therapy (N=562)
|
|
mHSPC: metastatic hormone-sensitive prostate cancer; HR: hazard ratio; CI: confidence interval ARPI: androgen receptor pathway inhibitor; m: months; NR: not reached; PSA: prostate-specific antigen OS: overall survival; ADT: androgen deprivation therapy.
ARM G of the STAMPEDE study compared the combination of abiraterone with prednisolone and ADT vs. ADT alone, showing an improvement in 5-year OS of up to 60%, compared to 41% in ADT.4 Similarly, in the LATITUDE trial, which included only patients with synchronous, high-risk metastases (defined as two of the three of the following factors: ≥8 Gleason score, ≥3 bone lesions, and the presence of visceral metastasis). The median OS was 53.3 months in males with high-risk de novo mHSPC treated with abiraterone and prednisone, vs. 36.5months in the ADT group.45 Apalutamide and enzalutamide have also confirmed the benefit of the doublet over ADT monotherapy in terms of time to castration resistance, PFS46 and OS.47,48Table 3 summarizes the studies on the combination of ADT with ARPI vs. ADT alone.
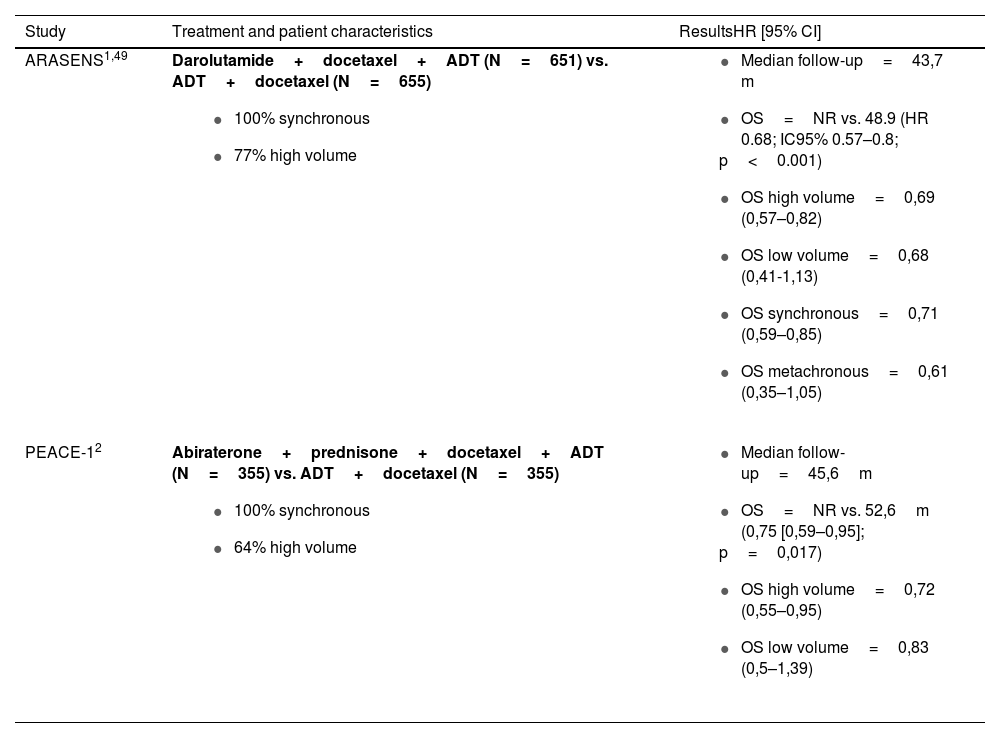
Triplet therapy with ADT+docetaxel+ARPI: Evidence ReviewTwo randomized phase III studies (PEACE-12 and ARASENS1,49) have demonstrated the superiority of triplet therapy over doublet therapy with ADT plus docetaxel (patient characteristics and results in Table 4). Of these, ARASENS is the only study designed from the outset to answer whether adding an ARPI improves the results of doublet therapy with docetaxel.
Evidence on the use of triplets in mHSPC.
| Study | Treatment and patient characteristics | ResultsHR [95% CI] |
|---|---|---|
| ARASENS1,49 | Darolutamide+docetaxel+ADT (N=651) vs. ADT+docetaxel (N=655)
|
|
| PEACE-12 | Abiraterone+prednisone+docetaxel+ADT (N=355) vs. ADT+docetaxel (N=355)
|
|
mHSPC: metastatic hormone-sensitive prostate cancer; HR: hazard ratio; CI: confidence interval m: months; NR: not reached: OS: overall survival; ADT: androgen deprivation therapy.
The primary endpoint of the PEACE-1 study was to evaluate the role of local treatment plus systemic therapy intensification with abiraterone. As recruitment was extended, the standard treatment, which initially consisted of ADT alone, shifted to ADT+docetaxel following a protocol modification. Triplet therapy improved OS compared to docetaxel and ADT, with a greater benefit in high-volume patients.2
A subanalysis of the PEACE-1 study evaluated the effect of the triplet in patients aged ≥70 years compared to younger patients.50 The older patients had a worse performance status (ECOG 1-2) and hypertension and type 2 diabetes mellitus were more frequent. The results suggested that the older population derives less benefit in terms of radiographic PFS and OS, possibly due to more toxicity leading to more frequent drug discontinuation, since in older patients fit enough to receive ADT+docetaxel, the benefit of adding abiraterone to standard treatment was comparable to that obtained in younger patients.50
The only registry trial published so far with a triplet therapy is ARASENS, which randomly assigned 1,306 patients with synchronous and metachronous (1:1) mHSPC to ADT+docetaxel+darolutamide or placebo.1,49 The triplet therapy was again associated with improved OS (global and in all patient subgroups) compared to the control group but was superior in patients with synchronous and high-volume disease. As an additional note, the majority of patients in this study received therapies that prolong progression-free survival, again confirming that a sequential treatment is inferior to an upfront intensification. In the long term, there was no deleterious effect on the quality of life of patients treated with darolutamide and no unexpected adverse events were observed.
EXPERT RECOMMENDATIONS: Patients who are candidates for docetaxel should not receive doublet therapy with docetaxel alone. The combination with darolutamide is the only one available according to the data sheet, based on a specific trial to demonstrate superiority over docetaxel. The combination with abiraterone is a valid alternative in those patients in whom triplet therapy with darolutamide cannot be administered and individualized according to comorbidities and potential toxicities.
Indirect comparisons between doublet and triplet therapies: Evidence ReviewThe ARCHES, TITAN and ENZAMET trials included a small number of patients who received sequential triplet therapy with docetaxel. In the first two, docetaxel was administered to 18% and 11%, respectively, and secondary analyses did not find an OS benefit with the triplet, probably due to the low number of patients.5,7,46,47 However, in the ENZAMET study (45% of patients received triplet therapy plus docetaxel) the results suggested that the triplet increased PFS at the expense of increased toxicity.48,51
Several systematic reviews and meta-analyses have made indirect comparisons between ADT plus ARPI plus docetaxel vs. ADT plus ARPI.52–57 In this regard, in the general population, most analyses have shown that PFS and OS were superior with the triplet than with ADT plus docetaxel5,7,46,47,53,54,56,57; however, the triplet is not superior when compared with ADT plus ARPI.52,53,55,56 Regarding subgroup analysis, OS was superior with the triplet vs. ADT plus docetaxel only in high-volume and synchronous patients.53,56 In low-volume patients, the triplet did not show a significant benefit compared to ADT plus docetaxel, and would even be unfavorable compared to ADT plus ARPI.57 Toxicity results were highly variable from one analysis to another, ranging from no differences to an increase in grade 3 toxicity with the triplets, especially in terms of arterial hypertension with abiraterone and darolutamide.52,57
EXPERT RECOMMENDATIONS: Triplet therapy could be considered for patients with metastatic disease and high tumor volume, especially de novo and without contraindications to docetaxel. Patients who are not candidates for treatment with docetaxel should receive a doublet of ADT plus ARPI. Doublet with docetaxel is not considered. ADT monotherapy should be limited to patients with significant comorbidities and who may not benefit from medium-term intensification.
ConclusionsThe therapeutic landscape of mHSPC has rapidly evolved, outpacing treatment with ADT monotherapy and ADT plus docetaxel. Advances are outlined by the incorporation of local radiotherapy in metastatic disease and evidence of the synergistic effect from the concomitant use of the different treatments. The choice of a triplet over a doublet therapy with ARPI cannot be based on the results of a direct trial. Certain criteria proposed for its selection are tolerance to docetaxel treatment, disease volume and metastatic timing. Although these criteria are still under way, we should look for individualized treatment strategies based on gene panels and biomarkers.
FundingThis work has been funded by Bayer in accordance with the Good Publication Practice guidelines (GPP-2022).
Conflicts of interestÁngel Borque-Fernando has participated in training sessions and received consulting fees from Asofarma, Astellas-Pharma, AstraZeneca, Bayer, GP Pharm, HealthMDx, Ipsen, Janssen, Lacer, MSD, Pharmalink and Recordati.
Almudena Zapatero has received lecture, consulting, research, and other non-financial support from Astellas-Pharma and Janssen.
Ray Manneh has received lecture, consulting and research fees from AstraZeneca, Amgen, Astellas-Pharma, Bayer, BMS, Eli Lilly, Ipsen, Jannsen, MSD, Merck Serono, Novartis, Pfizer, Roche and Tecnofarma.
Teresa Alonso-Gordoa has received honoraria for lectures, consulting, research, and other non-financial support from IPSEN, Eli Lilly, Adacap, Pfizer, Sanofi, EISAI, Bayer, Janssen, Astellas-Pharma, Novartis, and MSD.
Felipe Couñago has received honoraria from Janssen, Astellas, IPSEN, Recordati, Boston Scientific, AstraZeneca, and Bayer for participation in expert committees and conferences.
Mario Domínguez has received honoraria from Janssen, Astellas, IPSEN, Bristol, AAA, Boston Scientific, Intuitive, AstraZeneca and Bayer for his participation in expert committees and conferences.
Marta López Valcárcel has received honoraria for lectures, consulting, research, and other non-financial support from Astellas-Pharma, Janssen, Bayer, Recordati and MSD.
Alfredo Rodríguez Antolín has received fees for his participation in training and consulting sessions from Astellas-Pharma, AstraZeneca, Novartis, Bayer and Janssen.
Nuria Sala González: has received research grants, honoraria, and other non-financial support from IPSEN Pfizer, Bayer, BMS and MSD.
Noelia Sanmamed has received consulting fees from Astellas-Pharma.
Pablo Maroto has received fees for lectures, consulting, and other support such as logistic support from Astellas, Janssen, Bayer, MSD, and Novartis.
The authors would like to express their gratitude to Fernando Sánchez Barbero PhD, on behalf of Springer Healthcare, for editorial support and assistance in drafting the manuscript.