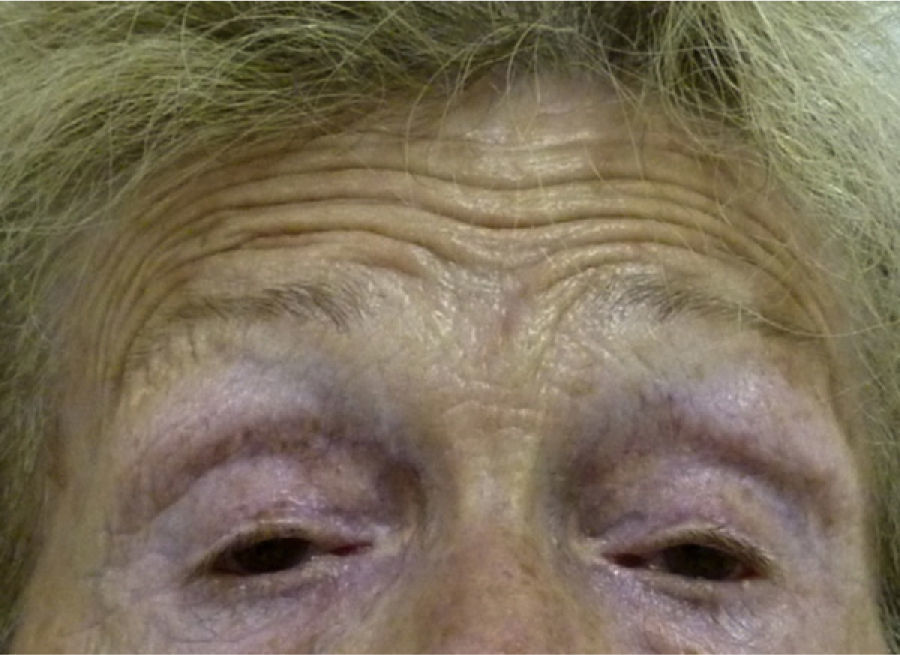
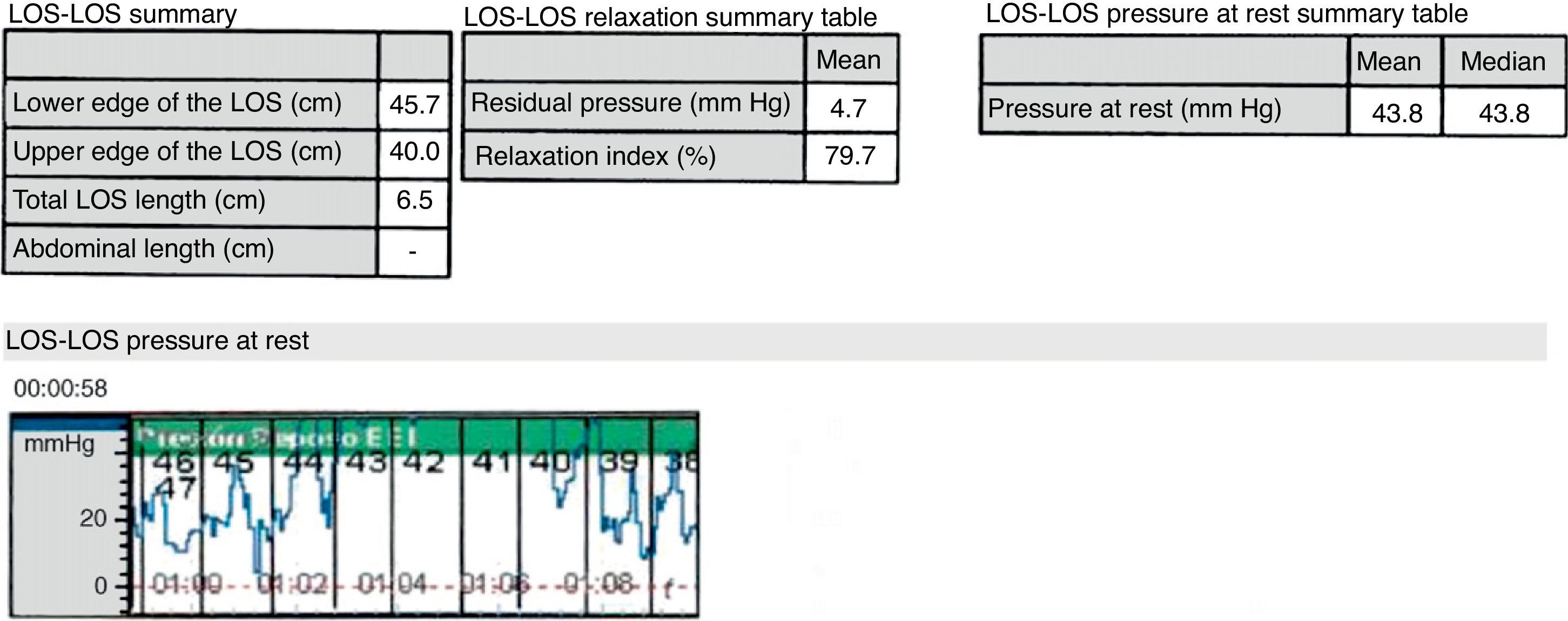
Oculopharyngeal muscular dystrophy is an infrequent, not widely known entity. Of genetic origin, it usually shows up in the 5th or 6th decade of life. Most cases are referred directly to the gastroenterologist by their general practitioner and not to the otolaryngologist, so it is essential to be aware of this disease to suspect it. We report a case diagnosed and treated in our hospital and we review the literature.
La distrofia muscular óculo-faríngea es una entidad infrecuente y poco conocida, genéticamente determinada, que suele presentarse en la 5.a o 6.a década de la vida. Casi siempre estos pacientes son remitidos directamente al digestólogo desde su médico de familia y no con tanta frecuencia al otorrinolaringólogo, por lo que el conocimiento de esta enfermedad es fundamental para sospecharla. Presentamos un caso diagnosticado y tratado en nuestro hospital y revisamos la literatura al respecto.